Abstract
Encapsulated microbubbles (MBs) serve as endovascular agents in a wide range of medical ultrasound applications. The oscillatory response of these agents to ultrasonic excitation is determined by MB size, gas content, viscoelastic shell properties and geometrical constraints. The viscoelastic parameters of the MB capsule vary during an oscillation cycle and change irreversibly upon shell rupture. The latter results in marked stress changes on the endothelium of capillary blood vessels due to altered MB dynamics. Mechanical effects on microvessels are crucial for safety and efficacy in applications such as focused ultrasound-mediated blood–brain barrier (BBB) opening. Since direct in vivo quantification of vascular stresses is currently not achievable, computational modelling has established itself as an alternative. We have developed a novel computational framework combining fluid–structure coupling and interface tracking to model the nonlinear dynamics of an encapsulated MB in constrained environments. This framework is used to investigate the mechanical stresses at the endothelium resulting from MB shell rupture in three microvessel setups of increasing levels of geometric detail. All configurations predict substantial elevation of up to 150 % for peak wall shear stress upon MB breakup, whereas global peak transmural pressure levels remain unaltered. The presence of red blood cells causes confinement of pressure and shear gradients to the proximity of the MB, and the introduction of endothelial texture creates local modulations of shear stress levels. With regard to safety assessments, the mechanical impact of MB breakup is shown to be more important than taking into account individual red blood cells and endothelial texture. The latter two may prove to be relevant to the actual, complex process of BBB opening induced by MB oscillations.








Similar content being viewed by others
References
Abbott NJ, Romero IA (1996) Transporting therapeutics across the blood–brain barrier. Mol Med Today 2:106–113
Abbott NJ et al (2010) Structure and function of the blood–brain barrier. Neurobiol Dis 37:13–25
Bertossi M et al (1997) Ultrastructural and morphometric investigation of human brain capillaries in normal and peritumoral tissues. Ultrastruct Pathol 21:41–49
Borden MA, Longo ML (2002) Dissolution behavior of lipid monolayer-coated, air-filled microbubbles: effect of lipid hydrophobic chain length. Langmuir 18:9225–9233
Caskey CF et al (2007) Direct observations of ultrasound microbubble contrast agent interaction with the microvessel wall. J Acoust Soc Am 122:1191–1200
Caskey CF et al (2009) Microbubble tunneling in gel phantoms. J Acoust Soc Am 125:EL183–EL189
Cassot F et al (2006) A novel three-dimensional computer-assisted method for a quantitative study of microvascular networks of the human cerebral cortex. Microcirculation 13:1–18
Chatterjee D, Sarkar K (2003) A Newtonian rheological model for the interface of microbubble contrast agents. Ultrasound Med Biol 29:1749–1757
Chen H, Konofagou EE (2014) The size of blood–brain barrier opening induced by focused ultrasound is dictated by the acoustic pressure. J Cereb Blood Flow Metab 34:1197–1204
Chen H et al (2011) Blood vessel deformations on microsecond time scales by ultrasonic cavitation. Phys Rev Lett 106:034301
Chin CT et al (2003) Brandaris 128: a digital 25 million frames per second camera with 128 highly sensitive frames. Rev Sci Instrum 74:5026–5034
Church CC (1995) The effects of an elastic solid-surface layer on the radial pulsations of gas-bubbles. J Acoust Soc Am 97:1510–1521
Davies PF et al (1997) Spatial relationships in early signaling events of flow-mediated endothelial mechanotransduction. Annu Rev Physiol 59:527–549
Dayton PA et al (1999) Optical and acoustical observations of the effects of ultrasound on contrast agents. IEEE Trans Ultrason Ferroelectr Freq Control 46:220–232
de Jong N et al (2000) Optical imaging of contrast agent microbubbles in an ultrasound field with a 100-MHz camera. Ultrasound Med Biol 26:487–492
de Jong N et al (2007) “Compression-only” behavior of phospholipid-coated contrast bubbles. Ultrasound Med Biol 33:653–656
de Jong N et al (2009) Ultrasonic characterization of ultrasound contrast agents. Med Biol Eng Comput 47:861–873
Degroote J, Bathe KJ, Vierendeels J (2009) Performance of a new partitioned procedure versus a monolithic procedure in fluid–structure interaction. Comput Struct 87:793–801
Doinikov AA, Haac JF, Dayton PA (2009) Modeling of nonlinear viscous stress in encapsulating shells of lipid-coated contrast agent microbubbles. Ultrasonics 49:269–275
Fang F, Szleifer I (2001) Kinetics and thermodynamics of protein adsorption: a generalized molecular theoretical approach. Biophys J 80:2568–2589
Ferrara K, Pollard R, Borden M (2007) Ultrasound microbubble contrast agents: fundamentals and application to gene and drug delivery. Annu Rev Biomed Eng 9:415–447
Ferziger JH, Peric M (1995) Computational methods for fluid dynamics. Springer Verlag, Berlin-New York
Fischer M et al (1996) Flow velocity of single lymphatic capillaries in human skin. Am J Physiol Heart C 270:H358–H363
Gorce JM, Arditi M, Schneider M (2000) Influence of bubble size distribution on the echogenicity of ultrasound contrast agents— a study of SonoVue (TM). Invest Radiol 35:661–671
Haidekker MA et al (2002) A novel approach to blood plasma viscosity measurement using fluorescent molecular rotors. Am J Physiol Heart C 282:H1609–H1614
Hernot S, Klibanov AL (2008) Microbubbles in ultrasound-triggered drug and gene delivery. Adv Drug Delivery Rev 60:1153–1166
Hoff L, Sontum PC, Hovem JM (2000) Oscillations of polymeric microbubbles: effect of the encapsulating shell. J Acoust Soc Am 107:2272–2280
Hosseinkhah N et al (2013) Mechanisms of microbubble–vessel interactions and induced stresses: a numerical study. J Acoust Soc Am 134:1875–1885
Hosseinkhah N, Goertz DE, Hynynen K (2015) Microbubbles and blood–brain barrier opening: a numerical study on acoustic emissions and wall stress predictions. IEEE Trans Biomed Eng 62:1293–1304
Hosseinkhah N, Hynynen K (2012) A three-dimensional model of an ultrasound contrast agent gas bubble and its mechanical effects on microvessels. Phys Med Biol 57:785–808
Hsiao CT, Chahine GL (2013) Breakup of finite thickness viscous shell microbubbles by ultrasound: a simplified zero-thickness shell model. J Acoust Soc Am 133:1897–1910
Hynynen K (2008) Ultrasound for drug and gene delivery to the brain. Adv Drug Delivery Rev 60:1209–1217
Hynynen K et al (2005) Local and reversible blood–brain barrier disruption by noninvasive focused ultrasound at frequencies suitable for trans-skull sonications. Neuroimage 24:12–20
Issa RI (1986) Solution of the implicitly discretized fluid-flow equations by operator-splitting. J Comput Phys 62:40–65
Jasak H, Tukovic Z (2007) Automatic mesh motion for the unstructured finite volume method. Trans Famena 30:1–18
Jasak H, Jemcov A, Tukovic Z (2007) OpenFOAM: a C++ library for complex physics simulations. Proc Int Workshop on Coupled Methods in Numerical Dynamics, Dubrovnik, Croatia, pp. 47–66
Klotz AR, Hynynen K (2010) Simulations of the Devin and Zudin modified Rayleigh–Plesset equations to model bubble dynamics in a tube. Electron J Tech Acous 11:1–15
Kuttler U et al (2010) Coupling strategies for biomedical fluid-structure interaction problems. Int J Numer Meth Bio 26:305–321
Li Q et al (2013) Modeling complicated rheological behaviors in encapsulating shells of lipid-coated microbubbles accounting for nonlinear changes of both shell viscosity and elasticity. Phys Med Biol 58:985–998
Liu YY, Miyoshi H, Nakamura M (2006) Encapsulated ultrasound microbubbles: therapeutic application in drug/gene delivery. J Control Release 114:89–99
Lowe GDO (1987) Blood rheology in vitro and in vivo. Baillieres Clin Haematol 1:597–636
Marmottant P et al (2005) A model for large amplitude oscillations of coated bubbles accounting for buckling and rupture. J Acoust Soc Am 118:3499–3505
McDannold N, Vykhodtseva N, Hynynen K (2006) Targeted disruption of the blood–brain barrier with focused ultrasound: association with cavitation activity. Phys Med Biol 51:793–807
McDannold N, Vykhodtseva N, Hynynen K (2008) Blood–brain barrier disruption induced by focused ultrasound and circulating preformed microbubbles appears to be characterized by the mechanical index. Ultrasound Med Biol 34:834–840
McHedlishvili GI, Varazashvili MN (1980) High erythrocyte concentration in blood circulating in the brain. Bull Exp Biol Med 90:1479–1481
Miao H, Gracewski SM, Dalecki D (2008) Ultrasonic excitation of a bubble inside a deformable tube: implications for ultrasonically induced hemorrhage. J Acoust Soc Am 124:2374–2384
Moran CM et al (2000) Quantification of microbubble destruction of three fluorocarbon-filled ultrasonic contrast agents. Ultrasound Med Biol 26:629–639
Nyborg WL (2001) Biological effects of ultrasound: development of safety guidelines. Part II: general review. Ultrasound Med Biol 27:301–333
Patabendige A, Skinner RA, Abbott NJ (2013) Establishment of a simplified in vitro porcine blood–brain barrier model with high transendothelial electrical resistance. Brain Res 1521:1–15
Paul S et al (2010) Material characterization of the encapsulation of an ultrasound contrast microbubble and its subharmonic response: strain-softening interfacial elasticity model. J Acoust Soc Am 127:3846–3857
Plesset MS, Prosperetti A (1977) Bubble dynamics and cavitation. Annu Rev Fluid Mech 9:145–185
Pries AR, Secomb TW, Gaehtgens P (2000) The endothelial surface layer. Pflug Arch Eur J Phy 440:653–666
Putnam FW (1975) The plasma proteins : structure, function, and genetic control. Academic Press, New York
Qin SP, Ferrara KW (2006) Acoustic response of compliable microvessels containing ultrasound contrast agents. Phys Med Biol 51:5065–5088
Quaia E (2007) Microbubble ultrasound contrast agents: an update. Eur Radiol 17:1995–2008
Sarkar K et al (2005) Characterization of ultrasound contrast microbubbles using in vitro experiments and viscous and viscoelastic interface models for encapsulation. J Acoust Soc Am 118:539–550
Schlachetzki F et al (2002) Observation on the integrity of the blood–brain barrier after microbubble destruction by diagnostic transcranial color-coded sonography. J Ultrasound Med 21:419–429
Secomb TW, Hsu R, Pries AR (2006) Tribology of capillary blood flow. P I Mech Eng J-J Eng 220:767–774
Sheikov N et al (2004) Cellular mechanisms of the blood–brain barrier opening induced by ultrasound in presence of microbubbles. Ultrasound Med Biol 30:979–989
Stride E (2005) Characterization and design of microbubble-based contrast agents suitable for diagnostic imaging. Medical radiology. In: Quaia E (ed) Contrast Media in Ultrasonography. Springer, Berlin Heidelberg, pp 31–42
Stride E, Saffari N (2003a) Microbubble ultrasound contrast agents: a review. P I Mech Eng H 217:429–447
Stride E, Saffari N (2003b) On the destruction of microbubble ultrasound contrast agents. Ultrasound Med Biol 29:563–573
Stride E, Saffari N (2004) Theoretical and experimental investigation of the behaviour of ultrasound contrast agent particles in whole blood. Ultrasound Med Biol 30:1495–1509
Stucker M et al (2004) Capillary blood cell velocity in periulcerous regions of the lower leg measured by laser Doppler anemometry. Skin Res Technol 10:174–177
Tu J et al (2009) Estimating the shell parameters of SonoVue (R) microbubbles using light scattering. J Acoust Soc Am 126:2954–2962
Tukovic Z, Jasak H (2007) Updated Lagrangian finite volume solver for large deformation dynamic response of elastic body. Trans Famena 31:55–70
Tukovic Z, Jasak H (2012) A moving mesh finite volume interface tracking method for surface tension dominated interfacial fluid flow. Comput Fluids 55:70–84
Unger EC et al (2004) Therapeutic applications of lipid-coated microbubbles. Adv Drug Delivery Rev 56:1291–1314
van der Meer SM et al (2007) Microbubble spectroscopy of ultrasound contrast agents. J Acoust Soc Am 121:648–656
van Wamel A et al (2006) Vibrating microbubbles poking individual cells: drug transfer into cells via sonoporation. J Control Release 112:149–155
Versluis M (2010) Nonlinear behavior of ultrasound contrast agent microbubbles and why shell buckling matters. In: Proceedings of 20th International Congress on Acoustics, Sydney, Australia
Vykhodtseva N, McDannold N, Hynynen K (2008) Progress and problems in the application of focused ultrasound for blood–brain barrier disruption. Ultrasonics 48:279–296
Weller HG et al (1998) A tensorial approach to computational continuum mechanics using object-oriented techniques. Comput Phys 12:620–631
Wiedemair W et al (2012) On ultrasound-induced microbubble oscillation in a capillary blood vessel and its implications for the blood–brain barrier. Phys Med Biol 57:1019–1045
Wiedemair W et al (2014) Modeling the interaction of microbubbles: effects of proximity, confinement, and excitation amplitude. Phys Fluids 26:062106 [1994-present]
Wu JR (2002) Theoretical study on shear stress generated by microstreaming surrounding contrast agents attached to living cells. Ultrasound Med Biol 28:125–129
Ye T, Bull JL (2006) Microbubble expansion in a flexible tube. J Biomech Eng T Asme 128:554–563
Zhang Y et al (2006) Porcine brain microvessel endothelial cells as an in vitro model to predict in vivo blood–brain barrier permeability. Drug Metab Dispos 34:1935–1943
Acknowledgments
The authors gratefully acknowledge the funding of this research by the Swiss National Science Foundation through NCCR Co-Me and NCCR Kidney.CH.
Author information
Authors and Affiliations
Corresponding author
Appendix: Validation of the IFT algorithm
Appendix: Validation of the IFT algorithm
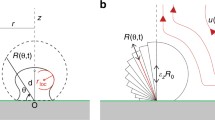
An IFT algorithm with a modified pressure boundary condition according to Eq. (7) is employed in this study to model the dynamics of a non-spherically oscillating encapsulated MB immersed in liquid. It allows for variations of \(\sigma _{s}\) and \(\mu _{s}\) as a function of MB size, including abrupt changes at shell breakup or during buckling. This algorithm is validated with respect to analytical predictions from Eq. (5).
Comparison of radius response curves from theoretical predictions and numerical results for a configuration with \(f_{\mathrm{ex}} = 2.9\) MHz, \(P_{\mathrm{ex}} = 130\) kPa, \(\kappa _{s} = 15\, \hbox {nN}\, \hbox {s}\, \hbox {m}^{-1},\, \chi = 1\, \hbox {N}\, \hbox {m}^{-1}\) and \(\tilde{a} = \hbox {a}_{0} = 0.975\, \upmu \hbox {m}\). The numerically determined a(t) shows excellent agreement with the analytical prediction, having a relative deviation of less than 0.45 %
The validation setup comprises a single MB of equilibrium radius \(a_{0} = 0.975\, \upmu \hbox {m}\) with variable settings for \(\kappa _{s}\) and \(\chi \). This MB is enclosed in a fluid sphere of radius \(R_{l} = 100\, \upmu \hbox {m}\), mimicking an infinitely large liquid envelope. The liquid is considered to be water with \(\rho _{l} = 1000\, \hbox {kg}\, \hbox {m}^{-3}\) and \(\mu _{l} = 10^{-3}\, \hbox {kg}\, \hbox {m}^{-1}\, \hbox {s}^{-1}\). This setup is exposed to a transient pressure field at various excitation frequencies \(f_{\mathrm{ex}}\) and either constant or linearly growing excitation amplitude \(P_{\mathrm{ex}}\).
In a first step, the conformity with predictions in the elastic regime and for buckling is established. The maximum tension that the shell can sustain is set to \(\sigma _{c} = 1\, \hbox {N}\, \hbox {m}^{-1}\), which is deliberately high to preclude shell rupture at this stage of the validation process. Figure 9 shows a comparison between the transient radius plots acquired with IFT and predicted by the modified RPE in Eq. (5) for the oscillation of a MB driven by an US field of \(f_{ex} = 2.9\) MHz and \(P_{\mathrm{ex}} = 130\) kPa. The shell properties were chosen to fit a SonoVue\(^{{\circledR }}\) UCA with \(\kappa _{s }= 15\, \hbox {nN}\, \hbox {s}\, \hbox {m}^{-1}\), \(\chi = 1\, \hbox {N}\, \hbox {m}^{-1}\) and \(\tilde{a} = a_{0} = 0.975\, \upmu \hbox {m}\) (Marmottant et al. 2005). We quantify the conformity between the numerical and the analytical results using the maximum of the transient relative difference
where \(a_{{a}}(t)\) represents the transient analytically determined MB radius and \(a_{n}(t)\) represents the transient numerically determined MB radius, while \(a_{a,\max }\) and \(a_{a,\min }\) denote the overall maximum and minimum of \(a_{a}(t)\). The analytically predicted and the numerically modelled comportments show excellent agreement with \(\varepsilon _{\mathrm{max}} = 0.45\) % in a simulation interval of 10 \(\upmu \hbox {s}\). The numerically acquired data also closely correspond to the results based on simulations using the same parameters published by Marmottant et al. (2005). As expected, the radius pattern exhibits compression preference (de Jong et al. 2007; Versluis 2010) and a change in slope during contraction.
Comparison between numerical results and analytical prediction for shell break up of two MBs with viscoelastic encapsulation of \(a_{0} = 0.975\, \upmu \hbox {m}\) and \(\tilde{a} = 0.95\, \upmu \hbox {m}\). An encapsulated MB of \(\kappa _{s} = 7.2\, \hbox {nN}\, \hbox {s}\, \hbox {m}^{-1}\), \(\chi = 0.55\, \hbox {N}\, \hbox {m}^{-1}\), \(\sigma _{c} = 0.0615\, \hbox {N}\, \hbox {m}^{-1}\) and \(\mu _{r} = 0.4\, \mu _{s}\) (top) exposed to \(f_{\mathrm{ex}} = 1.5\) MHz, \(P_{\mathrm{ex},i} = 100\) kPa and \(P_{\mathrm{ex},f} = 130\) kPa with \(\Delta t_{r} = 5\, \upmu \hbox {s}\) shows breakup at 3.48 \(\upmu \hbox {s}\). Another MB of \(\kappa _{s }= 15\, \hbox {nN}\, \hbox {s}\, \hbox {m}^{-1}\), \(\chi = 1\, \hbox {N}\, \hbox {m}^{-1}\), \(\sigma _{c} = 0.148\, \hbox {N}\, \hbox {m}^{-1}\) and \(\mu _{r} = 0.4\, \mu _{s}\) breaks up at 4.92 \(\upmu \hbox {s}\) when excited with \(f_{\mathrm{ex}} = 2.9\) MHz, \(P_{\mathrm{ex},i} = 150\) kPa and \(P_{\mathrm{ex},f} = 210\) kPa with \(\Delta t_{r} = 5\, \upmu \hbox {s}\). Both cases show close agreement between analytical prediction and numerical results
After checking the predictive capability of the numerical model for the elastic regime and the buckling state, we examine its ability to model shell rupture. To achieve a transition from oscillation with encapsulation to oscillation without encapsulation, \(P_{\mathrm{ex}}\) is ramped up from an initial \(P_{\mathrm{ex},i}\) to a final value \(P_{\mathrm{ex},f}\) over a time interval \(\Delta t_{r}\) and stays constant at \(P_{\mathrm{ex},f}\) for \(t > \Delta t_{r}\). Figure 10 displays a portion of the radius–time curves for two configurations with the instants of breakup indicated by arrows. Both encapsulated MBs have a buckling radius of \(\tilde{a} = 0.95\, \upmu \hbox {m}\).
The top panel of Fig. 10 shows results obtained for \(f_{\mathrm{ex}} = 1.5\) MHz, pressure amplitude buildup from \(P_{\mathrm{ex},i} = 100\) kPa to \(P_{\mathrm{ex},f} = 130\) kPa over \(\Delta t_{r} = 5\, \upmu \hbox {s}\) and shell properties of \(\kappa _{s} = 7.2\, \hbox {nN}\, \hbox {s}\, \hbox {m}^{-1},\, \chi = 0.55\, \hbox {N}\, \hbox {m}^{-1}\) (Gorce et al. 2000), \(\sigma _{c} = 0.0615\, \hbox {N}\, \hbox {m}^{-1}\) and \(\mu _{r} = 0.4\, \mu _{s}\). The shell’s breakup tension is surpassed at \(P_{\mathrm{ex}} = 121\) kPa and \(t_{b} = 3.48\, \upmu \hbox {s}\), after which the oscillation amplitude still keeps growing with increasing \(P_{\mathrm{ex}}\). \(\varepsilon _{\mathrm{max}}\) in the elastic regime does not surpass 0.6 % and peaks at 1.9 % after shell breakup.
Figure 10 (bottom) displays findings for the oscillation of a MB with \(f_{ex} = 2.9\, \hbox {MHz},\) \(P_{\mathrm{ex},i} = 150\, \hbox {kPa},\, P_{\mathrm{ex},f} = 210\, \hbox {kPa},\, \Delta t_{r} = 5\, \upmu \hbox {s}\), \(\kappa _{s }= 15 \hbox {nN}\, \hbox {s}\, \hbox {m}^{-1}\), \(\chi = 1\, \hbox {N}\, \hbox {m}^{-1}\), \(\sigma _{c} = 0.148\, \hbox {N}\, \hbox {m}^{-1}\) and \(\mu _{r} = 0.4\,\mu _{s}\). Shell breakup occurs at 4.92 \(\upmu \hbox {s}\) and \(P_{\mathrm{ex}} = 209\) kPa. Subsequently, a(t) quickly stabilizes to a new pattern with constant amplitude. \(\varepsilon _{\mathrm{max}}\) in the elastic regime does not surpass 0.4 % and increases to 2.4 % after shell breakup.
All three presented setups show an agreement between numerical results and analytical predictions with a difference below 1 % before shell rupture and lower than 2.5 % after rupture.
Rights and permissions
About this article
Cite this article
Wiedemair, W., Tukovic, Z., Jasak, H. et al. The breakup of intravascular microbubbles and its impact on the endothelium. Biomech Model Mechanobiol 16, 611–624 (2017). https://doi.org/10.1007/s10237-016-0840-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10237-016-0840-z