Abstract
Purpose
High survival rates and clinical outcomes similar to those from fresh oocytes and blastocysts have been observed with open oocyte vitrification systems. It has been suggested that the extremely fast cooling rates that are only achieved with open systems are necessary for human oocyte and blastocyst vitrification. However, there is a potential risk of introducing contamination with open systems. The aim of this study was to assess whether similar survival and subsequent implantation rates could be achieved using a closed vitrification system for human oocytes and blastocysts.
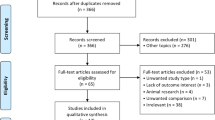
Methods
Initially, donated immature oocytes that were matured in vitro were vitrified using the cryoprotectants ethylene glycol (EG) + dimethyl sulphoxide (DMSO) + sucrose and either a closed system (Rapid-i®) or an open system (Cryolock). The closed system was subsequently introduced clinically for mature oocyte cryopreservation cases and blastocyst vitrification.
Results
Using in vitro matured oocytes, a similar survival was achieved with the open system of 92.4 % (73/79) and with the closed system of 89.7 % (35/39). For clinical oocyte closed vitrification, high survival rate of 90.5 % (374/413) and an implantation rate of 32.7 % (18/55) from the transfer of day 2 embryos was achieved, which is similar to fresh day 2 embryo transfers. Blastocysts have also been successfully cryopreserved using the Rapid-i closed vitrification system with 94 % of blastocysts having an estimated ≥75 % of cells intact and a similar implantation rate (31.5 %) to fresh single blastocyst transfers.
Conclusion
Closed vitrification can achieve high survival and similar implantation rates to fresh for both oocytes and blastocysts.
Similar content being viewed by others
References
Li Z, Wang YA, Ledger W, Edgar DH, Sullivan EA. Clinical outcomes following cryopreservation of blastocysts by vitrification or slow freezing: a population-based cohort study. Hum Reprod. 2014;29(12):2794–801.
Edgar DH, Gook DA. A critical appraisal of cryopreservation (slow cooling versus vitrification) of human oocytes and embryos. Hum Reprod Update. 2012;18:536–54.
Cobo A, de los Santos MJ, Castello D, Gamiz P, Campos P, Remohi J. Outcomes of vitrified early cleavage-stage and blastocyst-stage embryos in a cryopreservation program: evaluation of 3,150 warming cycles. Fertil Steril. 2012;98(5):1138–46. e1.
Cobo A, Meseguer M, Remohi J, Pellicer A. Use of cryo-banked oocytes in an ovum donation programme: a prospective, randomized, controlled, clinical trial. Hum Reprod. 2010;25(9):2239–46.
Cobo A, Remohi J, Chang CC, Nagy ZP. Oocyte cryopreservation for donor egg banking. Reprod Biomed Online. 2011;23(3):341–6.
Liebermann J. Vitrification of human blastocysts: an update. Reprod Biomed Online. 2009;19 Suppl 4:4328.
Devine K, Connell MT, Richter KS, Ramirez CI, Levens ED, DeCherney AH, et al. Single vitrified blastocyst transfer maximizes liveborn children per embryo while minimizing preterm birth. Fertil Steril. 2015;103(6):1454–60. e1.
Bielanski A, Nadin-Davis S, Sapp T, Lutze-Wallace C. Viral contamination of embryos cryopreserved in liquid nitrogen. Cryobiology. 2000;40:110–6.
Tedder RS, Zuckerman MA, Goldstone AH, Hawkins AE, Fielding A, Briggs EM, et al. Hepatitis B transmission from contaminated cryopreservation tank. Lancet. 1995;346(8968):137–40.
Bielanski A, Vajta G. Risk of contamination of germplasm during cryopreservation and cryobanking in IVF units. Hum Reprod. 2009;24:2457–67.
Cobo A, Romero JL, Perez S, de Los Santos MJ, Meseguer M, Remohi J. Storage of human oocytes in the vapor phase of nitrogen. Fertil Steril. 2010;94(5):1903–7.
Parmegiani L, Accorsi A, Cognigni GE, Bernardi S, Troilo E, Filicori M. Sterilization of liquid nitrogen with ultraviolet irradiation for safe vitrification of human oocytes or embryos. Fertil Steril. 2010;94(4):1525–8.
Parmegiani L, Accorsi A, Bernardi S, Arnone A, Cognigni GE, Filicori M. A reliable procedure for decontamination before thawing of human specimens cryostored in liquid nitrogen: three washes with sterile liquid nitrogen (SLN2). Fertil Steril. 2012;98(4):870–5.
Vajta G, Rienzi L, Ubaldi FM. Open versus closed systems for vitrification of human oocytes and embryos. Reprod Biomed Online. 2015;30(4):325–33.
Seki S, Mazur P. Effect of warming rate on the survival of vitrified mouse oocytes and on the recrystallization of intracellular ice. Biol Reprod. 2008;79(4):727–37.
Seki S, Mazur P. The dominance of warming rate over cooling rate in the survival of mouse oocytes subjected to a vitrification procedure. Cryobiology. 2009;59(1):75–82.
Vanderzwalmen P, Zech N, Prapas Y, Panagiotidis Y, Papatheodorou A, Lejeune B, et al. Closed carrier device: a reality to vitrify oocytes and embryos in aseptic conditions. Gynecol Obstet Fertil. 2010;38(9):541–6.
Papatheodorou A, Vanderzwalmen P, Panagiotidis Y, Prapas N, Zikopoulos K, Georgiou I, et al. Open versus closed oocyte vitrification system: a prospective randomized sibling-oocyte study. Reprod Biomed Online. 2013;26(6):595–602.
Chen Y, Zheng X, Yan J, Qiao J, Liu P. Neonatal outcomes after the transfer of vitrified blastocysts: closed versus open vitrification system. Reprod Biol Endocrinol. 2013;11:107.
Iwahata H, Hashimoto S, Inoue M, Inoue T, Ito K, Nakaoka Y, et al. Neonatal outcomes after the implantation of human embryos vitrified using a closed-system device. J Assist Reprod Genet. 2015;32(4):521–6.
Panagiotidis Y, Vanderzwalmen P, Prapas Y, Kasapi E, Goudakou M, Papatheodorou A, et al. Open versus closed vitrification of blastocysts from an oocyte-donation programme: a prospective randomized study. Reprod Biomed Online. 2013;26(5):470–6.
Desai NN, Goldberg JM, Austin C, Falcone T. The new Rapid-i carrier is an effective system for human embryo vitrification at both the blastocyst and cleavage stage. Reprod Biol Endocrinol. 2013;11:41.
Hashimoto S, Amo A, Hama S, Ohsumi K, Nakaoka Y, Morimoto Y. A closed system supports the developmental competence of human embryos after vitrification : closed vitrification of human embryos. J Assist Reprod Genet. 2013;30(3):371–6.
Paffoni A, Guarneri C, Ferrari S, Restelli L, Nicolosi AE, Scarduelli C, et al. Effects of two vitrification protocols on the developmental potential of human mature oocytes. Reprod Biomed Online. 2011;22:292–8.
Bourne H, Richings N, Harari O, Watkins W, Speirs AL, Johnston WIH, et al. The use of intracytoplasmic sperm injection for the treatment of severe and extreme male infertility. Reprod Fertil Dev. 1995;7:237–45.
Lawler C, Baker HW, Edgar DH. Relationships between timing of syngamy, female age and implantation potential in human in vitro-fertilised oocytes. Reprod Fertil Dev. 2007;19(3):482–7.
Edgar DH, Bourne H, Speirs AL, McBain JC. A quantitative analysis of the impact of cryopreservation on the implantation potential of human early cleavage stage embryos. Hum Reprod. 2000;15:175–9.
Edgar DH, Karani J, Gook DA. Increasing dehydration of human cleavage-stage embryos prior to slow cooling significantly increases cryosurvival. Reprod Biomed Online. 2009;19(4):521–5.
Nagy ZP, Chang CC, Shapiro DB, Bernal DP, Elsner CW, Mitchell-Leef D, et al. Clinical evaluation of the efficiency of an oocyte donation program using egg cryo-banking. Fertil Steril. 2009;92(2):520–6.
Ubaldi F, Anniballo R, Romano S, Baroni E, Albricci L, Colamaria S, et al. Cumulative ongoing pregnancy rate achieved with oocyte vitrification and cleavage stage transfer without embryo selection in a standard infertility program. Hum Reprod. 2010;25(5):1199–205.
Garcia JI, Noriega-Portella L, Noriega-Hoces L. Efficacy of oocyte vitrification combined with blastocyst stage transfer in an egg donation program. Hum Reprod. 2011;26:782–90.
Trokoudes KM, Pavlides C, Zhang X. Comparison outcome of fresh and vitrified donor oocytes in an egg-sharing donation program. Fertil Steril. 2011;95(6):1996–2000.
Rienzi L, Cobo A, Paffoni A, Scarduelli C, Capalbo A, Vajta G, et al. Consistent and predictable delivery rates after oocyte vitrification: an observational longitudinal cohort multicentric study. Hum Reprod. 2012;27:1606–12.
Sole M, Santalo J, Boada M, Clua E, Rodriguez I, Martinez F, et al. How does vitrification affect oocyte viability in oocyte donation cycles? A prospective study to compare outcomes achieved with fresh versus vitrified sibling oocytes. Hum Reprod. 2013;28(8):2087–92.
Stoop D, De Munck N, Jansen E, Platteau P, Van den Abbeel E, Verheyen G, et al. Clinical validation of a closed vitrification system in an oocyte-donation programme. Reprod Biomed Online. 2012;24:180–5.
De Munck N, Verheyen G, Van Landuyt L, Stoop D, Van de Velde H. Survival and post-warming in vitro competence of human oocytes after high security closed system vitrification. J Assist Reprod Genet. 2013;30(3):361–9.
Seki S, Mazur P. Ultra-rapid warming yields high survival of mouse oocytes cooled to −196 degrees C in dilutions of a standard vitrification solution. PLoS ONE. 2012;7(4):e36058.
Gook DA, Edgar DH. Implantation rates of embryos generated from slow cooled human oocytes from young women are comparable to those of fresh and frozen embryos from the same age group. J Assist Reprod Genet. 2011;28(12):1171–6.
Author information
Authors and Affiliations
Corresponding author
Additional information
Capsule Closed vitrification can achieve high survival and similar implantation rates to fresh for both human oocytes and blastocysts.
Rights and permissions
About this article
Cite this article
Gook, D.A., Choo, B., Bourne, H. et al. Closed vitrification of human oocytes and blastocysts: outcomes from a series of clinical cases. J Assist Reprod Genet 33, 1247–1252 (2016). https://doi.org/10.1007/s10815-016-0748-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10815-016-0748-7