Abstract
Background
Stoma closure is associated with high wound infection rates. The aim of this study was to evaluate risk factors for infection rates in such wounds, with particular emphasis on assessing the importance of the stomal wound closure technique.
Methods
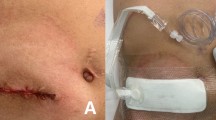
A retrospective analysis of 142 patients who had undergone ileostomy or colostomy closure between 2002 and 2011 was performed. Postoperative outcome as measured by wound infection rate was recorded. Three different closure techniques were identified: primary closure (PC), primary closure with Penrose drain (PCP) and purse-string circumferential wound approximation technique (PSC). Other factors such as age, sex, ASA score, type of prophylactic antibiotics used, diabetes, smoking and obesity were also analysed. All other techniques were excluded.
Results
Our series consisted of 142 stomal closures (90 ileostomy and 52 colostomy closures). The patients had a median age of 63.5 years with an interquartile range of 50.1–73.2 years. The overall wound infection rate was 10.7 %. PC, PCP and PSC were associated with wound infection rates of 17.9, 10.5 and 3.6 %, respectively. Compared to PSC, PC and PCP were associated with significantly higher wound infection rates (p = 0.027 and p = 0.068, respectively). Obesity was a significant risk factor for wound infection (p = 0.024). Use of triple-agent antibiotics prophylactically had a protective effect on the infection rate (p = 0.012).
Conclusions
To reduce stomal wound closure infection rates, we recommend institution of closure techniques other than PC with or without a drain. Risk factors such as obesity should be addressed, and prophylactic triple antibiotics should be administered.


Similar content being viewed by others
References
Gastinger I, Marusch F, Steinert R, Wolff S, Koekerling F, Lipport H (2005) Protective defunctioning stoma in low anterior resection for rectal carcinoma. Br J Surg 92:1137–1142
Tan WS, Tang CL, Shi L, Eu KW (2009) Meta-analysis of defunctioning stoma in low anterior resection for rectal cancer. Br J Surg 96:462–472
Oomen JL, Cuesta MA, Engel AF (2005) Reversal of Hartmann’s procedure after surgery for complications of diverticular disease of the sigmoid colon is safe and possible in most patients. Dig Surg 22:419–425
Keck JO, Collopy BT, Ryan PJ, Fink R, Mackay JR, Woods RJ (1994) Reversal of Hartmann’s procedure: effect of timing and technique on ease and safety. Dis Colon Rectum 37:243–248
Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG (1992) CDC definition of nosocomial surgical site infection, 1992: a modification of CDC definition of surgical wound infection. Infect Control Hosp Epidemiol 13:606–608
Milanchi S, Nasseri Y, Kidner T, Fleshner P (2009) Wound infection after ileostomy closure can be eliminated by circumferential subcuticular wound approximation. Dis Colon Rectum 52:469–474
Williams LA, Sagar PM, Finan PJ, Burke D (2008) The outcome of loop ileostomy closure: a prospective study. Colorectal Dis 10:460–464
Perez RO, Habr-Gama A, Seid VE et al (2006) Loop ileostomy morbidity: timing of closure matters. Dis Colon Rectum 49:1539–1545
Mann LJ, Stewart PJ, Goodwin RJ, Chapus PH, Bokey EL (1991) Complications following closure of loop ileostomy. ANZ J Surg 61:493–496
Phang PT, Hain JM, Perez-Ramirez JJ, Madoff RD, Gernio BT (1999) Techniques and complications of ileostomy takedown. Am J Surg 177:463–466
Lahat G, Tulchinsky H, Goldman G, Klauzner JM, Rabau M (2005) Wound infection after ileostomy closure: a prospective randomized study comparing primary vs. delayed primary closure technique. Tech Coloproctol 9:206–208
Sutton CD, Williams N, Marshall L, Lloyd G, Thomas WM (2002) A Technique for wound closure that minimizes sepsis after stoma closure. ANZ J Surg 72:766–767
Vermulst N, Vermeulen J, Hazebroek EJ, Coene PP, Van der Harst E (2006) Primary closure of the skin after stoma closure. Dig Surg 23:255–258
Wong KS, Remzi FH, Gorgun E et al (2005) Loop ileostomy closure after restorative proctocolectomy: outcome in 1,504 patients. Dis Colon Rectum 48:243–250
Bell C, Asolati M, Hamilton E et al (2005) A comparison of complications associated with colostomy reversal versus ileostomy reversal. Am J Surg 190:717–720
Banerjee A (1997) Pursestring skin closure after stoma reversal. Dis Colon Rectum 40:993–994
Cohen PR, Martinelli PT, Schulze KE, Nelson BR (2007) The cuticular purse string suture: a modified purse string suture for the partial closure of round postoperative wounds. Int J Dermatol 46:746–753
Marquez TT, Christoforidis D, Abraham A, Madoff RD, Rothenberger DA (2010) Wound infection following stoma takedown: primary skin closure versus subcuticular purse-string suture. World J Surg 34:2877–2882
Harold DM, Johnson EK, Rizzo JA, Steele SR (2010) Primary closure of stoma site wound after ostomy takedown. Am J Surg 199:621–624
Keating J, Kelly EW, Hunt I (2003) Save the skin and improve the scar. A simple technique to minimize the scar from a temporary stoma. Dis Colon Rectum 46:1428–1429
Acknowledgments
We would like to thank Dr. Zahrul Ismadi for his assistance with data collection.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mirbagheri, N., Dark, J. & Skinner, S. Factors predicting stomal wound closure infection rates. Tech Coloproctol 17, 215–220 (2013). https://doi.org/10.1007/s10151-012-0908-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-012-0908-4