Abstract
Purpose
To analyze the impact of the coronavirus disease (COVID) pandemic on emergency department (ED) computed tomography (CT) utilization.
Methods
A retrospective observational study was conducted assessing seven hospitals’ ED imaging volumes between Jan. 6, 2019, and Feb. 27, 2021. Weekly CT utilization is reported as CTs ordered per 100 ED visits. Utilization was ascertained in aggregate and by body area. Interrupted time series analysis was performed to assess significance of utilization change. Prespecified sensitivity analysis was performed for influenza-like or COVID-like illness (ILI/CLI).
Results
Weekly ED CT utilization increased from 35.9 CTs per 100 visits (95% confidence interval [95% CI] 35.8–36.1) to 41.8 per 100 visits (95% CI 41.7–42.0) in pre- and post-pandemic periods. Weekly ED CT chest utilization increased immediately following the pandemic declaration (+ 0.52 chest CTs per 100 ED visits, 95% CI 0.01–1.03, p < 0.05) and compared to pre-pandemic period (+ 0.02 per 100 ED visits, 95% CI 0.02–0.05, p < 0.02). For both CT abdomen/pelvis and CT head, there was neither an immediate effect (+ 0.34 CT-AP per 100 ED visits, 95% CI − 0.74 to 1.44, p = 0.89; − 0.42 CT-H per 100 ED visits, 95% CI − 1.53 to 0.70, p = 0.46) nor a change in weekly CT utilization (+ 0.03 CT-AP per 100 ED visits, 95% CI − 0.01 to 0.05, p = 0.09; + 0.03 CT-H per 100 ED visits, 95% CI − 0.01 to 0.06, p = 0.10).
Conclusion
These data may help formulate future strategies for resource utilization and imaging operations as we envision a future with COVID and other federal mandates affecting imaging utilization and appropriateness.
Similar content being viewed by others
Introduction
The COVID pandemic resulted in a significant impact on most aspects of the US healthcare system. Since the World Health Organization (WHO) first declared COVID a global pandemic on March 11, 2020 [1], US federal and state policies and procedures have been implemented in an attempt to limit the spread and impact of this pandemic [2, 3]. To reduce the risk of COVID-19 transmission, hospitals, health systems, and medical societies recommended the cancellation or postponement of nonurgent medical procedures and imaging services. These restrictions, in conjunction with local “stay at home” orders, resulted in a significant decline in hospital-based healthcare services across the globe, including imaging and emergency services [4,5,6]. ED patient visit volumes decreased 40–75% [7,8,9], and ED imaging volumes decreased by 28–58% [10,11,12,13,14]. While some proportion of the decreased healthcare utilization is thought to be deferral of elective care [15], a number of studies have also found visits for emergent conditions, such as ST-elevation myocardial infarction and stroke also decreased in the early pandemic [16,17,18,19,20].
Prior to COVID, national ED visit volumes had been increasing annually at rates higher than anticipated based on population growth, with a 10-year volume changes up as much as 32% and a 20-year volume changes up to 57% [21, 22]. ED CT utilization (number of CT studies per 100 ED visits [23]) was similarly increasing [21, 24, 25] up 33% (from 18 to 24 imaging studies per 100 ED visits [years 2005–2019]). This rise in imaging may be because CT-based diagnosis can improve patient outcomes and overall resource utilization [26, 27].
With the background of CT utilization increasing, several studies have evaluated patterns of CT use during the COVID pandemic, finding a decline in the absolute number of CT orders [10, 15, 28,29,30,31]. These decreases have been attributed to decreased imaging of lower acuity patients [10]; however, the data are difficult to interpret given that EDs nationwide experienced a nearly 40% reduction in visit volumes during the early COVID pandemic [7, 32]. Looking more specifically at CT chest utilization in the pandemic context, one prior study analyzing data in a single health system during the first 3 months of the pandemic noted a significant increase in CT chest utilization, despite a 46% drop in overall CT utilization; however, these data were not analyzed relative to the dynamic changes in ED volume [30]. CT chest imaging may have increased because early studies suggested that CT chest imaging can improve diagnostic accuracy when added to molecular testing for COVID [33, 34] as well as an increased risk for thromboembolic disease in patients with COVID [35].
In the setting of previously rising ED volumes and CT utilization, it remains to be seen how the impact of the COVID pandemic on ED volumes and resource utilization will affect ED clinician’s decision making practices and imaging utilization going forward. Prior researchers have called for further studies demonstrating how the pandemic has affected imaging utilization and ordering practices [30].
The purpose of this study was to describe CT utilization in the ED setting since the start of the global pandemic across a single health system. These data will add to the body of literature detailing the influence of COVID-19 on CT utilization which, in turn, may aid others in predictions and institutional preparedness efforts for the current pandemic as well as future states.
Methods
Study design
This was a retrospective time series analysis of ED visits and imaging volumes in one large Midwestern academic health system from January 6, 2019, to February 27, 2021. The health system is the largest integrated academic health system in Illinois with a cumulative volume of 400,000 annual ED visits in fiscal year 2019. The current study includes seven EDs across five counties, including one super high-volume urban academic tertiary care center.
Data collection and extraction
Aggregated imaging volume data and ED operational data were abstracted from the electronic data warehouse (EDW) using structured query language. Weekly volume data for total CT imaging studies as well as the total subcategorized by body area (CTs of the brain, abdomen/pelvis, and chest) were collected from seven of the EDs in the health system over the study period.
Statistical analysis
We tabulated the weekly number of CT scans ordered during ED visits from 1/6/19 to 2/27/21 to compare CT utilization trends before and after the onset of the COVID pandemic. Due to known substantial declines in ED visit volumes during the pandemic, we standardized weekly CT utilization by the total ED visit volumes in order to present adjusted CTs ordered per 100 ED visits [21].
We then evaluated weekly CT utilization trends using single group interrupted time series analyses with ordinary least squares regression and Newey-West standard errors, adjusting for the following a priori selected covariates: median age and ED length of stay and proportion of ED visits of female sex and admitted to the hospital. After selecting lag intervals based on Cumby-Huizinga tests for autocorrelation, we set the intervention time as the week beginning on 3/8/20 to capture the WHO pandemic declaration issued on 3/11/20 (week 62) [1]. We considered the pandemic to have a significant effect on adjusted CT utilization if either the immediate effect coefficient or the change in post-intervention trend over time was significant at p < 0.05. Our primary focus was on the utilization of CT chest orders, but we performed the same interrupted time series analyses for CT abdomen/pelvis and CT head orders for comparative purposes. All statistical analyses were performed in Stata v14.2 (StataCorp, College Station, TX) using the itsa and actest packages.
To confirm the robustness of our results, we conducted a sensitivity analysis evaluating only CT utilization among ED visits with an influenza-like or COVID-like illness, defined by a system-wide infectious disease screening protocol for symptoms of fever with cough or shortness of breath, or the presence of a COVID-19 diagnosis.
This retrospective observational study was approved by the Institutional Review Board at our institution. The need to obtain informed consent was waived. Aggregate data on ED demand and CT utilization from the health system were pooled without individual patient level identification. We adhered to the STROBE reporting guidelines.
Results
There were 618, 972 ED visits and 237, 053 CTs obtained during the 112 week-long study period. Mean ED visit volumes decreased from 6,063 visits/week in the pre-pandemic period to 4,885 visits/week in the pandemic period. The first COVID diagnosis in the health system was the week of 3/1/20, followed by a sharp weekly increase into bimodal peaks of 449 and 780 weekly COVID-19 diagnoses during the weeks of 4/19/20 and 11/8/20, respectively. ED visits in the pandemic period were older (44.4 years vs 40.6 years, p < 0.001), less likely to be female (55.0 vs 55.6%, p < 0.001), and had a higher admission rate (22.7% vs 20.4%, p < 0.001) than those in the pre-pandemic period. The median ED lengths of stay were similar (3.2 vs 3.4 h, p = 0.08).
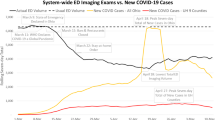
Weekly ED CT utilization increased from a mean of 35.9 CTs per 100 visits (95% confidence interval [95% CI] 35.8–36.1) in the pre-pandemic period to 41.8 CTs per 100 visits (95% CI 41.7–42.0) in the post-pandemic period. Figure 1 displays the weekly adjusted ED CT utilization and COVID-19 diagnoses.
CT utilization and COVID + cases over time. CT utilization, defined as number of CTs ordered per 100 visits, is plotted in blue. The number of COVID + cases per 100 ED visits is plotted on the secondary y axis on the dotted line. Weekly adjusted ED CT utilization increased from 35.9 CTs per 100 visits (35.8–36.1) in pre-pandemic to 41.8 CTs per 100 visits (41.7–42.0) in post-pandemic period
Figure 2 displays the interrupted time series analysis of weekly ED CT chest utilization, adjusted for age, sex, admit rate, and ED length of stay. Prior to the pandemic declaration during the week of 3/8/20 (week 62), there was no significant change in the weekly ED CT chest utilization of 4.4 CTs per 100 ED visits (p = 0.15). In the first week following the pandemic declaration, there was an immediate significant increase in ED CT chest utilization (+ 0.52 chest CTs per 100 ED visits, 95% CI 0.01–1.03, p < 0.05) and a significant increase in the pandemic weekly rate of ED CT chest utilization compared to the pre-pandemic period (+ 0.02 chest CTs per 100 ED visits, 95% CI 0.02–0.05, p < 0.02). The mean weekly ED CT chest utilization reached a bimodal peak during the post-pandemic period of 7.05 and 8.56 CTs per 100 ED visits during the weeks of 4/19/20 and 11/15/20, respectively, coinciding with bimodal peaks in COVID-positive cases (Fig. 1).
Interrupted time series analysis of weekly CT chest utilization per 100 ED visits. Weekly ED CT chest utilization adjusted for sex, age, admit rate, and ED length of stay. Prior to the pandemic declaration during the week of 3/8/20 (Week 62), there was no significant change in the weekly ED CT chest utilization. In the first week following the pandemic declaration, there was an immediate significant increase in ED CT chest utilization (+ 0.52 chest CTs per 100 ED visits, 95% CI 0.01–1.03, p < 0.05) and a significant increase in the pandemic weekly rate of ED CT chest utilization compared to the pre-pandemic period (+ 0.02 chest CTs per 100 ED visits, 95% CI 0.02–0.05, p < 0.02). Mean weekly ED CT chest utilization reached a bimodal peak during the post-pandemic period of 7.05 and 8.56 CTs per 100 ED visits during the weeks of 4/19/20 and 11/15/20, respectively
Interrupted time series analyses for CT abdomen/pelvis and CT head utilization are presented in eFigs. 1 and 2. For both CT abdomen/pelvis and CT head, there was neither an immediate effect following the pandemic declaration (+ 0.34 CT-AP per 100 ED visits, 95% CI − 0.74 to 1.44, p = 0.89; − 0.42 CT-H per 100 ED visits, 95% CI − 1.53 to 0.70, p = 0.46) nor a change in the post-pandemic weekly rate of CT utilization compared to the pre-pandemic period (+ 0.03 CT-AP per 100 ED visits, 95% CI − 0.01 to 0.05, p = 0.09; + 0.03 CT-H per 100 ED visits, 95% CI − 0.01 to 0.06, p = 0.10).
We found similar findings in the sensitivity analysis of only those ED visits for whom an influenza-like or COVID-like illness (ILI/CLI) was suspected (i.e., fever with cough or shortness of breath). Prior to the pandemic declaration (Fig. 3), there was no significant change in the weekly ED CT chest utilization rate of 4.4 CTs per 100 ED visits (p = 0.29). In the first week following the pandemic declaration, there was an immediate significant increase in ED CT chest utilization (+ 0.77 chest CTs per 100 ED visits, 95% CI 0.14–1.40, p-0.02), and in the following weeks, there was a significant increase in the pandemic weekly rate of ED CT chest utilization compared to the pre-pandemic period (+ 0.04 chest CTs per 100 ED visits, 95% CI 0.02–0.06, p < 0.0001). Although weekly CT chest utilization in this sensitivity analysis cohort reached bimodal peaks coinciding with the trends observed in the main analysis (Fig. 3; 5.45 and 7.64 CTs per 100 ED visits during the weeks of 4/19/20 and 11/15/20, respectively), CT utilization notably decreased in the weeks between these bimodal peaks to a level below that of the pre-pandemic rate (nadir 2.68 CTs per 100 ED visits on 8/30/20).
Interrupted time series analysis of weekly CT chest utilization per 100 ED visits among ED visits suspected to have influenza-like or COVID-like illness. In the first week following the pandemic declaration (week 62), there was an immediate significant increase in ED CT chest utilization (+ 0.77 chest CTs per 100 ED visits, 95% CI 0.14–1.40, p-0.02), and in the following weeks, there was a significant increase in the pandemic weekly rate of ED CT chest utilization compared to the pre-pandemic period (+ 0.04 chest CTs per 100 ED visits, 95% CI 0.02–0.06, p < 0.0001). Although weekly CT chest utilization in this sensitivity analysis cohort reached bimodal peaks coinciding with the trends observed in the main analysis (Fig. 3; 5.45 and 7.64 CTs per 100 ED visits during the weeks of 4/19/20 and 11/15/20, respectively), CT utilization notably decreased in the weeks between these bimodal peaks to a level below that of the pre-pandemic rate (nadir 2.68 CTs per 100 ED visits on 8/30/20)
Discussion
Compared to pre-pandemic baseline, there was a significant increase in rates of both overall ED CT utilization and ED CT chest utilization following the start of the COVID pandemic. The collateral effect of the COVID pandemic on healthcare utilization, including its effect on ED visit number and severity of disease as well as need for advanced diagnostic imaging, has been a concern for emergency physicians throughout the stages of the pandemic. Our study found an increase in overall ED CT utilization rates following the start of the COVID pandemic, which contrasts to prior studies looking at the absolute number of imaging studies (rather than imaging rates) that demonstrated decreased overall imaging volumes [10,11,12,13,14]. Despite the decreased ED patient arrivals resulting from the onset of the COVID pandemic, CT utilization per 100 visits increased in our study. Our data, therefore, argue against theories that ordering clinicians may have changed behavior with a more conservative utilization of diagnostic imaging services [15]. In contrast, it is possible that the increased CT use may reflect additional factors such as local practice patterns (which contributed to the pre-pandemic CT utilization of 35.9/100 ED visits), as well as rising patient acuity, admission rates, and patient age may all have contributed [36,37,38].
When evaluating ED CT chest utilization specifically, our data show a significant increase in ED CT chest utilization following the start of the COVID pandemic compared to historical control time period. The CT chest utilization increase aligns with prior research [30] and is likely attributable to the increase in respiratory-related ED visits as well as CT chest’s utility in the diagnostic evaluation and prognostic assessment of COVID-19 and its associated complications [35, 39, 40]. We did not identify any significant immediate changes in CT abdomen/pelvis or CT brain utilization. However, there were continued nonsignificant increases in both exam types from the pre-pandemic to pandemic timeframes. It is possible that some component of these increases represents the continuation of historical trends that predated the pandemic, such as our local health system ED CT utilization and local practice patterns. Other factors contributing to the increase may be that delayed and deferred care related to the pandemic may have led to an increased need for advanced imaging as patients presented later with worsened clinical conditions [36,37,38].
The sensitivity analysis of only those ILI/CLI-related ED visits found similar results to our overall study population. Although weekly CT chest utilization in the sensitivity analysis cohort reached bimodal peaks coinciding with the trends observed in the main analysis (Fig. 3; 5.45 and 7.64 CTs per 100 ED visits during the weeks of 4/19/20 and 11/15/20, respectively), CT utilization notably decreased in the weeks between these bimodal peaks to a level below that of the pre-pandemic rate (nadir 2.68 CTs per 100 ED visits on 8/30/20). Factors contributing to this dip in ED CT chest utilization below pre-pandemic baseline are likely the increased availability of diagnostic testing (rapid antigen or PCR-based) as well as awareness of and confidence in the diagnostic test characteristics of molecular testing. Additional contributing factors may have been patient- or disease-specific, including symptom severity, clinical course of a specific SARS-CoV2 variant, and location of healthcare utilization for patients with ILI/CLI symptoms. The subsequent increase in ED CT chest utilization corresponding to a second COVID wave may have been related to an increase in symptom severity and increased awareness and risk for various comorbid conditions, as well as utility of CT chest in both diagnosis and prognostic assessment of suspected COVID and the exclusion of related conditions (e.g., pulmonary embolism) [34, 35, 39,40,41,42].
These data add a more detailed understanding of how CT imaging use has evolved during this crisis, which is particularly important as we consider a future state during which clinicians will be required to consult tools to determine appropriateness of select high impact imaging studies [43]. EDs are currently encountering a large volume of patients with a relatively new disease process, one in which investigations are ongoing regarding how to best incorporate CT chest into an appropriate and evidence-based diagnostic evaluation, and for which clinical practice guidelines are yet to be developed [39]. This dynamic environment may inadvertently result in imaging being deemed inappropriate, impacting institutional compliance and performance relative to any relevant future mandates.
This study has several limitations. It is a retrospective design, which limits our analysis to correlation only. The study was conducted in a single health system and, however, included a large variety of ED types, volumes, and locations. One may note that the pre-pandemic ED CT utilization in our health system (35.9/100 ED visits) is well above national average across all types of EDs. However, this ED CT utilization is similar compared to like institutions, including only adult EDs (32/100), those with 80 k–100 k annual ED visits (32/100), and level 1 or 2 trauma centers (31/100) [21]. Additionally, the local medicolegal environment in Illinois as well as concerns regarding diagnostic accuracy likely contribute to increased ED diagnostic test utilization [44, 45]. An additional limitation is that our analysis focuses on presentation to the ED and is not able to capture those patients who may have been evaluated in the outpatient setting by primary care or other providers as well as may have sought evaluation in private outpatient only radiology centers, both of which could have provided a perception of safer, less risky care.
Conclusion
These data may help formulate future operational strategies for resource utilization and imaging indications as we look towards a future with endemic or annual COVID-19 seasons. Further, the dynamic changes in utilization highlight future challenges in universally applying appropriateness criteria to emergency imaging in the setting of a global pandemic or emerging disease process.
References
Ghebreyesus T (2020) World Health Organization (WHO) Director-General’s opening remarks at the media briefing on COVID-19. 11 March 2020. https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---20-march-2020. Accessed 1 May 2021
Azar A (2020) US Department of Health and Human Services - Determination that a public health emergency exists - Jan 31, 2020. https://www.phe.gov/emergency/news/healthactions/phe/Pages/2019-nCoV.aspx. Accessed 15 May 2021
Pritzker JB (2020) Gubernatorial disaster proclamation regarding COVID-19 - March 9,2020. https://www.illinois.gov/content/dam/soi/en/web/illinois/documents/government/coronavirus-disaster-proc-12-10-2021.pdf. Accessed 15 May 2021
Cohen BA, Wessling EG, Serina PT, Cruz DS, Kim HS, McCarthy DM, Loftus TM (2021) Emergency department operations in a large health system during COVID-19. Am J Emerg Med 41:241–243. https://doi.org/10.1016/j.ajem.2020.05.097
Barten DG, Latten GHP, van Osch FHM (2022) Reduced emergency department utilization during the early phase of the COVID-19 pandemic: viral fear or lockdown effect? Disaster Med Public Health Prep 16(1):6–39. https://doi.org/10.1017/dmp.2020.303
Wongtanasarasin W, Srisawang T, Yothiya W, Phinyo P (2021) Impact of national lockdown towards emergency department visits and admission rates during the COVID-19 pandemic in Thailand: a hospital-based study. Emerg Med Australas 33:316–323. https://doi.org/10.1111/1742-6723.13666
Hartnett KP, Kite-Powell A, DeVies J, Coletta MA, Boehmer TK, Adjemian J, Gundlapalli AV(2020) Impact of the COVID-19 pandemic on emergency department visits - United States, January 1, 2019-May 30, 2020. MMWR Morb Mortal Wkly Rep 69:699–704. https://doi.org/10.15585/mmwr.mm6923e1
DeLaroche AM, Rodean J, Aronson PL, Fleegler EW, Florin TA, Goyal M, Hirsch AW, Jain S, Kornblith AE, Sills MR, Wells JM, Neuman MI (2021) Pediatric emergency department visits at US children’s hospitals during the COVID-19 pandemic. Pediatrics 147(4):e20203968. https://doi.org/10.1542/peds.2020-039628
Haddadin Z, Blozinski A, Fernandez K et al (2021) Changes in pediatric emergency department visits during the COVID-19 pandemic. Hosp Pediatr 11:e57–e60. https://doi.org/10.1542/hpeds.2020-005074
Gibson AL, Chen BY, Rosen MP, Paez SN, Lo HS (2020) Impact of the COVID-19 pandemic on emergency department CT for suspected diverticulitis. Emerg Radiol 27:773–780. https://doi.org/10.1007/s10140-020-01865-3
Naidich JJ, Boltyenkov A, Wang JJ, Chusid J, Hughes D, Sanelli PC (2020) Impact of the coronavirus disease 2019 (COVID-19) pandemic on imaging case volumes. J Am Coll Radiol 17:865–872. https://doi.org/10.1016/j.jacr.2020.05.004
Naidich JJ, Boltyenkov A, Wang JJ, Chusid J, Hughes D, Sanelli PC (2020) Coronavirus disease 2019 (COVID-19) pandemic shifts inpatient imaging utilization. J Am Coll Radiol 17:1289–1298. https://doi.org/10.1016/j.jacr.2020.06.011
Cavallo JJ, Forman HP (2020) The economic impact of the COVID-19 pandemic on radiology practices. Radiology 296:E141–E144. https://doi.org/10.1148/radiol.2020201495
Messina MD, Stein MW, Armstrong IJ, Wolf EL (2021) Impact of the COVID-19 pandemic on radiology department emergency ultrasound utilization. Emerg Radiol 28(5):69–875. https://doi.org/10.1007/s10140-021-01936-z
Agarwal M, Udare A, Alabousi A, van der Pol CB, Ramonas L, Mascola K, Edmonds B, Ramonas M (2020) Impact of the COVID-19 pandemic on emergency CT head utilization in Ontario-an observational study of tertiary academic hospitals. Emerg Radiol 27:791–797. https://doi.org/10.1007/s10140-020-01857-3
Kansagra AP, Goyal MS, Hamilton S, Albers GW (2020) Collateral effect of Covid-19 on stroke evaluation in the United States. N Engl J Med 383:400–401. https://doi.org/10.1056/NEJMc2014816
Lange SJ, Ritchey MD, Goodman AB et al (2020) Potential indirect effects of the COVID-19 pandemic on use of emergency departments for acute life-threatening conditions - United States, January-May 2020. MMWR Morb Mortal Wkly Rep 69:795–800. https://doi.org/10.15585/mmwr.mm6925e2
Garcia S, Albaghdadi MS, Meraj PM, Schmidt C, Garberich R, Jaffer FA, Dixon S, Rade JJ, Tannenbaum M, Chambers J, Huang PP, Henry TD (2020) Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol 75:2871–2872. https://doi.org/10.1016/j.jacc.2020.04.011
Bres Bullrich M, Fridman S, Mandzia JL, Mai LM, Khaw A, Vargas Gonzalez JC, Bagur R, Sposato LA (2020) COVID-19: stroke admissions, emergency department visits, and prevention clinic referrals. Can J Neurol Sci Le J Can Des Sci Neurol 47:693–696. https://doi.org/10.1017/cjn.2020.101
Kim HS, Cruz DS, Conrardy MJ, Gandhi KR, Seltzer JA, Loftus TM, Fant AL, McCarthy DM (2020) Emergency department visits for serious diagnoses during the COVID-19 pandemic. Acad Emerg Med 27:910–913. https://doi.org/10.1111/acem.14099
Emergency Department Benchmarking Alliance (EDBA) (2020) Before there was COVID: 2019 ED performance measures report. https://www.edbenchmarking.org/. Accessed 1 July 2021
U.S. Census Bureau (2021) The US adult and under-age-18 populations: 2020 Census. 2020 Census redistricting data (Public Law 4-171) Summary File. https://www.census.gov/library/visualizations/interactive/adult-and-under-the-age-of-18-populations-2020-census.html. Accessed 1 July 2021
Wiler JL, Welch S, Pines J, Schuur J, Jouriles N, Stone-Griffith S (2015) Emergency department performance measures updates: proceedings of the 2014 emergency department benchmarking alliance consensus summit. Acad Emerg Med 22:542–553. https://doi.org/10.1111/acem.12654
Selvarajan SK, Levin DC, Parker L (2019) The increasing use of emergency department imaging in the United States: is it appropriate? Am J Roentgenol 213:W180–W184. https://doi.org/10.2214/AJR.19.21386
Bellolio MF, Heien HC, Sangaralingham LR, Jeffery MM, Campbell RL, Cabrera D, Shah ND, Hess EP (2017) Increased computed tomography utilization in the emergency department and its association with hospital admission. West J Emerg Med 18:835–845. https://doi.org/10.5811/westjem.2017.5.34152
Rao PM, Rhea JT, Novelline RA, Mostafavi AA, McCabe CJ (1998) Effect of computed tomography of the appendix on treatment of patients and use of hospital resources. N Engl J Med 338:141–146. https://doi.org/10.1056/NEJM199801153380301
Juszczyk K, Ireland K, Thomas B, Kroon HM, Hollington P (2019) Reduction in hospital admissions with an early computed tomography scan: results of an outpatient management protocol for uncomplicated acute diverticulitis. ANZ J Surg 89:1085–1090. https://doi.org/10.1111/ans.15285
Agarwal M, Udare A, Patlas M, Ramonas M, Alaref AA, Rozenberg R, Ly DL, Golev DS, Mascola K, van der Pol CB (2020) Effect of COVID-19 on computed tomography usage and critical test results in the emergency department: an observational study. CMAJ Open 8:E568–E576. https://doi.org/10.9778/cmajo.20200148
Parikh KD, Ramaiya NH, Kikano EG, Tirumani SH, Pandya H, Stovicek B, Sunshine JL, Plecha DM (2020) COVID-19 pandemic impact on decreased imaging utilization: a single institutional experience. Acad Radiol 27:1204–1213. https://doi.org/10.1016/j.acra.2020.06.024
Parikh KD, Ramaiya NH, Kikano EG, Tirumani SH, Pierce J, Butcher C, Sunshine JL, Plecha DM (2020) Quantifying the decrease in emergency department imaging utilization during the COVID-19 pandemic at a multicenter healthcare system in Ohio. Emerg Radiol 27:765–772. https://doi.org/10.1007/s10140-020-01848-4
Houshyar R, Tran-Harding K, Glavis-Bloom J, Nguyentat M, Mongan J, Chahine C, Loehfelm TW, Kohli MD, Zaragoza EJ, Murphy PM, Kampalath R (2020) Effect of shelter-in-place on emergency department radiology volumes during the COVID-19 pandemic. Emerg Radiol 27:781–784. https://doi.org/10.1007/s10140-020-01797-y
Adjemian J, Hartnett KP, Kite-Powell A, DeVies J, Azondekon R, Radhakrishnan L, van Santen KL, Rodgers L (2021) Update: COVID-19 pandemic-associated changes in emergency department visits - United States, December 2020-January 2021. Morb Mortal Wkly Rep 70:552–556. https://doi.org/10.15585/mmwr.mm7015a3
Fang Y, Zhang H, Xie J, Lin M, Ying L, Pang P, Ji W (2020) Sensitivity of chest CT for COVID-19: comparison to RT-PCR. Radiology 296:E115–E117. https://doi.org/10.1148/radiol.2020200432
Carpenter CR, Mudd PA, West CP, Wilber E, Wilber ST (2020) Diagnosing COVID-19 in the emergency department: a scoping review of clinical examinations, laboratory tests, imaging accuracy, and biases. Acad Emerg Med 27:653–670. https://doi.org/10.1111/acem.14048
Di Minno A, Ambrosino P, Calcaterra I, Di Minno MND (2020) COVID-19 and venous thromboembolism: a meta-analysis of literature studies. Semin Thromb Hemost 46:763–771. https://doi.org/10.1055/s-0040-1715456
Lam CN, Axeen S, Terp S, Burner E, Dworkis DA, Arora S, Menchine M (2021) Who stayed home under safer-at-home? Impacts of COVID-19 on volume and patient-mix at an emergency department. West J Emerg Med 22:234–243. https://doi.org/10.5811/westjem.2020.12.49234
Smulowitz PB, O’Malley AJ, Khidir H, Zaborski L, McWilliams JM Landon BE (2021) National trends in ED visits, hospital admissions, and mortality for medicare patients during the COVID-19 pandemic. Health Aff (Millwood) 40:1457–1464. https://doi.org/10.1377/hlthaff.2021.00561
Finkelstein Y, Maguire B, Zemek R et al (2021) Effect of the COVID-19 pandemic on patient volumes, acuity, and outcomes in pediatric emergency departments: a nationwide study. Pediatr Emerg Care 37:427–434. https://doi.org/10.1097/PEC.0000000000002484
Lieveld AWE, Azijli K, Teunissen BP et al (2021) Chest CT in COVID-19 at the ED: validation of the COVID-19 reporting and data system (CO-RADS) and CT ceverity score: a prospective, multicenter, observational study. Chest 159:1126–1135. https://doi.org/10.1016/j.chest.2020.11.026
Homayounieh F, Holmberg O, Al Umairi R, Aly S, Basevičius A, Costa PR, Darweesh A, Gershan V, Ilves P, Kostova-Lefterova D, Renha SK, Mohseni I, Rampado O, Rotaru N, Shirazu I, Sinitsyn V, Turk T, Van Ngoc TC, Kalra MK, Vassileva J (2021) Variations in CT utilization, protocols, and radiation doses in COVID-19 pneumonia: results from 28 countries in the IAEA study. Radiology 298:E141–E151. https://doi.org/10.1148/radiol.2020203453
Carlicchi E, Gemma P, Poerio A, Caminati A, Vanzulli A, Zompatori M (2021) Chest-CT mimics of COVID-19 pneumonia-a review article. Emerg Radiol 28:507–518. https://doi.org/10.1007/s10140-021-01919-0
He J, Guo Y, Mao R, Zhang J (2021) Proportion of asymptomatic coronavirus disease 2019: a systematic review and meta-analysis. J Med Virol 93:820–830. https://doi.org/10.1002/jmv.26326
Protecting access to Medicare act of 2014 - public law 113–93. Sec. 218. Quality incentives for computed tomography diagnostic imaging and promoting evidence-based care. https://www.govinfo.gov/content/pkg/PLAW-113publ93/pdf/PLAW-113publ93.pdf. Accessed 1 July 2021
Myers LC, Einbinder J, Camargo CAJ, Aaronson EL (2021) Characteristics of medical malpractice claims involving emergency medicine physicians. J Healthc Risk Manag 41:9–15. https://doi.org/10.1002/jhrm.21450
Roslund G (2014) Medical liability and the emergency physician: a state by state comparison - part 2. Common Sense 2014:27–30
Funding
Research reported in this publication was supported, in part, by the National Institutes of Health’s National Center for Advancing Translational Sciences, Grant Number UL1TR001422.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Daniel S. Cruz, Howard S. Kim, Danielle M. McCarthy, and Timothy M. Loftus. The first draft of the manuscript was written by Timothy M. Loftus and Emily G. Wessling, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they no conflict of interest.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
10140_2022_2071_MOESM1_ESM.docx
Supplementary file1 (DOCX 83 KB) eFig. 1Interrupted time series analysis of weekly CT abdomen/pelvis utilization per 100 ED visits. Observed CT abdomen/pelvis utilization is plotted in solid black dots and predicted utilization plotted on solid black line. There was no immediate or longer term effect of the COVID pandemic on observed weekly CT abdomen/pelvis utilization compared to predicted rates.
10140_2022_2071_MOESM2_ESM.docx
Supplementary file2 (DOCX 83 KB) eFig. 2Interrupted time series analysis of weekly CT head utilization per 100 ED visits. Observed CT head utilization is plotted in solid black dots and predicted utilization plotted on solid black line. There was no immediate or longer term effect of the COVID pandemic on observed weekly CT head utilization compared to predicted rates.
10140_2022_2071_MOESM3_ESM.docx
Supplementary file3 (DOCX 83 KB) eFig. 3Sensitivity analysis of COVID-suspected visits only. Graph shows an interrupted time series analysis of weekly CT chest utilization per 100 ED visits. Observed CT chest utilization is plotted in solid black dots and predicted utilization plotted on solid black line. There was an immediate effect on the pandemic declaration (week 62) followed by a nadir utilization rate below that of the pre-pandemic baseline, followed by a longer term effect of the COVID pandemic on observed weekly CT chest utilization compared to predicted rates in ED patients with suspected COVID.
Rights and permissions
About this article
Cite this article
Loftus, T.M., Wessling, E.G., Cruz, D.S. et al. Impact of the COVID pandemic on emergency department CT utilization: where do we go from here?. Emerg Radiol 29, 879–885 (2022). https://doi.org/10.1007/s10140-022-02071-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10140-022-02071-z