Abstract
Purpose
Our aim was to report the characteristics and long-term surgical outcomes of three subgroups of horizontal strabismus in a single institution (divided by strabismus subtype) in a developing country and look into pre-operative factors predictive of surgical success.
Methods
Two hundred and forty-four complete charts of patients, divided into 152 esotropes (ET) and 92 exotropes (XT) who had undergone horizontal strabismus surgeries, were retrospectively reviewed. Charts of patients with muscle palsy, Duane syndrome and consecutive strabismus were excluded; 172 patients were included divided into partially accommodative ET, congenital ET and intermittent XT. Surgical success was defined as a post-operative angle deviation of 12 prism diopters or less.
Results
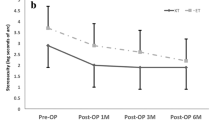
The mean follow-up period of all patients was 31.64 ± 23.12 months. The subgroups were divided into partially accommodative ET (60 patients), congenital ET (60 patients), and intermittent XT (52 patients). Esotropes (both partially accommodative and congenital) presented earlier (p < 0.001). Also, partially accommodative ET had a significantly higher spherical equivalent (SE) compared to congenital ET patients, who had a higher SE than intermittent XT (p < 0.001). Congenital ET patients had a significantly larger angle of deviation (for both far and near) than both partially accommodative ET and intermittent XT patients (p < 0.001). The overall success rate was 72.67% for the whole group with no significant differences among subgroups. Success rate of partially accommodative ET surgery was 78.33% compared to that of congenital ET at 66.67% and intermittent XT at 73.07%. Significant post-operative improvement in sensory fusion was observed mainly for patients with partially accommodative esotropia and intermittent exotropia.
Conclusion
Our results showed that esotropes (both partially accommodative and congenital) presented earlier, with a higher spherical equivalent in the partially accommodative ET subgroup, while the congenital ET subgroup had the largest angle of deviation for both distance and near. The overall surgical success rate for horizontal strabismus surgery was 72.67% with the 3 subgroups having similar success rates. A younger age at presentation and absence of amblyopia were positively correlated with surgical success in the partially accommodative esotropia group.
Similar content being viewed by others
References
Arora A, Williams B, Arora AK, McNamara R, Yates J, Fielder A (2005) Decreasing strabismus surgery. Br J Ophthalmol 89(4):409–412. https://doi.org/10.1136/bjo.2004.053678
Graham PA (1974) Epidemiology of strabismus. Br J Ophthalmol 58(3):224–231. https://doi.org/10.1136/bjo.58.3.224
Preslan MW, Novak A (1996) Baltimore vision screening project. Ophthalmology 103(1):105–109. https://doi.org/10.1016/s0161-6420(96)30753-7
Abrahamsson M, Magnusson G, Sjöstrand J (1999) Inheritance of strabismus and the gain of using heredity to determine populations at risk of developing strabismus. Acta Ophthalmol Scand 77(6):653–657. https://doi.org/10.1034/j.1600-0420.1999.770609.x
Kampanartsanyakorn S, Surachatkumtonekul T, Dulayajinda D, Jumroendararasmee M, Tongsae S (2005) The outcomes of horizontal strabismus surgery and influencing factors of the surgical success. J Med Assoc Thai 88(Suppl 9):S94–S99
Chia A, Dirani M, Chan Y-H et al (2010) Prevalence of amblyopia and strabismus in young Singaporean Chinese children. Invest Ophthalmol Vis Sci 51(7):3411–3417. https://doi.org/10.1167/iovs.09-4461
Burke JP, Leach CM, Davis H (1997) Psychosocial implications of strabismus surgery in adults. J Pediatr Ophthalmol Strabismus 34(3):159–164
Sun Y, Zhang T, Chen J (2018) Bilateral lateral rectus recession versus unilateral recession resection for basic intermittent exotropia: a meta-analysis. Graefes Arch Clin Exp Ophthalmol 256(3):451–458. https://doi.org/10.1007/s00417-018-3912-1
Dembinski RL, Collins ME, Kraus CL (2019) Outcomes following surgery for horizontal strabismus in children of lower socioeconomic backgrounds. Strabismus 27(2):47–53. https://doi.org/10.1080/09273972.2019.1626451
Chen YW, Lin SA, Lin PW, Huang HM (2019) The difference of surgical outcomes between manifest exotropia and esotropia. Int Ophthalmol 39(7):1427–1436. https://doi.org/10.1007/s10792-018-0956-5
Kumari N, Amitava AK, Ashraf M, Grover S, Khan A, Sonwani P (2017) Prognostic preoperative factors for successful outcome of surgery in horizontal strabismus. Oman J Ophthalmol 10(2):76–80. https://doi.org/10.4103/ojo.OJO_133_2016
Crouch ER Jr (1993) A comparison of the success rates of resident and attending strabismus surgery: discussion. J Pediatr Ophthalmol Strabismus 30(3):157–158
Bae GH, Bae SH, Choi DG (2019) Surgical outcomes of intermittent exotropia according to exotropia type based on distance/near differences. PLoS ONE 14(3):e0214478–e0214478. https://doi.org/10.1371/journal.pone.0214478
Birch EE, Stager DR Sr (2006) Long-term motor and sensory outcomes after early surgery for infantile esotropia. J Am Assoc Pediatric Ophthalmol Strabismus 10(5):409–413. https://doi.org/10.1016/j.jaapos.2006.06.010
Dohvoma VA, Ebana Mvogo SR, Ndongo JA, Mvilongo CT, Ebana Mvogo C (2020) Outcome of esotropia surgery in 2 tertiary hospitals in cameroon. Clin Ophthalmol 14:449–454. https://doi.org/10.2147/OPTH.S241861
Kushner BJ (2001) Fifteen-year outcome of surgery for the near angle in patients with accommodative esotropia and a high accommodative convergence to accommodation ratio. Arch Ophthalmol 119(8):1150–1153. https://doi.org/10.1001/archopht.119.8.1150
Maruo T, Kubota N, Sakaue T, Usui C (2001) Intermittent exotropia surgery in children: long term outcome regarding changes in binocular alignment. A study of 666 cases. Binocular Vis Strabismus Q 16(4):265–270
Ekdawi NS, Nusz KJ, Diehl NN, Mohney BG (2009) Postoperative outcomes in children with intermittent exotropia from a population-based cohort. J Am Assoc Pediatric Ophthalmol Strabismus 13(1):4–7. https://doi.org/10.1016/j.jaapos.2008.06.001
Berk AT, Koçak N, Ellidokuz H (2004) Treatment outcomes in refractive accommodative esotropia. J Am Assoc Pediatric Ophthalmol Strabismus 8(4):384–388. https://doi.org/10.1016/j.jaapos.2004.02.001
Archer SM, Sondhi N, Helveston EM (1989) Strabismus in infancy. Ophthalmology 96(1):133–137. https://doi.org/10.1016/S0161-6420(89)32932-0
Mohney BG, Erie JC, Hodge DO, Jacobsen SJ (1998) Congenital esotropia in olmsted county. Minnesota Ophthalmol 105(5):846–850. https://doi.org/10.1016/S0161-6420(98)95024-2
Wan MJ, Chiu H, Shah AS, Hunter DG (2018) Long-term surgical outcomes for large-angle infantile esotropia. Am J Ophthalmol 189:155–159. https://doi.org/10.1016/j.ajo.2017.11.006
Rutstein RP (2008) Update on accommodative esotropia. Optometry J Am Optometric Assoc 79(8):422–431. https://doi.org/10.1016/j.optm.2007.11.011
Hatt SR, Gnanaraj L (2013) Interventions for intermittent exotropia. Cochrane Database Syst Rev. https://doi.org/10.1002/14651858.CD003737.pub3
Wright KW (2003) Lens abnormalities. In: Wright KW, Spiegel PH (eds) Pediatric ophthalmology and strabismus. Springer, New York. https://doi.org/10.1007/978-0-387-21753-6_27
Abrahamsson M, Fabian G, Sjöstrand J (1992) Refraction changes in children developing convergent or divergent strabismus. Br J Ophthalmol 76(12):723. https://doi.org/10.1136/bjo.76.12.723
Ingram RM, Gill LE, Goldacre MJ (1994) Emmetropisation and accommodation in hypermetropic children before they show signs of squint—a preliminary analysis. Bull Soc Belge Ophtalmol 253:41–56
Raab EL (1984) Hypermetropia in accommodative esodeviation. J Pediatr Ophthalmol Strabismus 21(5):P64–P68
Sharma AK, Thapa M, Shrestha GB, Sitaula S, Shrestha GS (2014) Outcome of horizontal strabismus surgery and parents’ satisfaction. Nepal J Ophthalmol 6(2):162–169. https://doi.org/10.3126/nepjoph.v6i2.11704
Quigley C, Cairns M, McElnea E, Doyle F, McCance J, Mullaney P (2017) A retrospective evaluation of bilateral medial rectus recession for management of accommodative esotropia according to prism-adapted motor response preoperatively. J Am Assoc Pediatric Ophthalmol Strabismus 21(2):157-159.e1. https://doi.org/10.1016/j.jaapos.2016.10.007
Mohney BG (2001) Common forms of childhood esotropia. Ophthalmology 108(4):805–809. https://doi.org/10.1016/S0161-6420(00)00639-4
Sulayem LM, Bin-Khathlan AA (2018) Outcomes of esotropia surgery in Saudi Arabia: an audit from a single center. Saudi J Ophthalmol 32(4):280–285. https://doi.org/10.1016/j.sjopt.2018.07.006
Rosenbaum AL, Santiago AP (1999) Clinical strabismus management: principles and surgical techniques. David Hunter.
Al-Haddad C, Ismail K, Houry R, Al Sayyid S, El Moussawi Z (2020) Recurrence of intermittent exotropia after bilateral lateral rectus recession. Middle East Afr J Ophthalmol 27(2):123–127. https://doi.org/10.4103/meajo.MEAJO_188_18
Koklanis K, Georgievski Z (2009) Recurrence of intermittent exotropia: factors associated with surgical outcomes. Strabismus 17(1):37–40. https://doi.org/10.1080/09273970802678750
Kim HJ, Choi DG (2016) Clinical analysis of childhood intermittent exotropia with surgical success at postoperative 2 years. Acta Ophthalmol 94(2):e85–e89. https://doi.org/10.1111/aos.12849
Hatt SR, Mohney BG, Leske DA, Holmes JM (2008) Variability of stereoacuity in intermittent exotropia. Am J Ophthalmol 145(3):556-561.e1. https://doi.org/10.1016/j.ajo.2007.10.028
Stathacopoulos RA, Rosenbaum AL, Zanoni D et al (1993) Distance stereoacuity: assessing control in intermittent exotropia. Ophthalmology 100(4):495–500. https://doi.org/10.1016/S0161-6420(93)31616-7
Birch EE, Fawcett S, Stager DR (2000) Why does early surgical alignment improve stereoacuity outcomes in infantile esotropia? J Am Assoc Pediatric Ophthalmol Strabismus 4(1):10–14. https://doi.org/10.1016/S1091-8531(00)90005-3
Yildirim C, Mehmet Mutlu F, Chen Y, Altinsoy HI (1999) Assessment of central and peripheral fusion and near and distance stereoacuity in intermittent exotropic patients before and after strabismus surgery. Am J Ophthalmol 128(2):222–230. https://doi.org/10.1016/S0002-9394(99)00079-3
Adams WE, Leske DA, Hatt SR et al (2008) Improvement in distance stereoacuity following surgery for intermittent exotropia. J Am Assoc Pediatric Ophthalmol Strabismus 12(2):141–144. https://doi.org/10.1016/j.jaapos.2007.09.015
Birch EE, Wang J (2009) Stereoacuity outcomes after treatment of infantile and accommodative esotropia. Optometry Vis Sci 86(6):647–652. https://doi.org/10.1097/OPX.0b013e3181a6168d
Birch EE (2003) Marshall Parks lecture. Binocular sensory outcomes in accommodative ET. J Am Assoc Pediatric Ophthalmol Strabismus 7(6):369–373. https://doi.org/10.1016/j.jaapos.2003.08.003
Acknowledgements
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest related to this work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dakroub, M., El Hadi, D., El Moussawi, Z. et al. Characteristics and long-term surgical outcomes of horizontal strabismus. Int Ophthalmol 42, 1639–1649 (2022). https://doi.org/10.1007/s10792-021-02159-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10792-021-02159-4