Abstract
In the United Kingdom, current screening guidelines for TP53 germline mutation carriers solely recommends annual breast MRI, despite the wide spectrum of malignancies typically seen in this group. This study sought to investigate the role of one-off non-contrast whole-body MRI (WB MRI) in the screening of asymptomatic TP53 mutation carriers. 44 TP53 mutation carriers and 44 population controls were recruited. Scans were read by radiologists blinded to participant carrier status. The incidence of malignancies diagnosed in TP53 mutation carriers against general population controls was calculated. The incidences of non-malignant relevant disease and irrelevant disease were measured, as well as the number of investigations required to determine relevance of findings. In TP53 mutation carriers, 6 of 44 (13.6, 95% CI 5.2–27.4%) participants were diagnosed with cancer during the study, all of which would be considered life threatening if untreated. Two were found to have two primary cancers. Two participants with cancer had abnormalities on the MRI which were initially thought to be benign (a pericardial cyst and a uterine fibroid) but transpired to be sarcomas. No controls were diagnosed with cancer. Fifteen carriers (34.1, 95% CI 20.5–49.9%) and seven controls (15.9, 95% CI 6.7–30.1%) underwent further investigations following the WB MRI for abnormalities that transpired to be benign (p = 0.049). The cancer detection rate in this group justifies a minimum baseline non-contrast WB MRI in germline TP53 mutation carriers. This should be adopted into national guidelines for management of adult TP53 mutation carriers in addition to the current practice of contrast enhanced breast MRI imaging.
Similar content being viewed by others
Introduction
Li-Fraumeni Syndrome (LFS) is a rare autosomal dominant condition which predisposes individuals to numerous cancer types. The majority of families with LFS have been found to carry mutations in the TP53 gene [1–3]. Typical cancers in the Li-Fraumeni spectrum include soft tissue and bone sarcoma, breast, brain, adrenal cortical carcinoma and leukaemia [4], however an increased risk has also been found in many other cancer types [5, 6]. The cancers are typically young onset occurring 2 or 3 decades before the median in the general population [6], and individuals are predisposed to multiple malignancies [7]. The condition has a high penetrance, with a lifetime cancer risk of almost 100% for females and 75% for males [8] and may have a birth incidence as high as 1 in 5000 [9].
In the United Kingdom, the National Institute for Health and Clinical Excellence (NICE) recommends annual breast MRI from age 20–49 years for female TP53 mutation carriers and to consider continuation of breast screening past age 50. Discussion of risk-reducing mastectomy is also recommended, however, no other surveillance is currently suggested in any guidelines. Screening across UK genetics centres varies and many employ an open-door policy for carriers experiencing symptoms.
Recent evidence suggests there may be a survival benefit with more intensive screening, including whole-body MRI (WB MRI) [10, 11]. Internationally, more intensive screening programmes are starting to become employed [12, 13] and, in particular, are being explored in the research setting [10, 14–16]. Several studies are employing WB MRI [14, 17], others FDG-PET/CT [15, 16], and, most commonly, combinations of several physical examination, imaging and biochemical screening modalities [10, 14, 17]. Given the lack of radiation, WB MRI provides an attractive choice to screen this cohort of individuals with an increased susceptibility to radiation-induced neoplasms [18, 19].
When considering a screening modality, the incidence of incidental findings is important in decision making whether to adopt the modality in guidelines. To our knowledge, no studies have employed a healthy control group to compare the incidence of malignancies and incidental findings to that found in the TP53 mutation carriers.
This pilot study aimed to assess the incidence of malignancies diagnosed in asymptomatic TP53 mutation carriers using a non-contrast WB MRI against general population controls, as well as the incidences of non-malignant relevant and irrelevant disease and the investigations required to determine relevance. It was hypothesised that more malignancies would be diagnosed in the TP53 mutation carrier cohort than in the controls and the ratio of relevant to non-relevant findings (relevant defined as needing definitive treatment) would be higher in the TP53 mutation carriers than controls.
Methods
Study subjects and data collection
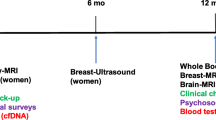
From November 2012 through July 2016, TP53 mutation carriers were recruited through genetics services from across the United Kingdom and general population controls through local advertisements. Carriers with a known low penetrance TP53 mutation (in the view of a geneticist) or a variant of unknown significance were excluded, as well as those with a malignancy diagnosed in the previous 5 years [except non-melanomatous skin cancer or cervical carcinoma in situ (CIS)]. Population controls were sex and age (±5 years) matched to carriers and required to have no personal history of cancer (except non-melanomatous skin cancer or cervical CIS) and minimal family history of cancer (no first degree relative diagnosed before age 50 and only one first, second or third degree relative diagnosed at any age). Any person with current symptoms suggestive of malignancy was excluded.
An additional sub-study was included to examine the psychosocial impact of screening in this group of high-risk individuals, the results of which will be reported separately.
The research was approved by the Health Research Authority NRES Committee London—Brent (12/LO/0781).
MRIs
MRI examinations were performed at The Royal Marsden NHS Foundation Trust or Central Manchester University Hospitals NHS Foundation Trust using a 1.5 T MRI machine (Siemens, Erlangen, Germany) from vertex to feet using conventional MR imaging sequences (T1-weighted, with or without fat suppressed T2-weighted/STIR sequences), as well as diffusion weighted images (Supplementary Table 1). Slices were 0.8 cm thick and scans were not contrast enhanced. Comparisons of imaging techniques will be reported elsewhere.
Scans were read independently by two radiologists with at least 5 years’ experience, who were blinded to the mutation status of the study participants. MRIs were divided into anatomical sections and each section scored 0 to 5 (0 normal findings, 1 definitely benign, 2 likely to be benign, 3 equivocal, 4 likely to be malignant, 5 definitely malignant). Initial recommendations for further investigations were made blinded to carrier status, however subsequent review and intervention was made with consideration of this factor. In a case of discrepancy a consensus reading was performed by the two study radiologists plus a radiologist from the other centre. Ten percent of scans, selected randomly, were cross-read at both centres for quality assurance. Lesions requiring investigation and incidental findings were discussed in a cross centre video-linked multidisciplinary team (MDT) meeting including PIs, radiologists and other study staff from both sites. All pathology was reviewed by expert pathologists in two tertiary cancer centres and at tumour-specific MDT meetings.
Sample size and statistical analysis
A total of 88 participants were recruited to the study, with 44 carriers of TP53 mutations matched to 44 healthy population controls. This sample size was calculated for 80% power to detect a difference in cancer detection between the mutation carrier group and the control group assuming a 20% cancer detection rate in the carrier group and 1% in the control group for a two-tailed analysis.
The efficacy of WB MRI as a screening tool was evaluated by diagnosis of early stage malignancy in asymptomatic individuals, with respect to the number of further investigations required and false positives. Incidence of malignancies with 95% confidence intervals was calculated in both carrier and control groups and any difference between groups was compared using Chi square or Fisher’s exact test as appropriate at a 5% significance level. The incidence of and proportion of the cohort with relevant and non-relevant MRI findings is reported with 95% confidence intervals. Of those who were recalled, additional investigations with non-malignant results were reported with 95% confidence intervals and any difference between groups assessed using Mann–Whitney test. All statistical tests were two-sided and analysis was performed using STATA [20].
Results
Patient characteristics
Forty-four TP53 mutation carriers from 37 families and 44 matched healthy population controls were recruited (Table 1). Nine of the 27 female TP53 carriers had had risk-reducing surgery of some kind, or mastectomies for previous breast cancer.
Cancer diagnoses and treatments
In TP53 mutation carriers, six of 44 (13.6, 95% CI 5.2–27.4%) participants were diagnosed with cancer during the study (Table 2). Only four (9.1, 95% CI 2.5–21.7%) of these were a direct result of the study WB MRI, however two participants had two simultaneous primary tumours diagnosed. There was no diagnosis of cancer in the control group. Analysis showed no statistically significant difference in number of TP53 mutation carriers diagnosed with malignancy compared to controls (p = 0.116), however the study was powered at a higher cancer detection rate in TP53 mutation carriers. Table 3.
All four individuals with screen detected cancers were women who were asymptomatic and all were treated with curative intent.
The first woman had a low grade astrocytoma in the right inferior temporal gyrus and underwent a R0 resection with full post-operative recovery 2 years after surgery. Upon questioning after her diagnosis she retrospectively reported episodes of déjà vu but no other symptoms and had never had a cancer diagnosis previously.
The second woman was diagnosed with a myxosarcoma in the abdominal wall (Trojani grade 2). The size was 46 × 37 mm and all margins were free indicating complete surgical excision. She did not require additional chemotherapy or radiotherapy. This patient had a previous cancer history of ovarian teratoma at age 4, phylloides tumour of the breast aged 41 and DCIS breast cancer at 42 and a fibrosarcoma of the left thigh at 42.
The third woman was 45 years of age and reported irregular menstrual cycle on enrolment. She had no history of cancer and was found to have a 10.6 × 8.6 cm mass of the right kidney on WB MRI. The differential diagnosis included an oncocytoma or renal cell carcinoma. Additionally, two uterine fibroids and an ovarian cyst were detected. Following renal CT and pelvic MRI, she underwent a right nephrectomy and given her carrier status and age, simultaneous total abdominal hysterectomy, right salpingectomy (right ovary previously excised) and left salpingo-oophorectomy. A 110 mm chromophobe renal cell carcinoma (Fuhrman grade 3) confined to the kidney with no lymphovascular invasion was detected, plus an incidental benign renal angiomyolipoma measuring 15 mm. In the resected uterus, 2 fibroids were present; the larger (65 mm) was found to be a leiomyosarcoma confined to the myometrium with no evidence of vascular invasion, and the smaller (25 mm) fibroid was a benign leiomyoma. The left ovary contained a benign cyst and interestingly both fallopian tube fimbrial ends were noted to contain scattered atypical epithelial cells with severe cytological atypia, thought to be more consistent with a tubal intra-epithelial lesion in transition rather than a definite serous intra-epithelial carcinoma. Both the uterine and renal tumour resections were R0 and no further treatment was required.
The fourth participant had previously had a rhabdomyosarcoma at 6 months of age. During the study, three tumours were detected, of which the first two (in the liver and right kidney) were detected on the initial WB MRI. Subsequent dedicated liver and renal MRIs were inconclusive but were strongly suspicious of malignancy. Resection of the lesions revealed epithelioid angiomyolipomas in both organs, with suspiciously high mitotic incidence, however their malignant potential was unclear, as was the synchronicity of the tumours. Given the rarity of angiomyolipomas, tuberous sclerosis was subsequently ruled out. While on follow up for these initial tumours, a new left sacroiliac lesion was detected 19 months after the initial WB MRI. This was initially monitored then biopsied, diagnosing a high-grade chondroblastic osteosarcoma. The patient has completed methotrexate, doxorubicin and cisplatin (MAP) chemotherapy; surgery has been advised but the patient is pursuing proton beam therapy in the USA.
An additional patient had a pericardial cyst (seen on WB MRI) that was initially reported as likely benign but became symptomatic and non-study dedicated MRI and biopsy revealed a mediastinal sarcoma. The sixth was diagnosed with B-cell acute lymphocytic leukaemia 9 months after his whole-body MRI. This patient’s WB MRI was negative and he only reported some upper abdominal discomfort when questioned on enrolment in the study.
Non-malignant findings from WB MRI
Outcomes of findings from the WB MRI are detailed in Table 2 with further details of all investigations in Supplementary Table 2. Fifteen carriers (34.1%, 95% CI 20.5–49.9%) and 7 controls (15.9%, 95% CI 6.7–30.1%) underwent further investigations after their WB MRI that did not result in a diagnosis of cancer (Table 5). There was a marginally significant difference between the groups (p = 0.049). Six carriers and one control had more than one follow-up investigation (Table 4). Of those who were recalled, TP53 mutation carriers on average had 2.33 (95% CI 1.17–3.50) additional investigations with non-malignant results and controls 1.14 (95% CI 0.79 to 1.49). There was no significant difference between groups (p = 0.101).
There was one case in a TP53 mutation carrier of a non-malignant incidental finding that needed intervention (triggering a rheumatology referral) and additionally three lesions in two TP53 mutation carriers are requiring continued surveillance given their genetic status (3 of 44, 6.8%; 95% CI 1.4–18.7%).
Eight investigations with non-malignant results (four CTs, two PET-CT scans and one X-ray) were carried out in five carriers using imaging techniques that exposed the participant to radiation (Table 5). However the majority of investigations conferred no exposure: most commonly, MRI imaging was used (13 scans in carriers and two in controls, either repeat scanning to monitor growth of the lesion, addition of contrast or more detailed imaging), then ultrasound (eight scans in carriers and six in controls). Two invasive procedures that did not result in a diagnosis of cancer were undertaken in carriers in the study: a biopsy of a suspicious pelvic bone lesion and the simultaneous salpingo-oophorectomy (for likely ovarian cyst) with nephrectomy and hysterectomy in the case of the chromophobe renal cell cancer.
Discussion
The SIGNIFY baseline WB MRI study demonstrates an overall cancer detection rate of 9.1% in prevalent WB MRI scans in TP53 mutation carriers with no cancers identified in controls (p = 0.116). The peak annual incidence rate for malignancy in TP53 mutation carriers is around 3% [21] therefore the prevalence in study of 9.1% suggests there is significant lead time in the cancers detected which indicates that such screening is likely to be effective in LFS. This would be further demonstrated by a low detection rate at a subsequent annual incident screens which remains to be proven. Similar findings of a high prevalent detection rate was found in the MARIBS study [22, 23] (which included TP53 mutation carriers) with 2.7% of 632 women detected with breast cancer at prevalent screen dropping to 1.2% at the first incident round. This has translated into a significant survival benefit in women undergoing breast MRI screening [22].
The detection rate at prevalent screen could have been higher at 11.3% if further dedicated MRI had been performed as part of the study to detect the mediastinal sarcoma that had presented with a pericardial fluid collection that appeared to be a benign cyst. Additionally, the seemingly benign appearance of the uterine leiomyosarcoma also argues for a lower threshold for suspicion in this high risk cohort. Although, further investigation of these apparent benign features would lead to a higher rate of subsequent radiological investigation, this may translate into higher tumour survival rates. Complete resection of a brain astrocytoma, abdominal wall sarcoma and liver, kidney and uterine tumours may not have been possible without presymptomatic MRI detection in the current study. Sarcomas and brain malignancy in TP53 mutation carriers have poor overall survival rates and without curative surgery patients gain little benefit from chemotherapy or radiotherapy [24–26]. Indeed the avoidance of radiotherapy through complete surgical excision may well prevent future radiation induced malignancy that appears to be very high in TP53 mutation carriers [18]. It is likely that annual WB MRI [10, 11] will be required as sarcomas in TP53 mutation carriers are often high grade and one patient already developed an osteosarcoma 19 months after a true negative prevalent scan.
Thus far if the missed mediastinal sarcoma and leukaemia are included, two symptomatic malignancies have developed in the 12-months post prevalent MRI. The leukaemia would not have been expected to be detected and further additional blood and other tests need to be considered in TP53 mutation carriers as occurs in the Toronto protocol [10, 11]. In particular we do not believe that WB MRI will replace dedicated breast MRI which requires a breast coil and gadolinium injection for the highest sensitivity [23]. This indicates that both screening measures will be needed in the management of TP53 mutation carriers. It is not yet known how often such scans should be undertaken; at present breast MRI is performed annually from 20 to 50 years, but further studies are needed to assess if WB MRI needs to be repeated annually concurrently.
There was a high rate of identification of incidental findings at WB MRI. More than twice as many TP53 mutation carriers required further investigation for incidental findings, resulting in a marginally significant difference between the groups (p = 0.049). Carriers who were recalled also had a higher number of repeat scans compared to controls, however this difference did not reach significance (p = 0.110). We are awaiting the psychological outcomes of these in a study related protocol, but this high rate of investigation including eight TP53 mutation carriers versus zero controls requiring modalities involving radiation for further investigation is of concern. Nonetheless the higher rate of these findings may presage future malignancy risk as evidenced by the finding of apparent benign cystic lesions in the bone and pericardium that were found to be tumour related.
This study only considered mutation carriers with mutations previously known to be of high penetrance and it is possible that the balance of incidental findings and relevant tumour detection may not be the same in those with low penetrance mutations, such as the Brazilian founder mutation [27]. The increase in use of gene panels in families or individuals with cancer without a history of classical LFS or LFL syndrome will identify more individuals with germline TP53 mutations where the penetrance may be lower and the role of WB MRI in such individuals is still uncertain.
LFS leads to tumours in both children and adults, however it was not possible to examine the role of screening children in the present study as the Ethics Committee passed the protocol to be undertaken in adults only. Furthermore, studies from Toronto have published the use of screening in the paediatric age group [10, 11].
The present study has some limitations. The study size was not sufficient to detect significant differences in tumour rates between cases and controls, but the trend of the data are compelling. Nonetheless the blinding of radiologists to cases and controls, the first time we are aware this has been done, is an obvious strength. In particular, the imaging of controls has demonstrated the incidental finding incidence in a small general population cohort. It is interesting that the rate of recall for further scans was higher in mutation carriers and there are animal data that suggest that mutation carriers may have dysmorphic features [28, 29]. It would be ideal to undertake an international meta-analysis of WB MRI data in TP53 mutation carriers.
The malignancy prevalence of 13.6% in this study, detection rate on initial MRI of 9.1% and two cases of simultaneous primary cancers in two participants all argue for the adoption of at least a baseline whole body MRI scan in the screening of TP53 mutation carriers. Given the rarity of this condition and the relative ease of delivery of MRI without contrast, this additional screen warrants further research prior to incorporation into national guidelines for management of adult TP53 mutation carriers in addition to the current practice of gadolinium enhanced breast MRI imaging.
References
Varley JM, McGown G, Thorncroft M et al (1997) Germ-line mutations of TP53 in Li-Fraumeni families: an extended study of 39 families. Cancer Res 57(15):3245–3252
Varley JM (2003) Germline TP53 mutations and Li-Fraumeni syndrome. Hum Mutat 21(3):313–320. doi: 10.1002/humu.10185
Malkin D, Li FP, Strong LC et al (1990) Germ line p53 mutations in a familial syndrome of breast cancer, sarcomas, and other neoplasms. Science 250(4985):1233–1238
Li FP, Fraumeni JF Jr (1969) Soft-tissue sarcomas, breast cancer, and other neoplasms. A familial syndrome? Ann Intern Med 71(4):747–752
Gonzalez KD, Noltner KA, Buzin CH et al (2009) Beyond li fraumeni syndrome: clinical characteristics of families with p53 germline mutations. J Clin Oncol 27(8):1250–1256
Nichols KE, Malkin D, Garber JE, Fraumeni JF Jr, Li FP (2001) Germ-line p53 mutations predispose to a wide spectrum of early-onset cancers. Cancer Epidemiol Biomarkers Prev 10(2):83–87
Hisada M, Garber JE, Fung CY, Fraumeni JF Jr, Li FP (1998) Multiple primary cancers in families with Li-Fraumeni syndrome. J Natl Cancer Inst 90(8):606–611
Mai PL, Best AF, Peters JA et al (2016) Risks of first and subsequent cancers among TP53 mutation carriers in the National Cancer Institute Li-Fraumeni syndrome cohort. Cancer. 122(23): 3673–3681. doi: 10.1002/cncr.30248
Lalloo F, Varley J, Ellis D, et al. (2003) Prediction of pathogenic mutations in patients with early-onset breast cancer by family history. Lancet (London, England) 361(9363): 1101–1112 doi: 10.1016/s0140-6736(03)12856-5
Villani A, Shore A, Wasserman JD et al (2016) Biochemical and imaging surveillance in germline TP53 mutation carriers with Li-Fraumeni syndrome: 11 year follow-up of a prospective observational study. The Lancet Oncol. doi: 10.1016/S1470-2045(16)30249-2
Villani A, Tabori U, Schiffman J et al (2011) Biochemical and imaging surveillance in germline TP53 mutation carriers with Li-Fraumeni syndrome: a prospective observational study. The Lancet Oncol 12(6):559–567. doi: 10.1016/S1470-2045(11)70119-X
Ballinger ML, Mitchell G, Thomas DM (2015) Surveillance recommendations for patients with germline TP53 mutations. Curr Opin Oncol 27(4):332–337. doi: 10.1097/CCO.0000000000000200
McBride KA, Ballinger ML, Killick E et al (2014) Li-Fraumeni syndrome: cancer risk assessment and clinical management. Nat Rev Clin Oncol 11(5):260–271. doi:10.1038/nrclinonc.2014.41
Caron O et al. (2011) Evaluation of whole body mri for early detection of cancers in subjects with P53 mutation (Li-Fraumeni Syndrome) (LIFSCREEN). In ASCO Annual Meeting Proceedings 31(15):TPS1607
Masciari S, Van den Abbeele AD, Diller LR et al (2008) F18-fluorodeoxyglucose-positron emission tomography/computed tomography screening in Li-Fraumeni syndrome. JAMA 299(11):1315–1319 p[doi]
Nogueira STS, Lima ENP, Nóbrega AF et al (2015) (18)F-FDG PET-CT for surveillance of Brazilian patients with Li-Fraumeni Syndrome. Front Oncol 5:38. doi:10.3389/fonc.2015.00038
Brito JP., Morris JC, Montori VM (2013) Surveillance study investigating whole body magnetic resonance imaging and other diagnostic procedures in people at high risk of cancer
Heymann S, Delaloge S, Rahal A et al (2010) Radio-induced malignancies after breast cancer postoperative radiotherapy in patients with Li-Fraumeni syndrome. Radiat Oncol 5:104
Evans DGR, Birch JM, Ramsden RT, Sharif S, Baser ME (2006) Malignant transformation and new primary tumours after therapeutic radiation for benign disease: substantial risks in certain tumour prone syndromes. J Med Genet 43(4):289–294. doi: 10.1136/jmg.2005.036319
StataCorp (2015) Stata Statistical Software: Release 14. StataCorp LP, College Station
Bougeard G, Renaux-Petel M, Flaman JM et al (2015) Revisiting Li-Fraumeni Syndrome From TP53 Mutation Carriers. J Clin Oncol 33(21):2345–2352. doi: 10.1200/JCO.2014.59.5728
Evans DG, Kesavan N, Lim Y et al (2014) MRI breast screening in high-risk women: cancer detection and survival analysis. Breast Cancer Res Treat 145(3):663–672. doi: 10.1007/s10549-014-2931-9
Evans DG, Lennard F, Pointon LJ et al (2009) Eligibility for magnetic resonance imaging screening in the United Kingdom: effect of strict selection criteria and anonymous DNA testing on breast cancer incidence in the MARIBS Study. Cancer Epidemiol Biomarkers Prev 18(7):2123–2131. doi: 10.1158/1055-9965.EPI-09-0138
Hoang HLT, Ensor K, Rosen G, Leon Pachter H, Raccuia JS (2014) Prognostic factors and survival in patients treated surgically for recurrent metastatic uterine leiomyosarcoma. Intl J Surg Oncol 2014:8. doi: 10.1155/2014/919323
Schomas DA, Laack NNI, Rao RD, et al. (2009) Intracranial low-grade gliomas in adults: 30-year experience with long-term follow-up at Mayo Clinic. Neuro-Oncology 11(4): 437–445 doi: 10.1215/15228517-2008-102
Pepper C, Thomas A, Hoy T et al. (2003) Leukemic and non-leukemic lymphocytes from patients with Li Fraumeni syndrome demonstrate loss of p53 function, Bcl-2 family dysregulation and intrinsic resistance to conventional chemotherapeutic drugs but not flavopiridol. Cell cycle (Georgetown, Tex) 2(1): 53–8
Garritano S, Gemignani F, Palmero EI, Olivier M, Martel-Planche G, Le Calvez-Kelm F, Brugiéres L, Vargas FR, Brentani RR, Ashton-Prolla P, Landi S, Tavtigian SV, Hainaut P, Achatz MI (2010) Detailed haplotype analysis at the TP53 locus in p.R337H mutation carriers in the population of Southern Brazil: evidence for a founder effect. Hum Mutat 31(2):143–150. doi: 10.1002/humu.21151
Saifudeen Z, Dipp S, El-Dahr SS (2002) A role for p53 in terminal epithelial cell differentiation. J Clin Invest 109(8):1021–1030. doi: 10.1172/JCI13972
Saifudeen Z, Dipp S, Stefkova J, Yao X, Lookabaugh S, El-Dahr SS (2009) p53 regulates metanephric development. J Am Soc Nephrol 20(11):2328–2337. doi:10.1681/ASN.2008121224
Acknowledgements
We thank all the participants and families who took part in this research. This work was supported by The Annabel Evens Memorial Fund. The investigators at The Institute of Cancer Research and The Royal Marsden NHS Foundation Trust are supported by an NIHR research grant to the Biomedical Research Centre at The Institute of Cancer Research and The Royal Marsden NHS Foundation Trust. The SIGNIFY Study Steering Committee: Prof Anwar Padhani, Paul Strickland Scanner Centre, Mount Vernon Cancer Centre; Prof Leslie Walker, University of Hull; Dr Gillian Mitchell, Familial Cancer Centre, Peter MacCallum Cancer Centre and Sir Peter MacCallum Department of Oncology, University of Melbourne; Dr Gek Kwan-Lim, The Institute of Cancer Research and The Royal Marsden NHS Foundation Trust; Susan Eastbrook, patient representative; Dr Peter Simmonds, Cancer Sciences Academic Unit and University of Southampton Clinical Trials Unit, Faculty of Medicine, University of Southampton and University Hospital Southampton Foundation Trust; Dr Frank Saran, The Royal Marsden NHS Foundation Trust.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Sibel Saya and Emma Killick—Joint first authorship.
Richard W. Whitehouse, Dow-Mu Koh, S. Aslam Sohaib, D. Gareth Evans and Rosalind A. Eeles—Joint last authorship.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Saya, S., Killick, E., Thomas, S. et al. Baseline results from the UK SIGNIFY study: a whole-body MRI screening study in TP53 mutation carriers and matched controls. Familial Cancer 16, 433–440 (2017). https://doi.org/10.1007/s10689-017-9965-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10689-017-9965-1