Abstract
Objective
We assessed the predictive value added by Anti-Mullerian Hormone (AMH) to currently validated live birth (LB) prediction models.
Methods
Based on recent data from our center, we compared the external validity of the Templeton Model (TM) and its recent improvement (TMA) to select our model of reference. The added predictive value of AMH was assessed in testing the likelihood ratio significance and the Net Reclassification Index (NRI). The surrogate utility of AMH was tested by conducting an exploratory stepwise logistic regression.
Results
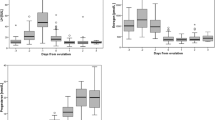
Based on 715 cycles, the original TM had poor performances (auROC C = 0.61 [0.58, 0.66], improving by fitting TM to our data (C = 0.71[0.66, 0.75]. TMA fitting proved better (C = 0.76; 95 %CI: 0.71, 0.80) and was selected as model of reference. Adding AMH to TMA or TM had no effect on discrimination (C = 0.76; 95 %CI: 0.72, 0.80), the likelihood ratio test was significant (p = 0.023), but the NRI was not (6.7 %; p = 0.055). A stepwise exploratory logistic regression identified the effects of age, previous IVF resulting in LB, time trend and AMH, leading to a prediction model reduced to four predictors (C = 0.75 [0.70, 0.81]).
Conclusion
The added predictive value of AMH is limited. A possible surrogate/simplifying effect of AMH was found in eliminating 9/13 predictors from the model of reference. We conclude that whereas AMH does not add significant predictive value to the existing model, it contributes to simplifying the equation to reliable, easy to collect, and available in all databases predictors: age, AMH, time trend and female previous fertility history.


Similar content being viewed by others

References
Templeton A, Morris JK, Parslow W. Factors that affect outcome of in-vitro fertilisation treatment. Lancet. 1996;348:1402–6.
Bancsi LF, Huijs AM, den Ouden CT, Broekmans FJ, Looman CW, Blankenstein MA, et al. Basal follicle-stimulating hormone levels are of limited value in predicting ongoing pregnancy rates after in vitro fertilization. Fertil Steril. 2000;73:552–7.
Commenges-Ducos M, Tricaud S, Papaxanthos-Roche A, Dallay D, Horovitz J, Commenges D. Modelling of the probability of success of the stages of in-vitro fertilization and embryo transfer: stimulation, fertilization and implantation. Hum Reprod. 1998;13:78–83.
Ferlitsch K, Sator MO, Gruber DM, Rucklinger E, Gruber CJ, Huber JC. Body mass index, follicle-stimulating hormone and their predictive value in in vitro fertilization. J Assist Reprod Genet. 2004;21:431–6.
Hunault CC, Eijkemans MJ, Pieters MH, te Velde ER, Habbema JD, Fauser BC, et al. A prediction model for selecting patients undergoing in vitro fertilization for elective single embryo transfer. Fertil Steril. 2002;77:725–32.
Lintsen AM, Eijkemans MJ, Hunault CC, Bouwmans CA, Hakkaart L, Habbema JD, et al. Predicting ongoing pregnancy chances after IVF and ICSI: a national prospective study. Hum Reprod. 2007;22:2455–62.
Minaretzis D, Harris D, Alper MM, Mortola JF, Berger MJ, Power D. Multivariate analysis of factors predictive of successful live births in in vitro fertilization (IVF) suggests strategies to improve IVF outcome. J Assist Reprod Genet. 1998;15:365–71.
Nelson SM, Lawlor DA. Predicting live birth, preterm delivery, and low birth weight in infants born from in vitro fertilisation: a prospective study of 144,018 treatment cycles. PLoS Med. 2011;8:e1000386.
Ottosen LD, Kesmodel U, Hindkjaer J, Ingerslev HJ. Pregnancy prediction models and eSET criteria for IVF patients–do we need more information? J Assist Reprod Genet. 2007;24:29–36.
Smeenk JM, Stolwijk AM, Kremer JA, Braat DD. External validation of the templeton model for predicting success after IVF. Hum Reprod. 2000;15:1065–8.
Stolwijk AM, Wetzels AM, Braat DD. Cumulative probability of achieving an ongoing pregnancy after in-vitro fertilization and intracytoplasmic sperm injection according to a woman’s age, subfertility diagnosis and primary or secondary subfertility. Hum Reprod. 2000;15:203–9.
Leushuis E, van der Steeg JW, Steures P, Bossuyt PM, Eijkemans MJ, van der Veen F, et al. Prediction models in reproductive medicine: a critical appraisal. Hum Reprod Update. 2009;15:537–52.
te Velde ER, Nieboer D, Lintsen AM, Braat DD, Eijkemans MJ, Habbema JD, et al. Comparison of two models predicting IVF success; the effect of time trends on model performance. Hum Reprod. 2014;29:57–64.
Arvis P, Lehert P, Guivarc’h-Leveque A. Simple adaptations to the Templeton model for IVF outcome prediction make it current and clinically useful. Hum Reprod. 2012;27:2971–8.
La Marca A, Argento C, Sighinolfi G, Grisendi V, Carbone M, D’Ippolito G, et al. Possibilities and limits of ovarian reserve testing in ART. Curr Pharm Biotechnol. 2012;13:398–408.
Kallio S, Aittomaki K, Piltonen T, Veijola R, Liakka A, Vaskivuo TE, et al. Anti-Mullerian hormone as a predictor of follicular reserve in ovarian insufficiency: special emphasis on FSH-resistant ovaries. Hum Reprod. 2012;27:854–60.
Visser JA, Schipper I, Laven JS, Themmen AP. Anti-Mullerian hormone: an ovarian reserve marker in primary ovarian insufficiency. Nat Rev Endocrinol. 2012;8:331–41.
Buyuk E, Seifer DB, Younger J, Grazi RV, Lieman H. Random anti-Mullerian hormone (AMH) is a predictor of ovarian response in women with elevated baseline early follicular follicle-stimulating hormone levels. Fertil Steril. 2011;95:2369–72.
Broer SL, Dolleman M, Opmeer BC, Fauser BC, Mol BW, Broekmans FJ. AMH and AFC as predictors of excessive response in controlled ovarian hyperstimulation: a meta-analysis. Hum Reprod Update. 2011;17:46–54.
Seifer DB, MacLaughlin DT, Christian BP, Feng B, Shelden RM. Early follicular serum mullerian-inhibiting substance levels are associated with ovarian response during assisted reproductive technology cycles. Fertil Steril. 2002;77:468–71.
Freeman EW, Sammel MD, Lin H, Gracia CR. Anti-mullerian hormone as a predictor of time to menopause in late reproductive age women. J Clin Endocrinol Metab. 2012;97:1673–80.
Rustamov O, Smith A, Roberts SA, Yates AP, Fitzgerald C, Krishnan M, et al. Anti Mullerian Hormone: poor assay reproductibility in a large cohort of subjects suggests sample instability. Hum Reprod. 2012;27:3085–91.
Lee TH, Liu CH, Huang CC, Hsieh KC, Lin PM, Lee MS. Impact of female age and male infertility on ovarian reserve markers to predict outcome of assisted reproduction technology cycles. Reprod Biol Endocrinology : RB&E. 2009;7:100.
Khader A, Lloyd SM, McConnachie A, Fleming R, Grisendi V, La Marca A, et al. External validation of anti-Mullerian hormone based prediction of live birth in assisted conception. J Ovarian Res. 2013;6:3.
Brodin T, Hadziosmanovic N, Berglund L, Olovsson M, Holte J. AMH Is Related to ART Outcome and Oocyte Quality. J Clin Endocrinol Metab. 2013;98:1107–14.
Swets JA. Measuring the accuracy of diagnostic systems. Science. 1988;240:1285–93.
Hosmer DWLS. Applied Logistic Regression. New York: Wiley and Sons; 2000.
Steyerberg EW, Harrell Jr FE, Borsboom GJ, Eijkemans MJ, Vergouwe Y, Habbema JD. Internal validation of predictive models: efficiency of some procedures for logistic regression analysis. J Clin Epidemiol. 2001;54:774–81.
Pencina MJ, D’Agostino Sr RB, D’Agostino Jr RB, Vasan RS. Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med. 2008;27:157–72. discussion 207–12.
Lintsen AM, Braat DD, Habbema JD, Kremer JA, Eijkemans MJ. Can differences in IVF success rates between centres be explained by patient characteristics and sample size? Hum Reprod. 2010;25:110–7.
van Loendersloot LL, van Wely M, Repping S, van der Veen F, Bossuyt PM. Templeton prediction model underestimates IVF success in an external validation. Reprod Biomed Online. 2011;22:597–602.
Coppus SF, van der Veen F, Opmeer BC, Mol BW, Bossuyt PM. Evaluating prediction models in reproductive medicine. Hum Reprod. 2009;24:1774–8.
Young DS. Tolerance: an R package for estimating tolerance intervals. J Stat Softw. 2010;36:1–39.
Conflict of interest
None
Author information
Authors and Affiliations
Corresponding author
Additional information
Capsule The added predictive value of AMH to existing predictive model for live birth is limited; however AMH may contribute to simplify the model.
Rights and permissions
About this article
Cite this article
Rongieres, C., Colella, C. & Lehert, P. To what extent does anti-mullerian hormone contribute to a better prediction of live birth after IVF?. J Assist Reprod Genet 32, 37–43 (2015). https://doi.org/10.1007/s10815-014-0348-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-014-0348-3