Abstract
This study quantifies the extent socioeconomic status (SES) affects hospital utilization and adverse hospital events of chronic disease patients. After identifying the initial first-year spell of the disease, we examine six outcomes that include measures of utilization and incidence of adverse in-hospital events. Three years of hospital administrative data from the state of Victoria, Australia, are used to extract a sample of 237,743 patients with chronic disease spells. SES is measured using the utilization records of specific health and human services. The study finds that, compared to patients with no disadvantage, SES disadvantaged patients tend to incur higher hospital costs and longer utilization by about 20% and greater incidence of in-hospital adverse outcomes by up to 80% than non-disadvantaged patients. Further analysis shows that hospital adverse outcomes indirectly contribute to about a quarter of the observed difference in hospital costs between SES disadvantaged and non-disadvantaged patients.

Similar content being viewed by others
Notes
Besides SES Group, other covariates include disease group dummies, gender, age, marital status, rurality, number of diagnoses, number of the previous admission, and ICU hours as a private patient. See “Appendix 1” for a complete listing of all covariates and their coefficient estimates.
The list of covariates in these regressions can be found in “Appendix 1”.
References
Baron, R.M., Kenny, D.A.: The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J. Pers. Soc. Psychol. 51(6), 1173–82 (1986)
Braveman, P., Egerter, S., Williams, D.R.: The Social Determinants of Health: Coming of Age. Annu. Rev. Public Health 32(1), 381–98 (2011). https://doi.org/10.1146/annurev-publhealth-031210-101218
Charlton, J., Rudisill, C., Bhattarai, N., Gulliford, M.: Impact of deprivation on occurrence, outcomes and health care costs of people with multiple morbidity. J. Health Serv. Res. 18(4), 215–23 (2013)
Cheng, T.C., Haisken-DeNew, J., Yong, J.: Cream skimming and hospital transfers in a mixed public-private system. Soc. Sci. Med. 132, 156–164 (2015)
Cohen, A.K., Rai, M., Rehkopf, D.H., Abrams, B.: Educational attainment and obesity: a systematic review. Obes. Rev. 14(12), 989–1005 (2013). https://doi.org/10.1111/obr.12062
Cookson, R., Propper, C., Asaria, M., Raine, R.: Socio-economic inequalities in health care in England. Fiscal Stud. 37(3–4), 371–403 (2016)
Dixon, A., Le Grand, J., Henderson, J., Murray, R., Poteliakhoff, E.: Is the British National Health Service equitable? The evidence on socioeconomic differences in utilization. J. Health Serv. Res. Policy 12(2), 104–9 (2007)
Fleurbaey, M., Schokkaert, E.: Equity in health and health care. In: Pauly, M.V., Mcguire, T.G., Barros, P.P. (eds.) Handbook of Health Economics, vol. 2, pp. 1003–92. Elsevier, Oxford (2012)
Goddard, M., Smith, P.: Equity of access to health care services. Soc. Sci. Med. 53, 1149–62 (2001)
Haan, M., Kaplan, G.A., Camacho, T.: Poverty and health: prospective evidence from the alameda county study. Am. J. Epidemiol. 185(11), 1161–70 (2017). https://doi.org/10.1093/aje/kwx112
Hill, S.C., Miller, G.E.: Health expenditure estimation and functional form: application of the generalized gamma and extended estimating equation models. Health Econ. 19(5), 608–627 (2010)
Jones, A.M., Rice, N., d’Uva, T.B., Balia, S.: Applied Health Economics. Routledge, New York (2007)
Jones, A.M.: Models for health care. In: Clement, M.P., Hendry, D.F. (eds.) The Oxford Handbook of Economic Forecasting, pp. 625–654. Oxford University Press, New York (2011). (chap 23)
Lostao, L., Geyer, S., Albaladejo, R., Moreno-Lostao, A., Santos, J.M., Regidor, E.: Socioeconomic position and health services use in Germany and Spain during the Great Recession. PLoS One 12(8), e0183325 (2017). https://doi.org/10.1371/journal.pone.0183325
Liu, R.S., Aiello, A.E., Mensah, F.K., Gasser, C.E., Rueb, K., Cordell, B., Juonala, M., Wake, M., Burgner, D.P.: Socioeconomic status in childhood and C reactive protein in adulthood: a systematic review and meta-analysis. J. Epidemiol. Community Health 71(8), 817–26 (2017). https://doi.org/10.1136/jech-2016-208646
Löfvendahl, S.A., Jöud, I.F., Petersson, E.Theander, Svensson, Å., Carlsson, K.S.: Income disparities in health care use remain after controlling for health care need: evidence from Swedish register data on psoriasis and psoriatic arthritis. Eur. J. Health Econ. 19(3), 447–462 (2018). https://doi.org/10.1007/s10198-017-0895-5
Lusardi, A., Schneider, D., Tufano, P.: The economic crisis and medical care use: comparative evidence from five high-income countries. Soc. Sci. Q. 96(1), 202–13 (2015)
Mirowsky, J., Ross, C.E.: Education, Social Status, and Health. Aldine de Gruyter, Hawthorne (2003)
Marmot, M.G., Kogevinas, M., Elston, M.A.: Social/economic status and disease. Annu. Rev. Public Health 8(1), 111–35 (1987). https://doi.org/10.1146/annurev.pu.08.050187.000551
Morello-Frosch, R., Zuk, M., Jerrett, M., Shamasunder, B., Kyle, A.D.: Understanding the cumulative impacts of inequalities in environmental health: implications for policy. Health Aff. 30(5), 879–87 (2011)
Morris, S., Sutton, M., Gravelle, H.: Inequity and inequality in the use of health care in England: an empirical investigation. Soc. Sci. Med. 60, 1251–66 (2005)
Mueller, C.W., Parcel, T.L.: Measures of socioeconomic status: alternatives and recommendations. Child Dev. 52(1), 13–30 (1981). https://doi.org/10.2307/1129211
Preacher, J.K., Hayes, A.F.: Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav. Res. Methods 40(3), 879–91 (2008)
Susser, M.W., Watson, W., Hopper, K.: Sociology in Medicine. Oxford University Press, New York (1985)
Sutton, M.: Vertical and horizontal aspects of socio-economic inequity in general practitioner contacts in Scotland. Health Econ. 11, 537–49 (2002)
Terraneo, M.: Inequities in health care utilization by people aged 50+: evidence from 12 European countries. Soc. Sci. Med. 126, 154–63 (2015). https://doi.org/10.1016/j.socscimed.2014.12.028
Van Doorslaer, E., Wagstaff, A., van der Burg, H., et al.: Equity in the delivery of health care in Europe and the US. J. Health Econ. 19(5), 553–83 (2000)
Wagstaff, A., van Doorslaer, E.: Equity in health care finance and delivery. In: Culyer, A.J., Newhouse, J.P. (eds.) Handbook of Health Economics, vol. 1, pp. 1803–62. Elsevier, Oxford (2000). (Part B)
Acknowledgements
This paper arises out of a project commissioned by the Victorian Department of Health and Human Services (DHHS). The views expressed herein are those of the authors and do not necessarily reflect the views of the Department. The authors are grateful to the Victorian DHHS for funding support and making possible access to the data, to Peter Breadon, Laura Andrew, Ross Geddes for many rounds of discussions on earlier drafts, and especially to Tristan Bouckley for coordinating the project and facilitating data access. The authors have no other competing interests to declare.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Appendix 1: Additional tables
Appendix 1: Additional tables
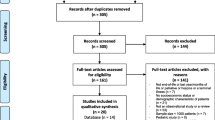
Exclusion criteria
The following exclusion criteria are applied because patients with certain characteristics are considered to be different in important ways from other patients. For example, chronic disease patients suffering from complications such as cancer, HIV or an organ transplant are clearly in worse health and/or likely to incur much higher costs than patients who did not have such complications. Likewise, patients who died have an incomplete or truncated spell—had they survived, they might have recorded higher utilization and more adverse outcomes (Table 5).
Summary statistics of covariates used in regressions
Table 6 presents the summary statistics of the covariates by SES group. Generally patients in moderate and high disadvantage groups are older, more of them are widowed or divorced, living in major cities (where social services are more widely availabe than in regional and remote areas), and with more complex health conditions.
Regressions for estimating indirect effects in mediation analysis
Tables 7 and 8 show the coefficient estimates and standard errors for regression models estimated to conduct the mediation analysis to obtain the indirect effect estimates of SES. The indirect effect estimates reported in Table 4 are obtained as the product of the coefficients on adverse outcomes in Table 7 and the coefficients on SES in Table 8.
Rights and permissions
About this article
Cite this article
Yong, J., Yang, O. Does socioeconomic status affect hospital utilization and health outcomes of chronic disease patients?. Eur J Health Econ 22, 329–339 (2021). https://doi.org/10.1007/s10198-020-01255-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10198-020-01255-z