Abstract
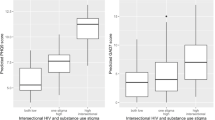
Little is known about the intersection of HIV stigma and substance use stigma. Using data from 188 HIV-positive people who inject drugs (PWID) in Russia, we examined the associations of these stigmas and their interaction with access and utilization of healthcare. While substance use stigma was significantly associated with poor access to care (AOR 2.31, 95%CI 1.50–3.57), HIV stigma was not. HIV stigma was associated with lower inpatient care utilization (AOR 0.32, 95%CI 0.14–0.65), while substance use stigma was not. We did not detect a significant interaction between the two forms of stigma for either of the primary outcomes. However, those with high levels of both substance use stigma and HIV stigma had higher odds of poor general access to healthcare (AOR 1.86, 95%CI 1.19–2.92), and lower odds of recent general outpatient (AOR 0.52, 95%CI 0.32–0.85) and any inpatient (AOR 0.48, 95%CI 0.22–0.99) care utilization compared to those with low levels of both types of stigma. Interventions addressing both substance use and HIV stigma in general healthcare settings might improve care in this HIV key population.
Similar content being viewed by others
References
Levi J, Raymond A, Pozniak A, Vernazza P, Kohler P, Hill A. Can the UNAIDS 90-90-90 target be achieved? A systematic analysis of national HIV treatment cascades. BMJ Glob Health. 2016;1:1–10.
Heimer R. The policy-driven HIV epidemic among opioid users in the Russian Federation. Curr HIV/AIDS Rep. 2018;15:259–65.
Federal Service for Surveillance on Consumer Rights Protection and Human Wellbeing. Gosudarstvennyy doklad “O sostoyanii sanitarno-epidemiologicheskogo blagopoluchiya naseleniya v Rossiyskoy Federatsii v 2017 godu” [Internet]. 2018. Available from: http://rospotrebnadzor.ru/documents/details.php?ELEMENT_ID=10145.
UNAIDS. 90-90-90 An ambitious treatment target to help end the AIDS epidemic. 2014;40. http://www.unaids.org/sites/default/files/media_asset/90-90-90_en_0.pdf.
Sarang A, Rhodes T, Sheon N. Systemic barriers accessing HIV treatment among people who inject drugs in Russia: a qualitative study. Health Policy Plan. 2013;28:681–91. https://doi.org/10.1093/heapol/czs107.
Bikmuhametov DA. Ways to optimize and improve the quality of medical services for people with HIV in the AIDS Centres of the Russian Federation. Moscow: FIP (in Russian) [Internet]. Found. Intersectoral Partnersh. 2009. Available from: https://spdfund.org/wp-content/uploads/survey_report200911.pdf 13. September 2019.
Ministry of Health of Russian Federation. Modern approaches in organization medical and social rehabilitation of patients with substance use disorder. Clinical guidelines (in Russian) [Internet]. 2013;1–7. Available from: http://r-n-l.ru/documents/minzdravmet2013.pdf.
Kirzhanova VV, Grigorova NI, Kirzhanov VN, Sidoryuk OV. The main outcomes of the narcological care in Russian Federation in 2015–2016: statistical bulletin. FSBI « Serbsky FMSCPN» Minist Heal Russ Fed. 2017.
Kelly J, Amirkhanian Y, Yakovlev A, Musatov V, Meylakhs A, Kuznetsova A, et al. Stigma reduces and social support increases engagement in medical care among persons with HIV infection in St. Petersburg, Russia. J Int AIDS Soc. 2014;17:19618. https://doi.org/10.7448/IAS.17.4.19618.
Corrigan PW, Nieweglowski K. Stigma and the public health agenda for the opioid crisis in America. Int J Drug Policy. 2018;59:44–9. https://doi.org/10.1016/j.drugpo.2018.06.015.
Link BG, Phelan JC. Conceptualizing stigma. Annu Rev Sociol. 2001;27:363–85.
Turan JM, Elafros MA, Logie CH, Banik S, Turan B, Crockett KB, et al. Challenges and opportunities in examining and addressing intersectional stigma and health. BMC Med. 2019;17:1–15.
Earnshaw VA, Smith LR, Cunningham CO, Copenhaver MM. Intersectionality of internalized HIV stigma and internalized substance use stigma: implications for depressive symptoms. J Health Psychol. 2015;20:1083–9.
Nartova N, Yasaveyev I, Shilova A. People living with HIV and HIV activists (St. Petersburg & Kazan) Russia. PROMISE Promot Youth Involv Soc Engagem Oppor challenges conflicted young people across Eur. 2018.
Crenshaw K. Mapping the margins: intersectionality, identity politics, and violence against women of color. Stanford Law Rev. 1991;43:1241–99.
Earnshaw VA, Chaudoir SR. From conceptualizing to measuring HIV stigma : a review of HIV stigma mechanism measures. AIDS Behav. 2009;13:1160–77.
Kelly J, Amirkhanian Y, Yakovlev A, Musatov V, Meylakhs A, Kuznetsova A, et al. Stigma reduces and social support increases engagement in medical care among persons with HIV infection in St. Petersburg, Russia. J Int AIDS Soc. 2014;17:19618.
King EJ, Maman S, Bowling JM, Moracco KE, Dudina V. The influence of stigma and discrimination on female sex workers’ access to HIV services in St. Petersburg, Russia. AIDS Behav. 2013;17:2597–603.
Steward WT, Herek GM, Ramakrishna J, Bharat S, Chandy S, Wrubel J, et al. HIV-related stigma: adapting a theoretical framework for use in India. Soc Sci Med. 2008;67:1225–35.
Ekstrand ML, Bharat S, Srinivasan K. HIV stigma is a barrier to achieving 90-90-90 in India. Lancet HIV. 2018;5:e543–5.
Bobrova N, Alcorn R, Rhodes T, Rughnikov I, Neifeld E, Power R. Injection drug users’ perceptions of drug treatment services and attitudes toward substitution therapy: a qualitative study in three Russian cities. J Subst Abuse Treat. 2007;33:373–8.
Stringer KL, Marotta P, Baker E, Turan B, Kempf MC, Drentea P, et al. Substance use stigma and antiretroviral therapy adherence among a drug-using population living with HIV. AIDS Patient Care STDS. 2019;33:282–93.
Burke SE, Calabrese SK, Dovidio JF, Levina OS, Uusküla A, Niccolai LM, et al. A tale of two cities: stigma and health outcomes among people with HIV who inject drugs in St. Petersburg, Russia and Kohtla-Järve, Estonia. Soc Sci Med. 2015;130:154–61. https://doi.org/10.1016/j.socscimed.2015.02.018.
Amirkhanian YA, Kelly JA, DiFranceisco WJ, Kuznetsova AV, Tarima SS, Yakovlev AA, et al. Predictors of HIV care engagement, antiretroviral medication adherence, and viral suppression among people living with HIV infection in St. Petersburg, Russia. AIDS Behav. 2018;22:791–9.
Rice WS, Crockett KB, Mugavero MJ, Raper JL, Atkins GC, Turan B. Association between internalized HIV-related stigma and HIV care visit adherence. J Acquir Immune Defic Syndr. 2017;76:482–7.
So-Armah KA, Cheng DM, Freiberg MS, Gnatienko N, Patts G, Ma Y, et al. Association between alcohol use and inflammatory biomarkers over time among younger adults with HIV—the Russia ARCH Observational Study. PLoS ONE. 2019;14:e0219710.
Weatherby NL, Needle R, Cesari H, Booth R, McCoy CB, Watters JK, et al. Validity of self-reported drug use among injection drug users and crack cocaine users recruited through street outreach. Eval Program Plann. 1994;17:347–55.
Needle R, Fisher DG, Weatherby N, Chitwood D, Brown B, Cesari H, et al. Reliability of self-reported HIV risk behaviors of drug users. Psychol Addict Behav. 1995;9:242–50.
Berger BE, Ferrans CE, Lashley FR. Measuring stigma in people with HIV: psychometric assessment of the HIV stigma scale. Res Nurs Health. 2001;24:518–29.
Wright K, Naar-King S, Lam P, Templin T, Frey M. Stigma scale revised: reliability and validity of a brief measure of stigma for HIV+ youth. J Adolesc Health. 2007;40:96–8.
Pantelic M, Boyes M, Cluver L. ‘They say HIV is a punishment from God or from Ancestors’: cross-cultural adaptation and psychometric assessment of an HIV stigma scale for South African adolescents living with HIV (ALHIV-SS). Child Indic Res. 2018;11:207–23.
Luoma JB, Nobles RH, Drake CE, Hayes SC, O’Hair A, Fletcher L, et al. Self-stigma in substance abuse: development of a new measure. J Psychopathol Behav Assess. 2013;35:223–34.
Luoma JB, Twohig MP, Waltz T, Hayes SC, Roget N, Padilla M, et al. An investigation of stigma in individuals receiving treatment for substance abuse. Addict Behav. 2007;32:1331–46.
Cunningham WE, Hays RD, Williams KW, Beck KC, Dixon WJ, Shapiro MF. Access to medical care and health-related quality of life for low-income persons with symptomatic human immunodeficiency virus. Med Care. 1995;33:739–54.
Sayles JN, Wong MD, Kinsler JJ, Martins D, Cunningham WE. The Association of stigma with self-reported access to medical care and antiretroviral therapy adherence in persons living with HIV/AIDS. J Gen Intern Med. 2009;24:1101–9.
Chishinga N, Kinyanda E, Weiss HA, Patel V, Ayles H, Seedat S. Validation of brief screening tools for depressive and alcohol use disorders among TB and HIV patients in primary care in Zambia. BMC Psychiatry. 2011. https://doi.org/10.1186/1471-244X-11-75.
Radloff LSLS. The CES-D scale: a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1:385–401.
Fleishman JA, Sherbourne CD, Crystal S, Collins RL, Marshall GN, Kelly M, et al. Coping, conflictual social interactions, social support, and mood among HIV-infected persons. HCSUS Consortium. Am J Community Psychol. 2000;28:421–53.
Saunders JB, Aasland OG, Babor TF, et al. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption—II. Addiction. 1993;88:791–803.
Sobell LC, Sobell MB, Leo GI, Cancilla A. Reliability of a Timeline Method: assessing normal drinkers’ reports of recent drinking and a comparative evaluation across several populations. Br J Addict. 1988;83:393–402.
Justice AC, Holmes W, Gifford AL, Rabeneck L, Zackin R, Sinclair G, et al. Development and validation of a self-completed HIV symptom index. J Clin Epidemiol. 2001;54:8–10.
Kazis LE, Miller DR, Clark JA, Skinner KM, Lee A, Ren XS, et al. Improving the response choices on the veterans SF-36 health survey role functioning scales: results from the veterans health study. J Ambul Care Manag. 2004;27:263–80.
Lanza ST, Moore JE, Butera NM. Drawing causal inferences using propensity scores: a practical guide for community psychologists. Am J Community Psychol. 2013;52:380–92.
Stürmer T, Wyss R, Glynn RJ, Brookhart MA. Propensity scores for confounder adjustment when assessing the effects of medical interventions using nonexperimental study designs. J Intern Med. 2014;275:570–80.
Open Society Institute. The effects of drug user registration laws on people’s rights and health: Key findings from Russia, Georgia and Ukraine [Internet]. 2009. Available from: https://idpc.net/publications/2009/11/osi-report-drug-user-registration.
Vetrova MV, Toussova OV, Blokhina EA, Bushara NM, Idrisov B, Bendiks S, et al. A-AIDS2020-03634 Public or private—which way to go? A qualitative study of HIV-positive patients’ navigation of addiction care in Saint Petersburg, Russia. 23rd Int AIDS Conf 6–10 July 2020 [Internet]. 2020; Available from: https://cattendee.abstractsonline.com/meeting/9289/Presentation/2037.
Bobrova N, Sarang A, Stuikyte R, Lezhentsev K. Obstacles in provision of anti-retroviral treatment to drug users in Central and Eastern Europe and Central Asia: a regional overview. Int J Drug Policy. 2007;18:313–8.
Sarang A, Rhodes T, Sheon N. Systemic barriers accessing HIV treatment among people who inject drugs in Russia: a qualitative study. Health Policy Plan. 2013;28:681–91.
Lunze K, Raj A, Cheng DM, Quinn EK, Bridden C, Blokhina E, et al. Punitive policing and associated substance use risks among HIV-positive people in Russia who inject drugs. J Int AIDS Soc. 2014;17:1–7.
Gunn AJ, Sacks TK, Jemal A. “That’s not me anymore”: resistance strategies for managing intersectional stigmas for women with substance use and incarceration histories. Qual Soc Work. 2018;17:490–508.
Calabrese SK, Burke SE, Dovidio JF, Levina OS, Uusküla A, Niccolai LM, et al. Internalized HIV and drug stigmas: interacting forces threatening health status and health service utilization among people with HIV who inject drugs in St. Petersburg, Russia. AIDS Behav. 2016;20:85–97.
Kiriazova T, Lunze K, Raj A, Bushara N, Blokhina E, Krupitsky E, et al. “It is easier for me to shoot up”: stigma, abandonment, and why HIV-positive drug users in Russia fail to link to HIV care. AIDS Care. 2017;29:559–63. https://doi.org/10.1080/09540121.2016.1259451.
Ding L, Landon BE, Wilson IB, Wong MD, Shapiro MF, Cleary PD. Predictors and consequences of negative physician attitudes toward HIV-infected injection drug users. Arch Intern Med. 2005;165:618–23.
Bobrova N, Rhodes T, Power R, Alcorn R, Neifeld E, Krasiukov N, et al. Barriers to accessing drug treatment in Russia: a qualitative study among injecting drug users in two cities. Drug Alcohol Depend. 2006;82:57–63.
Toussova O, Vetrova M, Blokhina E, Bushara N, Bendiks S, Gnatienko N, et al. Dual stigma affecting HIV-positive PWID in Russia: a qualitative study [Internet]. San Diego, USA; 2018. Available from: https://www.drugabuse.gov/international/abstracts/double-stigma-among-hiv-positive-people-who-inject-drugs-in-russia-hiv-care-qualitative-study.
Biancarelli D, Biello K, Childs E, Drainoni M-L, Salhaney P, Edeza A, et al. Strategies used by people who inject drugs to avoid stigma in healthcare settings. Drug Alcohol Depend. 2018. https://doi.org/10.1016/j.drugalcdep.2019.01.037.
Van Boekel LC, Brouwers EPM, Van Weeghel J, Garretsen HFL, Van BLC, Brouwers EPM, et al. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: systematic review. Drug Alcohol Depend. 2013;131:23–35. https://doi.org/10.1016/j.drugalcdep.2013.02.018.
Pantelic M, Steinert JI, Park J, Mellors S, Murau F. “Management of a spoiled identity”: systematic review of interventions to address self-stigma among people living with and affected by HIV. BMJ Glob Health. 2019;4:e001285.
Ikeda DJ, Nyblade L, Srithanaviboonchai K, Agins BD. A quality improvement approach to the reduction of HIV-related stigma and discrimination in healthcare settings. BMJ Glob Health. 2019;4:1–9.
Acknowledgements
The authors thank the Russia ARCH participants and the contributions of the staff at St. Petersburg AIDS Center who help with recruitment, in particular Ludmila Gutova and research staff who conducted the assessments, in particular Vladimir Palatkin, Tatiana Yaroslavtseva and Janna Vasylieva, and study nurse, Anna Kazishvili. This work was supported by grants from National Institute on Drug Abuse: K99DA041245,4R00DA041245, 2018 National Institute on Drug Abuse (NIDA) International Visiting Scientists and Technical Exchange Program (INVEST) and by grants from the National Institute on Alcohol Abuse and Alcoholism (NIAAA) in support of URBAN ARCH: U24AA020778, U24AA020779, U01AA0020780, U01AA021989, and the Providence/Boston Center for AIDS Research (P30AI042853).
Author information
Authors and Affiliations
Contributions
KL conceived of this study and secured funding. MVV and KL drafted the paper. DMC guided the analytic approach, CL-T, and WJ conducted statistical analyses. SB, NG, EB, EK, and DL provided assistance with study implementation and data collection. JL, ME, AR, and JHS provided input to the analytic plan and data interpretation. All authors revised the manuscript draft for important intellectual content. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The content is solely the responsibility of the authors and does not represent the official views of the National Institutes of Health. No conflicting financial interests exist.
Ethical Approval
Institutional Review Boards of Boston University Medical Campus and First St. Petersburg Pavlov State Medical University approved this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vetrova, M.V., Cheng, D.M., Bendiks, S. et al. HIV and Substance Use Stigma, Intersectional Stigma and Healthcare Among HIV-Positive PWID in Russia. AIDS Behav 25, 2815–2826 (2021). https://doi.org/10.1007/s10461-021-03172-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10461-021-03172-5