Abstract
The convergence/divergence of health care systems between countries is an interesting facet of the health care system research from a macroeconomic perspective. In this paper, we concentrate on an important dimension of every health care system, namely the convergence/divergence of health care financing (HCF). Based on data from 22 OECD countries in the time period 1970–2005, we use the public financing ratio (public financing in % of total HCF) and per capita public HCF as indicators for convergence. By applying different concepts of convergence, we find that HCF is converging. This conclusion also holds when we look at smaller subgroups of countries and shorter time periods. However, we find evidence that countries do not move towards a common mean and that the rate of convergence is decreasing over time.


Similar content being viewed by others
Notes
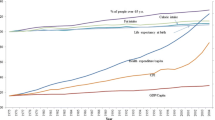
Some studies focus on the outcome indicator health status. For example, Mayer-Foulkes [26] asks whether there are convergence clubs in cross-country life expectancy dynamics.
For the discussion of testing convergence using cross-section or time series data and methods, see Bernard and Durlauf [4]. For the closely related problem of stationarity of health care expenditures and their determinants, see for example Hansen and King [18], McCoskey and Selden [27], Gerdtham and Löthgren [12], Okunade and Karakus [37], MacDonald and Hopkins [25], Dreger and Reimers [11].
Private health insurance can offer primary, duplicate, complementary and supplementary coverage. For a detailed discussion of these different functions, see OECD [36].
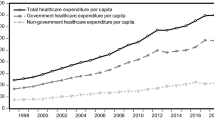
Disaggregated information on the different sources of HCF focused on the collecting stage is not available yet. Hence, health expenditures of public institutions (consisting of central government, provinces/states, municipalities/local governments, social security funds and selected private non-profit institutions) are taken as an indicator for public financing.
Overall, time invariant, country-specific characteristics and differences in the countries’ health care systems that cannot be addressed specifically are accounted for by the specific estimation method (biased corrected LSDV estimator) applied.
Only for data on union density and total tax revenues in Iceland, we cannot justify this replacement of missing entries which results in a loss of 13 observations.
The latter concepts were developed within the framework of neoclassical growth models to explain the convergence in aggregate output (see [3] for convergence in income per capita) and assume the existence of a steady-state in economic development.
Note that our dependent variable refers to its quantity in period t (instead of its growth). If we subtracted 1 from the parameter b, we would get the corresponding coefficient if the growth rate was the dependent variable. The speed of β-convergence can be calculated from the regression coefficient b on the initial level y 0. For example, for the specification at hand, the speed of convergence equals \(-\frac{ln(T b)}{T}\).
One may doubt the exogeneity of the explanatory variables included. Although public HCF may shape the regressors used, such influences do not occur contemporaneously. Rather, it is adequate to assume that the effects of public HCF on the regressors occur with some time lags meaning that today’s HCF influences tomorrow’s insurance coverage, proportion of elderly, GDP, … but not today’s levels.
We determine the number of lags to be included based on the Schwartz Bayesian information criterion and the Akaike information criterion.
If b = 1, the series follows a random walk.
These values were calculated by multiplying public with the real health expenditures per capita that range from 174 to 5,616 US$ with a mean of 1,670 US$.
NHS countries are Denmark, Finland, Ireland, Iceland, Italy, Norway, Portugal, Sweden, Spain and the United Kingdom. Austria, Belgium, Germany, France, Luxembourg and the Netherlands represent the group of SHI countries. Australia, Canada, Japan, New Zealand, Switzerland and the United States together form the group ‘Others’ as they can neither be classified as NHS nor as SHI countries (Switzerland, USA) or do not belong to Europe.
In order to improve clarity, we forgo plotting public for the third group. The corresponding values are lower at each point in time. The minimum (maximum) is 63.2% (69.3%) in 1971 (1984). The line in Fig. 3 referring to the total sample includes these values. This explains why the curve picturing the total sample always runs below the curves for the two other subsamples.
As before, we do not plot the values for the other countries for clarity reasons but their values are included in the plot representing the total sample.
For the panel specification, the rate of convergence is given by β = − (ln b).
We classify those countries as old NHS countries which were already NHS-systems at the beginning of the observation period (Denmark, Great Britain, Finland, Iceland, Ireland, Norway, Sweden). Countries that changed to a NHS-system during the past 36 years are defined as new NHS countries (Italy in 1978, Portugal in 1979, Spain in 1987).
References
Alcalde-Unzu J., Ezcurra R., Pascual P.: Cross-country disparities in health-care expenditure: a factor decomposition. Health Econ. 18, 479–485 (2009)
Aldridge, S.C., Sundarapandiyan, S.: The convergence model in health care reform: experience from Singapore, the United Kingdom and the United States. Asian J. Public Admin. 17, 60–104 (1995)
Barro, R.J., Sala-i Martin, X.: Convergence. J. Politic. Econ. 100, 223–251 (1992)
Bernard, A.B., Durlauf, S.N.: Interpreting tests of the convergence hypothesis, technical working paper series 159, NBER (1994)
Bruno, G.S.F.: Estimation and inference in dynamic unbalanced panel data models with a small number of individuals, working paper 165, Universita Bocconi-CESPRI (2005)
Busse, R., Schreyögg, J., Gericke, C.: Analyzing changes in health financing arrangements in high-income countries—a comprehensive framework approach, health, nutrition and population (HNP) discussion paper of the World Bank’s Human Development Network, World Bank. http://www.worldbank.org/hnppublications (2007)
Clemente, J., Marcuello, C., Montañes, A., Pueyo, F.: On the international stability of health care expenditure functions: are government and private functions similar? J. Health Econ. 23, 589–613 (2004)
Cohen, R.A., Makuc, D.M., Bernstein, A.B., Bilheimer, L.T., Powel-Griner, E.: Health insurance coverage trends: estimates from the national health interview survey. Natl. Health Stat. Rep. 17, 1–28 (2009)
Comas Herrera, A. Is there a convergence in the health expenditures of the EU member states. In: Mossialos E., Le Grand J. (eds) Health Care and Cost Containment in the European Union. Ashgate, Aldershot, pp. 197–218 (1999)
Corrado, L., Londoño, B.D.A., Mennini, F.S., Trovato, G.: The welfare states in a United Europe. Eur. Politic. Econ. Rev. 1, 40–55 (2003)
Dreger, C., Reimers, H.-E.: Health care expenditures in OECD countries: a panel root and cointegration analysis. Int. J. Appl. Econ. Quant. Stud. 2, 5–20 (2005)
Gerdtham, U.-G., Löthgren, M.: On stationarity and conintegration of international health expenditure and GDP. J. Health Econ. 19, 461–475 (2000)
Glied, S.A.: Health care financing, efficiency, and equity, working paper No. 13881, NBER. http://www.nber.org/papers/w13881 (2008)
Glied, S.A.: Universal public health insurance and private coverage: externalities in health care consumption, working paper No. 13885, NBER. http://www.nber.org/paperss/w13885 (2008)
Globerman, S., Hodges, H., Vining, A.: Canadian and US health care systems performance and governance: elements of convergence, technical report, EconWPA. http://www.129.3.20.41/eps/pe/papers/0404/0404003.pdf (2001)
Globerman, S., Vining, A.: A policy perspective on ‘mixed’ health care financial systems of business and economics. J. Risk Insur. 65, 57–80 (1998)
Gouveia, M.: The public sector and health care. Int. Tax Public Financ. 3, 329–349 (1996)
Hansen, P., King, A.: The determinants of health care expenditure: a cointegration approach. J. Health Econ. 15, 127–137 (1996)
Hitiris, T., Nixon, J.: Convergence of health care expenditure in the EU countries. Appl. Econ. Lett. 8, 223–228 (2001)
Hurley, J.: An overview of the normative economics of the health care sector. In: Culyer A.J., Newhouse J.P. (eds) Handbook of Health Economics, vol. 1A. Elsevier, Amsterdam, pp. 55–118 (2000)
Kerem, K., Puss, T., Maldre, R.: Health and convergence of health care expenditure in EU. Int. Business Econ. Res. J. 2, 29–43 (2008)
Kim, T.-K., Zurlo, K.: How does economic globalisation affect the welfare state? focusing on the mediating effect of welfare regimes. Int. J. Soc. Welf. 17, 1–12 (2008)
Kiviet, J.F.: On bias, inconsistency, and efficiency of various estimators in dynamic panel data models. J. Econ. 68, 53–78 (1995)
Levin, A., Lin, C.-F., Chu Chia-Shang, J.: Unit root tests in panel data: asymptotic and finite sample properties. J. Econ. 108, 1–24 (2002)
MacDonald G., Hopkins S.: Unit root properties of OECD health care expenditure and GDP data. Health Econ. 11, 371–376 (2002)
Mayer-Foulkes, D.: Convergence clubs in cross-country life expectancy dynamics, discussion paper No. 2001/124, World Institute for Development Economics Research (2001)
McCoskey, S., Selden, T.: Health care expenditures and GDP: panel data unit root test results. J. Health Econ. 17, 369–376 (1998)
Montero-Granados, R., De Dios Jimenez, J., Martin, J.: Decentralisation and convergence in health among the provinces of Spain. Soc. Sci. Med. 64, 1253–1264 (2007)
Narayan P.K.: Do health expenditures ‘catch-up’?. Evidence from OECD countries. Health Econ. 16, 993–1008 (2007)
Narayan, P.K., Narayan, S.: The role of permanent and transitory shocks in explaining international health expenditures. Health Econ. 17, 1171–1186 (2008)
Nerlove, M.: Further evidence on the estimation of dynamic economic relations from a time series of cross-sections. Econometrica 39, 359–387 (1971)
Nickell, S.: Biases in dynamic models with fixed effects. Econometrica 49, 1417–1426 (1981)
Nixon, J.: Convergence analysis of health care expenditure using two approaches, Discussion Papers in Economics No. 99/3, University of York (1999)
Nixon, J.: Convergence of health care spending and health outcomes in the European Union, 1960-95, Discussion Paper Series No. 183, Centre for Health Economics (2000)
OECD: A System of health accounts, Paris (2000)
OECD: Private health insurance in OECD countries, Paris (2004)
Okunade, A., Karakus, M.C.: Unit root and cointegration tests: time series versus panel estimates for international health expenditure models. Appl. Econ. 33, 1131–1137 (2001)
Okunade, A., Murthy, V.: Technology as a ‘major driver’ of health care costs: a cointegration analysis of the Newhouse conjecture. J. Health Econ. 21, 147–159 (2002)
Okunade A., Suraratdecha C.: The pervasiveness of pharmaceutical expenditure inertia in the OECD countries. Soc. Sci. Med. 63, 225–238 (2006)
Pierson, P.: Increasing returns, path dependence, and the study of politics. Am. Politic. Sci. Rev. 94, 251–267 (2000).
Propper, C., Green, K.: A larger role for the private sector in health care? a review of arguments, working paper series no. 99/009, Centre for Market and Public Organisation (CMPO) (1999)
Saltman, R.B.: Convergence versus social embeddedness. Eur. J. Public Health 7, 449–453 (1997)
Sanz I., Velázquez, F.J.: The evolution and convergence of the government expenditure composition in the OECD countries. Public Choice 119, 61–72 (2004)
van Doorslaer, E., Koolman, X., Jones, A.: Explaining income-realted inequalities in doctors utilisation in Europe. Health Econ. 13, 629–647 (2004)
Wagstaff, A., van Doorslaer.: Equity in health care finance and delivery. In: Culyer A., Newhouse J. (eds) Handbook of Health Economics, vol. 2. Elsevier, Amsterdam, pp. 1803–1862 (2000)
Wang, Z.: The convergence of health care expenditure in the US States. Health Econ. 18, 55–70 (2009)
Wendt, C., Grimmeisen, S., Rothgang, H.: Convergence or divergence of OECD health care systems?. In: Cantillon B., Marx I. (eds) International Cooperation in Social Security. Antwerpen, Oxford, pp. 15–45 (2005)
Wolf, H.: Globalization and the convergence of social expenditure in the European union, occasional paper series, GW Center of the Study of Globalization (2002)
Wooldridge, J.M.: Econometric Analysis of Cross Section and Panel Data. Cambridge and London: MIT-Press(2002)
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors would like to thank Jesus Crespo-Cuaresma, Michael Pfaffermayr, Harald Oberhofer, Hannes Winner for valuable discussion and two anonymous reviewers for helpful comments
Rights and permissions
About this article
Cite this article
Leiter, A.M., Theurl, E. The convergence of health care financing structures: empirical evidence from OECD-countries. Eur J Health Econ 13, 7–18 (2012). https://doi.org/10.1007/s10198-010-0265-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-010-0265-z