Abstract
Aim Studies show that about 60 min of moderate physical activity (PA) per day compensate for sitting all day at work. However, the workplace offers an ideal setting for health-promoting interventions such as PA coaching as a person-centered intervention aimed at achieving lasting health behavior changes. Given a good evidence base of health coaching studies in general, this systematic review aims to provide an overview of workplace PA coaching interventions. Methods This review was conducted according to PRISMA guidelines. Studies published up to July 2021 were considered based on the following inclusion criteria: (1) longitudinal intervention studies, (2) analysis of PA at work, (3) sedentary employees, (4) PA coaching in the workplace as intervention, (5) increasing workplace PA. Results Of 4323 studies found, 14 studies with 17 interventions met inclusion criteria. All 17 interventions indicated an increase in at least one PA outcome. Twelve interventions indicated significant improvements in at least one workplace or total PA outcome. There is a high variation within the different coaching parameters, such as behavior change techniques and communication channels. The study quality showed a moderate to high risk of bias. Conclusions The majority of interventions provided evidence for the effectiveness of workplace PA coaching. Nevertheless, the results are inconclusive with regard to the variety of coaching parameters and thus no general statement can be made about the effectiveness of individual parameters. However, this variety of parameters also leads to a high degree of individualization of workplace PA coaching interventions to increase PA for different groups of employees and different types of workplaces.
Similar content being viewed by others
Introduction
More than half of the adult population are physically active for less than two and a half hours per week and hence do not meet the core aspect of the WHO recommendations for physical activity (PA; [1,2,3]). Despite well-publicized national health campaigns and a large choice of recreational activities, this statistic is surprising. The extensive positive effects are multifaceted and refer to both physical as well as psychological improvements at any age [4]. Physical improvements relate to, for example, reduced risks for weight gain and overweight/obesity, type 2 diabetes, cardiovascular diseases, stroke, age-related illnesses such as dementia and Alzheimer’s disease, and several types of cancer [5,6,7,8,9]. Psychological improvements include the reduction of symptoms of depression and anxiety, improvement of mood, and stress management [10, 11].
One method to increase PA behavior is physical activity coaching (PA coaching). Coaching to change a health behavior, in this case PA, is a collaborative patient- or person-centered approach to empower individuals to take responsibility for their PA behavior and to facilitate their achievement of PA-related goals in order to change their PA behavior permanently [12,13,14]. PA coaching can be installed in many different settings, such as schools, health care organizations, community centers, recreational facilities, and workplaces [15, 16].
The workplace, in particular, is an ideal setting for the implementation of PA coaching. It can overcome commonly cited barriers, such as lack of time, and provides access to a broad and diverse section of society [17,18,19]. Especially, people with particular health risks are easier to reach in the workplace than in the leisure time, where there are often major barriers to accessing health programs. Other advantages of the workplace as a health-promoting setting include the "convenient place and time," as well as the possibility of "paid time off" while being physically active; [20]). In addition, company leadership has a responsibility to ensure and promote the health of their employees [21]; conversely, they also benefit greatly from the long-term good health of their employees in terms of lower health care costs and added working time [22,23,24]. However, in addition to these benefits, the workplace also presents some issues that need to be addressed, such as relatively little time available for health programs and organizational challenges.
PA coaching interventions are characterized by different parameters, such as the time scope or organization of coaching. Time scope includes, for example, the duration of the intervention (short-term vs. long-term; [13] and the frequency and duration of the coaching interactions (speed coaching vs. longer conversation; [13]). Organization of coaching includes, for example, the communication channel (e.g., in person, telephone, web [25,26,27] and additional voluntary interventions including environmental modifications (e.g., walking tracks outside a company; [28]). Further parameters comprise the underlying theory (e.g., self-determination theory, SDT, [29]; transtheoretical model of change, TTM, [30]; social cognitive theory, SCT, [31]) and the question of which and how many behavior change techniques (BCTs) are applied [32]. The role of the coach in PA coaching is active listening, supporting, motivating [25], and using motivational strategies to change health behaviors [33], such as goal setting, social support, and barrier management [13, 30].
Despite the wide variety of compositions of PA coaching interventions, numerous studies showed positive effects on the PA behavior for patients with different chronic conditions, for inactive people, and in different settings [34,35,36,37,38]. In addition to these primary studies, recent reviews also summarized the effects of PA coaching, showing positive effects on the PA behavior in different target groups, for example, inactive adults [39], patients with chronic diseases [40], and the elderly [41, 42]. So far, however, there are only reviews that summarize general workplace physical activity promotion interventions (e.g., [17, 43]). Likewise, some workplace PA coaching interventions showed positive effects according to Dugdill et al. [17]. Although there is evidence for PA coaching interventions in a variety of settings, and likewise in the workplace, a review of studies summarizing solely PA coaching in the workplace is yet lacking.
Considering the increasing importance of PA promotion, the known positive effects of PA on health, as well as the positive effects of coaching, it is important to understand how workplace PA can be promoted in workplace coaching programs. Therefore, the purpose of this review is to summarize existing coaching interventions promoting workplace PA in order to provide an up-to-date overview of intervention studies. Specific objectives include (1) describing the characteristics of these interventions (e.g., time scope of coaching, organization of coaching, theoretical foundation, applied BCTs) and (2) determining whether these interventions have a positive impact on PA.
Methods
This systematic review was conducted in line with PRISMA guidelines [44]. The protocol of the study is registered with the PROSPERO database and can be accessed under reference number CRD42021256548.
Inclusion Criteria
To be included in this review, studies had to be longitudinal intervention studies. For this review, the intervention, PA coaching in the workplace, was defined as personalized, person-centered, interactive PA coaching (within the institution/company) that is either web-based, telephone-based, mobile-based, or in person. When it comes to e-coaches (web-based/mobile-based), this review included interventions that considered e-coaching systems as a computerized part of a system that uses an artificial entity to observe, learn from, and support user behavior in a proactive collaboration applying planning and goal-related techniques [45]. There had to be at least one interaction between coach and coachee (coached employee) and it could be either individual or group coaching. Interventions had to aim at increasing health-enhancing PA in the workplace (plus optional leisure time PA, subjectively and/or objectively assessed). Health-enhancing PA was defined as “any form of physical activity that benefits health and functional capacity without undue harm and risk” [46]. Furthermore, interventions had to be addressed toward sedentary employees. Sedentary work was defined as "involving lifting no more than 10 pounds at a time and occasionally lifting and carrying articles like, docket files, ledgers, and small tools" (The United States Social Security Administration 2012). The reason for including sedentary employees is that prolonged sitting at work in particular can pose a health risk [47]. Studies that did not meet the inclusion criteria were excluded from this review.
There were no restrictions on the basis of sample size, participant characteristics (e.g., age, gender), type of PA coaching intervention, study length, duration of follow-up, or publication date. Randomized, controlled, and quasi-experimental studies, as well as pilot studies were included, as a pure randomized controlled trial (RCT) design is not always possible in a workplace setting. Similarly, multicomponent health promotion interventions with the main aim of improving general health were included if they provided an outcome measure that focused specifically on employees’ PA.
Literature Search
The literature search was conducted using the following electronic databases: PsycINFO, PsycArticles, PSYNDEX, Web of Science, SocIndex, and MEDLINE. A broad search strategy was elaborated using a combination of specified search terms (Table 1). Peer-reviewed studies published in English and German up to July 2021 were retrieved. Two review authors independently reviewed the titles and abstracts of all potentially relevant articles for eligibility. Either articles were confidently included, confidently excluded, or this decision was made after full-text screening when still uncertain. Any disagreements between the two were resolved through discussions involving a third person.
Data Extraction
Two review authors extracted the data independently and merged them afterwards. Likewise, when discrepancies were identified during this process, they were resolved in a conversation with a third person. The extracted data included the author(s), year of data collection, country/region of data collection, type of study, sample size, age, gender, response rate, professional sector, other behaviors potentially addressed in coaching, duration of intervention, frequency and duration of coaching interactions, group/individual intervention, communication channel, voluntary interventions in addition to coaching, underlying theory/model, number and name of applied BCTs, PA outcomes (workplace, leisure time, transport), and measurements used to assess the PA outcome(s).Footnote 1 In addition to these categories reported in the protocol, the goals of the interventions as well as the numbers and types of the control group/further intervention groups were also reported. Furthermore, the material provided during coaching, the PA outcomes, and the type of coach (person/e-coach) were added. Due to lack of data, the type of sampling as written in the protocol was not considered for this review.
Quality Assessment
The methodological quality of each study was assessed independently by two review authors using the revised and validated Cochrane risk of bias tools for randomized trials (RoB 2, [48]) and for non-randomized trials (ROBINS-I, [49]). When discrepancies were identified during this process, they were resolved in a conversation with a third person. Additionally, this review used the taxonomy of BCTs developed by Michie et al. [32] to derive and better compare the specific BCTs used in the coaching interventions promoting PA. Due to assumed heterogeneous study designs, no overall meta-analytical effect sizes were analyzed in this paper.
Results
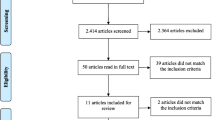
The initial computerized search found 4323 publications (Fig. 1). Computerized duplication removal of several factors (using doi, filtering by abstract, title, and authors, and sorting from a to z) resulted in 2740 publications. The authors of two publications of which only the abstract was available online were contacted but without success. After title and abstract screening of the 2740 studies by two review authors, 2691 studies were further excluded. The remaining 49 studies were reviewed for full-text screening. After full-text screening, 35 studies were excluded. Reasons for exclusion included, for example, lack of individualization in PA coaching (n = 8), no PA components in coaching (n = 9) or no longitudinal intervention study (n = 1). Ultimately, 14 studies were selected for this review (detailed information in Table 2 and Table 3).
Sample Characteristics
The total sample size amounted to N = 1394 and ranged from 13 to 246 (M = 82) between the 14 studiesFootnote 2 examined. Seven of the 14 studies had a majority of female participants (> 70%) (Table 2; interventions 1, 3, 7, 12–17), out of those, three studies were conducted exclusively with female subjects (Table 2; interventions 12–14, 16, 17). There was only one study with exclusively male participants (Table 2, intervention 5). Two studies provided no indication of gender (Table 2; interventions 6, 8, 9). The participants’ median age ranged from 38.3 to 58.9 years. Overall, in 11 studies the participants’ median age was between 40 and 50 years (Table 2; interventions 1, 2, 3, 5, 7, 10–17). Employees were recruited from health care organizations (Table 2; interventions 1, 3, 10, 13–17), universities (Table 2; interventions 2, 8, 9, 12), the production sector (Table 2; interventions 6, 7), the transportation sector (Table 2; interventions 4, 5), as well as “other services” [municipal services (Table 2, intervention 11)]. Response rates at the last measurement point ranged between 42 and 100% (M = 77%). Eleven studies had a response rate > 70% (Table 2; interventions 1, 2, 5–13, 16, 17).
Study Design
Nine of the 14 studies were randomized controlled trials (RCTs) (Table 2; interventions 3, 7–17). The remaining studies were non-randomized trials (Table 2; interventions 1, 2, 4–6).
Among the RCTs, different control group designs were used [passive control groups (Table 2; interventions 7, 10)], additional intervention group(s) (Table 2; interventions 7, 8, 9, 13–17), active control group (Table 2; interventions 3, 11, 12). The non-RCTs also included different groups in the studies (no control group (Table 2; interventions 2, 4, 5), an active control group (Table 2, intervention 6), a passive control group (Table 2, intervention 1)].
Regarding their follow-up measurement, nine studies measured effects before and after the intervention (Table 2; interventions 2–4, 6–12) with five studies applying a follow-up measurement [after eight weeks (Table 2, intervention 5), after four months (Table 2, intervention 15), after 6 months (Table 2; interventions 1, 13, 14, 16, 17)].
Goals and Behaviors Addressed in Coaching
In terms of goals, increasing PA is the only objective reported in five of the 17 interventions2 (Table 2; interventions 1, 4, 6, 10, 12). Nine interventions reported the evaluation of other variables and additional goals, such as the reduction of sedentary (Table 2; interventions 2, 3, 7, 16, 17) and dietary behavior (Table 2, intervention 5) or the examination of mental health (Table 2; interventions 7–9, 11).
In terms of behaviors addressed in coaching, 13 interventions solely targeted PA behavior (Table 2; interventions 1, 4, 6–10, 12, 13–17). The other four addressed additional behaviors, such as sedentary and dietary, stress, and smoking behavior in their coaching (Table 2; interventions 2, 3, 5, 11).
Time Scope of Coaching
The scope of coaching, including the duration of the intervention, the total number of interactions, the duration and frequency of the interactions, was very heterogeneous. The duration of PA coaching ranged from two to 36 weeks with the most common frequency being 12 weeks (Table 2; interventions 1, 6, 8, 9, 13, 14, 16, 17). The total number of interactions ranged from two to 168 interactions. Eleven interventions had two to 12 interactions (Table 2; interventions 1, 4, 5, 7–9, 11, 12–15), and six interventions had more than 84 to 168 interactions (Table 2; interventions 2, 3, 6, 10, 16, 17). In three of the 17 interventions, wide ranges of interactions between e-coach and coachee were reported, because in these cases the coachees themselves determined how often they “approached” their e-coach (Table 2; interventions 10, 16, 17). To ensure comparability, the total highest number of interactions was therefore reported in this review. The frequency of coaching interactions (meaning how often interactions between coach and coachee occurred during the duration of the intervention) was regular (daily, biweekly, triweekly) in eight of the included interventions (Table 2; interventions 1, 2, 3, 6, 10, 15 at the beginning, 16, 17). In seven interventions, interactions were more frequent in the initial phase and then subsided with the intervention period (Table 2; interventions 4, 5, 8, 9, 12, 14, 15 at the end). Three interventions did not provide any information on the frequency of coaching contacts (Table 2; interventions 7, 11, 13).
Organization of Coaching
The organization of coaching, which involves the setting, communication channel, additional coaching materials, or additional voluntary interventions to increase workplace PA, also varied widely across all interventions. Thirteen of the 17 interventions included were individual interventions (Table 2; interventions 1, 2, 3, 6, 8–13, 15–17), one was a group intervention (Table 2, intervention 14), and three were combinations (Table 2; interventions 4, 5, 7). The choice of communication channel varied widely across interventions ranging from exclusively face-to-face communication (6 times) (Table 2; interventions 4, 7, 8, 11, 13, 14), mobile app (2 times) (Table 2; interventions 2, 3), messaging (4 times) (Table 2; interventions 10, 15, 16, 17), or a combination thereof (5 times) (Table 2; interventions 1, 5, 6, 9, 12). Nine interventions used additional materials for coaching, such as brochures/leaflets/workbooks (Table 2; interventions 1, 4, 6, 8, 9, 11–14), a website with written information (Table 2; interventions 10, 15), or an activity/step diary (Table 2; interventions 4, 13, 14). Additional voluntary interventions to increase workplace PA next to PA coaching were also integrated into some interventions. Examples were walking meetings (5 times) (Table 2; interventions 7–9, 16, 17), exercise sessions/PA programs (1 time) (Table 2, intervention 7), stair climbing (Table 2; interventions 16, 17), provision of a company bike and sit-stand desks (1 time) (Table 2, intervention 7), or a workstation treadmill and a video game system (2 times) (Table 2; interventions 16, 17).
Figure 2 presents an overview of the communication channels used in the interventions, the duration of the interventions, and the number of interactions
Theory
Of the 17 interventions, five were based on a psychological theory (TTM: (Table 2; interventions 11, 12, 15), SCT: (Table 2, intervention 4), SDT: (Table 2, intervention 1).
Behavior Change Techniques
Seventeen BCTs were identified throughout all interventions. The number of identified BCTs per intervention ranged from one to nine techniques. The six most frequently used techniques were goal setting (14 times), self-monitoring (of behavior and outcomes of behavior) (11 times), feedback (on behavior and outcomes of behavior) (9 times), information about health consequences (8 times), social support (7 times), and problem solving (7 times). The most frequently used combinations of BCTs were goal setting and self-monitoring (11 times), goal setting and information about health consequences (8 times), goal setting and feedback, goal setting and social support, and self-monitoring and feedback (6 times each) (Online Resource Table 4).
Coach
The interventions used different types of coaches. They included coaching by personal contact with scientific personnel (6 times) (Table 2; interventions 1, 5, 8, 9, 16, 17) or health care personnel (6 times) (Table 2; interventions 4, 7, 11–14). Other four interventions relied on an e-coaching system (Table 2; interventions 2, 3, 6, 10). Two did not mention their type of coach [Table 2; interventions 6 (no information about face-to-face coach), 15)].
Outcomes
PA outcomes as well as their measurements varied widely across all studies. Eight studies measured their PA outcomes (e.g., total energy expenditure, time spent walking or being active, numbers of flights of stairs and daily steps) objectively using different versions of accelerometers (Table 2; interventions 2, 3, 5, 7, 10, 16, 17) and pedometers (Table 2; interventions 4, 13, 14). Four studies used subjective measurement methods (questionnaires) (Table 2; interventions 8, 9, 11, 12, 15). The rest used a combination of both (Table 2; interventions 1, 6).
Effects of Interventions on PA Outcomes
All 17 interventions indicated an increase in at least one PA outcome (Table 3). In terms of workplace PA, all but one intervention had an improvement in at least one workplace PAFootnote 3 outcome (Table 3; interventions 1–8, 10–17). The intervention (Table 3, intervention 9) that did not yield an increase in workplace or total PA had an increase in leisure time PA only. Twelve of the 17 interventions indicated significant improvements in at least one workplace PA3 outcome after the intervention (Table 3; interventions 1, 3, 4, 6, 8, 10–16). Seven of these interventions showed a significant effect over time (Table 3; interventions 1, 3, 4, 6, 8, 11, 16), and eight showed a significant effect against another intervention group (Table 3; interventions 8, 14) or against a control group (Table 3; interventions 1, 6, 10, 12–15).
Risk of Bias
After the initial assessment of risk of bias, the two raters who assessed study quality had an overall agreement on RoB 2 of 84.2% and on ROBINS-I of 92.9%. After a discussion meeting, there was agreement on all domains of the two instruments (Fig. 3 and 4).
Of nine RCTs assessed with the RoB 2 tool, five studies (Table 3; interventions 3, 10, 11, 12, 15) received a high risk of bias rating. The other four studies (Table 3; interventions 7–9, 13, 14, 16, 17) were rated as having some concerns. Study limitations and consequently a high risk of bias were due to deviations from intended interventions, missing outcome data, and the inappropriate measurement of outcomes.
Of five non-RCTs evaluated using the ROBINS-I tool, one (Table 3, intervention 1) received a critical risk of bias rating and the other four (Table 3; interventions 2, 4, 5, 6) a moderate risk of bias rating. Among the non-RCTs, the limitations of studies associated with a high risk of bias were due to deviations from intended interventions and due to confounding.
Discussion
The aim of this review was to summarize previous workplace PA coaching interventions that aim to increase health-enhancing PA in the workplace. Included studies were longitudinal intervention studies. The intervention had to be PA coaching in the workplace, which had to be either web-/telephone-/mobile-based, or in person. The coaching had to include at least one interaction between coach and coachee, and it could either be individual or group coaching. The intervention had to aim at increasing health-enhancing PA in the workplace (plus optional leisure time PA, subjectively and/or objectively assessed) and be addressed toward sedentary employees. Thus, the present review provides an up-to-date overview of workplace PA coaching interventions, their compositions, and effectiveness.
As its main result, this review shows a wide variety of different compositions of PA coaching interventions in the workplace. These interventions varied greatly within the resources (e.g., organizational coaching parameters) and the activities (e.g., BCTs), thereby illustrating the diversity of PA coaching interventions implemented to date. In terms of outputs and outcomes, this review reveals that some studies have already used coaching in the workplace to increase PA. These studies showed positive effects on at least one PA outcome, but some showed only small changes. Overall, this review demonstrates the potential of PA coaching as a multifaceted workplace intervention with a high degree of individualization of parameters for different employee groups and different types of workplaces to increase PA.
In terms of the resources such as the organizational coaching parameters, this review found that a high variety of different communication channels (e.g., face-to-face/app/combinations) was integrated. Even though most studies substantiated their choice of communication channel, some did not provide any rationale (e.g., [51,52,53]). One good example are Poirier et al. [54], who substantiated their messaging intervention with benefits such as a great outreach at low cost and a “considerable public health impact” (p. 2). Other examples ([50]a, b.; [55]) integrated their e-coaching and PA into the work routines of employees to make the coaching as enjoyable and effective as possible. In order to understand the choice for a particular communication channel in a workplace PA coaching intervention, it is important that the rationale for this choice is also transparent to other researchers or practitioners.
Furthermore, it can be assumed that the resources communication channel and time scope parameters of coaching (e.g., the number of interactions) are interrelated, as, for example, coaching with an e-coach can provide "around-the-clock coaching" with many interactions in a shorter time period [45] in contrast to coaching with face-to-face contact. This "around-the-clock coaching" was found in interventions that used messaging, apps, or combinations thereof as communication channels (Fig. 2). However, e-coaching interventions based on messaging also eliminate the face-to-face contact that Wolever et al. [14] emphasize in their health coaching definition. The selection of the communication channel and consequently the number of interactions both depend on the specific coaching goals and organizational circumstances (e.g., the preferences and working routines of the target group, costs, or the technical possibilities).
In terms of activities, a variety of BCTs were used, but the reasons behind the choices for these techniques are crucial. Some researchers derived their BCTs theoretically or practically well. In terms of theory, SDT [51] and SCT [52] were used to derive BCTs. In terms of practical approaches, scholars [52, 56] used a practical community-based participatory research approach to engage the target population and/or other stakeholders. They identified and categorized the techniques needed to increase PA from the target population’s/stakeholders’ perspective. Other included interventions used pre-designed protocols/programs to develop their intervention, e.g., a PACE protocol (Patient-Centered Assessment and Counseling for Exercise protocol; Caparosa and Thompson 1999 in [57]) or the ALIVE program (A Lifestyle Intervention Via E-mail; Block et al. 2008 in [58]). In conclusion, there are different ways to justify integrated BCTs so far; however, there is no gold standard yet. Whether concept developers take the practical, theoretical or empirical route to justifying BCTs, it is particularly important to consider the target groups and individuals in the final developmental step.
It is difficult to draw conclusions about which BCTs and which combinations of BCTs are most effective due to the diversity as well as the interrelation of the different coaching parameters within the different interventions. This is consistent with a recent meta-review by Spring et al. [59], who similarly found little evidence for the isolated effectiveness of single BCTs in promoting PA, because there was no evidence for one BCT evaluated in more than one meta-analysis whose inclusion in PA interventions was associated with better outcomes.
Moreover, in some included studies—in addition to coaching—other activities such as organized voluntary interventions were implemented to increase workplace PA. Examples of these interventions include bike routes around campus ([60] a. & b.), treadmills in the workplace ([50] a. & b.), and sports promoters in departments [53, 60] a. & b.]. These interventions demonstrate that PA can be integrated well into the workplace. To conclude, the implementation of additional voluntary interventions can facilitate the increase in physical activity targeted by coaching and should always be considered in coaching concepts.
In addition to these voluntary workplace interventions, some interventions also integrated additional techniques to increase PA during leisure time, e.g., techniques that aim at increasing PA in the active transportation context or leisure context [58, 61] a. & b.]. Thus, workplace PA coaching ideally targets PA in all contexts, such as leisure and active transportation, so that a transfer effect can take place and a PA increase is present in each context.
Lastly, the included studies showed a great outreach to people of many age groups (up to retirement), different genders, sectors, and social classes. In this review, among others, employees of health care companies, pharmacies, but also universities, airlines, and ambulatory clinic services are represented. This overcomes the barrier to PA-enhancing interventions of limited accessibility to different groups of people [18] and shows that workplace PA coaching can address many different groups of people. However, groups of people that are typically not included in workplace PA coaching are unemployed persons, pensioners, self-employed persons, children, and young adolescents. Future reflection and research should therefore address workplace-like settings in which PA coaching can be integrated to reach these non-working target groups.
Although the included studies could not be meta-analyzed due to their wide diversity, they appear to have a positive impact on workplace PA. With the exception of one intervention, all interventions showed either positive effects for at least one workplace or total PA outcome (e.g., active transportation, total energy expenditure, or weekday step count) either over time or compared to other active or passive control groups. This output supports the evidence that coaching interventions are able to increase PA in sedentary employees just as in other target groups [40, 41]. Moreover, another output is acceptability of the included interventions that has been shown through relatively high response rates (M = 77%) which indicate high adherences of the target groups for intervention studies. Reasons for these high adherence rates could be, first, the interactivity, individuality, and person-centeredness that characterize the coaching interventions included here [14], and second, the many different coaching parameters described, each of which can be modified to suit the occupational target group.
Limitations
Limitations of this review relate primarily to the difficulty of comparing the included interventions. This difficulty has also been acknowledged in other reviews (e.g., [14]) and can mostly be attributed to two main issues: 1) the different goals of the interventions; and 2) the varying intervention descriptions.
The different goals of the interventions are problematic because they lead to different intervention implementations and different BCTs, making their comparability difficult. Some interventions only aim at evaluating PA coaching and related PA behavior, while other interventions additionally evaluate other behaviors, such as sedentary or dietary behavior or the improvement of parameters such as fat mass. In terms of PA and sedentary behavior, it can further be discussed to what extent there is a difference between increasing PA and decreasing sedentary behavior, because decreasing sedentary behavior actually also aims at increasing PA.
The varying intervention descriptions further complicate the comparison of the different interventions. In particular, some intervention descriptions [51, 54,55,56, 58, 62, 63] were formulated in a detailed and comprehensible manner. Inadequate intervention descriptions make replication studies infeasible and do not add much value to practitioners or other researchers. In some cases, intervention descriptions were not described properly and so inadequate that only one BCT could be detected and inferred (e.g., [57]), whereas others were detailed enough so that up to 9 BCTs could be identified [56].
In addition to the limitations concerning the intervention level, there are also some limitations that regard the study design, as the risk of bias results show. First, there were deviations from intended interventions, as both participants (in this case, coachees) and carers/people delivering the interventions (in this case, coaches) could not be blinded to a coaching intervention. Second, most study publications did not provide evidence that the results were not biased by missing outcome data. Third, some study results are limited due to problematic outcome measures, such as less feasible accelerometers (incorrect carrying position on body; [62]) or mere subjective measurement of PA ([60] a. & b.; [57, 58, 64]).
Two limitations that generally apply to reviews must also be considered when interpreting the results. First, our literature search was restricted to academic articles published in English and German. This may have resulted in the exclusion of relevant studies published in other languages or in gray literature sources. Second, there is a risk for publication bias, as interventions that yield a negative or insignificant outcome are less likely to be published [65].
Strengths
The strengths of this review are, on the one hand, the provision of the first general overview of the state of the literature on workplace PA coaching to increase PA in the workplace. Second, the Cochrane tools RoB 2 [48] and ROBINS-I [49] were used to assess the risk of bias. These are validated but challenging to implement even for raters with extensive experience [66, 67]. A third strength regards the high interrater reliability between the two raters of the studies (RoB 2: 84.2%, ROBINS-I: 92.9%).
Recommendations for Practice
Two features for recommendations for practice are particularly noteworthy when considering, in particular, those studies that show significant effects against a control group or another intervention group. The first feature of these studies is a combination of BCTs, more specifically goal setting, self-monitoring, and problem solving. These techniques have both a motivational, as well as a volitional focus, and therefore form a good basis for health behavior change [68]. The second feature concerns the communication channel. Face-to-face coaching alone or in combination with messaging, phone calls or an app should take precedence over digital-only coaching. Face-to-face enables a more intensive personal relationship, which Wolever et al. [14] already emphasized in their coaching definition.
Recommendations for Future Research
Some included studies provided inadequate intervention descriptions, making the actual coaching difficult to understand or replicate. A possible approach would be to use a unified language for BCTs as tools for coaching programs [69]. One possibility for a collection of such techniques would be the taxonomy by Michie et al. [32], which was developed in a Delphi survey with behavior change experts.
In addition to the insufficient intervention descriptions, many derivations of the interventions were not comprehensible. It is useful for both other researchers and practitioners to comprehend why specific techniques were used and combined with others to understand the theoretical mechanisms underlying the effects. One approach is to derive and combine different BCTs according to health behavior change theories (HAPA; [70]) by implementing motivational techniques (e.g., goal setting) to form the intention and volitional techniques (e.g., action planning) in order to support the implementation of this intention. As a second approach, some studies used a community-based participatory research approach with the help of group conversations (e.g., [56]) to develop the coaching intervention based on a needs assessment prospectively. Both approaches could be used in future coaching interventions to allow for the development of a coaching intervention that is tailored to the needs and desires of the participants.
Only a few included studies integrated a follow-up phase with additional measurements. These additional phases and measurements are important in order to evaluate the long-term effectiveness of future coaching interventions because only long-term intervention effects show lasting success.
The individual interventions included considered coaching resources (e.g., organizational coaching parameters), coaching activities (e.g., BCTs) and coaching outputs (increasing PA), but there is little information on the outcomes of the interventions, such as the psychological and physical improvements of increased physical activity behavior on well-being or job satisfaction. In this review, only one study [63] examined worker's productivity as an outcome. Future research should therefore also consider and co-evaluate the short-, medium-, and long-term effects of the interventions.
Conclusion
In conclusion, this overview shows that coaching has already been used in some studies to increase the PA of employees, all with positive effects in at least one variable, whereby some only led to low changes in certain variables. This paper is the first review to provide an overview of the current state of the literature on workplace PA coaching and shows a range of different coaching interventions and their compositions, including different resources (e.g., organizational coaching parameters) and activities (e.g., BCTs). Due to the resulting different coaching approaches, where each parameter can be changed individually, PA coaching in the workplace can contribute to the improvement of employees' PA. The workplace could thus become another coaching setting besides schools, health care organizations or community centers to counteract the lack of PA in everyone's daily life.
Data Availability
The data supporting this systematic review are from previously reported studies, which have been cited. The processed data are available from the corresponding author on reasonable request.
Notes
Some extracted data categories have different terms in the registered protocol. To report the data, more global terms were used in some cases because the data were more heterogeneous than initially thought (occupational group became professional sector, coaching sessions became coaching interactions). In other cases, more precise terms were used for a better understanding (other potential components addressed in coaching became other behaviors potentially addressed in coaching, medium of intervention became communication channel, and type of BCT became name of BCT, transport PA became active transportation).
The 14 included studies resulted in 17 interventions, since Opdenacker and Boen [60], Ribeiro et al. [61] ), and Tucker et al. [50] each included two intervention groups (e.g. [50]; a. & b.) relevant for this review. When we talk about Sample Characteristics, Study Design, Outcomes and Risk of Bias, we are referring to studies (but list the interventions in the parentheses). In all other paragraphs in the results section, we talk about the 17 interventions.
In some interventions, workplace PA is measured separately; in other interventions, it is measured as part of the total PA outcomes.
References
Finger JD, Mensik GBM, Lange C, Manz K. Gesundheitsfördernde körperliche Aktivität in der Freizeit bei Erwachsenen in Deutschland [Health-promoting leisure-time physical activity among adults in Germany]. J Health Monit 2017;2(2).
Martin S, Morrow JR, Jackson A, Dunn AL. Variables related to meeting the CDC/ACSM physical activity guidelines. Med Sci Sports Exerc. 2000;32:2087–2092.
World Health Organization. WHO guidelines on physical activity and sedentary behaviour: at a glance.; 2020. https://apps.who.int/iris/bitstream/handle/10665/337001/9789240014886-eng.pdf.
Warburton DER, Nicol CW, Bredin SSD. Health benefits of physical activity: the evidence. CMAJ. 2006;174(6):801–809.
Fine LJ, Philogene GS, Gramling R, Coups EJ, Sinha S. Prevalence of multiple chronic disease risk factors 2001. National Health Interview Survey. Am J Prev Med. 2004;27(2 Suppl):18–24.
Jeon CY, Lokken RP, Hu FB, van Dam RM. Physical activity of moderate intensity and risk of type 2 diabetes: a systematic review. Diabetes Care. 2007;30(3):744–752.
Mora S, Cook N, Buring JE, Ridker PM, Lee I-M. Physical activity and reduced risk of cardiovascular events: potential mediating mechanisms. Circulation. 2007;116(19):2110–2118.
Reiner M, Niermann C, Jekauc D, Woll A. Long-term health benefits of physical activity: A systematic review of longitudinal studies. BMC Public Health. 2013;13:813.
Sabiston CM, Brunet J. Reviewing the benefits of physical activity during cancer survivorship. Am J Lifestyle Med. 2012;6(2):167–177.
Fox KR. The influence of physical activity on mental well-being. Public Health Nutr 1999; 2(3a//3A): 411–418.
Paluska SA, Schwenk T. Physical activity and mental health: current concepts. Sports Med Open. 2000;29(3):167–180.
Frates EP, Moore MA, Lopez CN, McMahon GT. Coaching for behavior change in physiatry. Am J Phys Med Rehabil. 2011;90(12):1074–1082.
Olsen JM, Nesbitt BJ. Health coaching to improve healthy lifestyle behaviors: an integrative review. Am J Health Promot. 2010;25(1):e1–e12.
Wolever RQ, Simmons LA, Sforzo GA, et al. A systematic review of the literature on health and wellness coaching: Defining a key behavioral intervention in healthcare. Glob Adv Health Med. 2013;2(4):38–57.
Heath GW. The role of the public health sector in promoting physical activity: national, state, and local applications. J Phys Act Health. 2009;6(s2):S159–S167.
Heath GW, Parra DC, Sarmiento OL, et al. Evidence-based intervention in physical activity: lessons from around the world. The Lancet. 2012;380(9838):272–281.
Dugdill L, Brettle A, Hulme C, McCluskey S, Long AF. Workplace physical activity interventions: a systematic review. Int J Workplace Health Mgt. 2008;1(1):20–40.
Grimani A, Aboagye E, Kwak L. The effectiveness of workplace nutrition and physical activity interventions in improving productivity, work performance and workability: a systematic review. BMC Public Health. 2019;19(1):1676.
Hoare E, Stavreski B, Jennings GL, Kingwell BA. Exploring motivation and barriers to physical activity among active and inactive australian adults. Sports (Basel) 2017; 5(3).
Kruger J, Yore MM, Bauer DR, Kohl HW. Selected barriers and incentives for worksite health promotion services and policies. Am J Health Promot. 2007;21(5):439–447.
Workplace policy and management practices to improve the health and wellbeing of employees - Guidance and guidelines; 2015 [cited 2021 January 29] Available from: https://doi.org/10.1002/14651858.CD010395.pub2.
Katzmarzyk PT, Janssen I. The economic costs associated with physical inactivity and obesity in Canada: an update. Can J Appl Physiol. 2004;29(1):90–115.
Oldridge NB. Economic burden of physical inactivity: healthcare costs associated with cardiovascular disease. Eur J Cardiovasc Prev Rehabil. 2008;15(2):130–139.
Jex SM, Heinisch DA. Assessing the relationship between exercise and employee mental health: methodological concerns. In: Kerr JH, Griffiths A, Cox T, editors. Workplace health, employee fitness, and exercise. London: Taylor & Francis; 1996. p. 55–67.
Hayes E, McCahon C, Panahi MR, Hamre T, Pohlman K. Alliance not compliance: coaching strategies to improve type 2 diabetes outcomes. J Am Acad Nurse Pract. 2008;20(3):155–162.
op den Akker H, Klaassen R, op den Akker R, Jones VM, Hermens HJ. Opportunities for smart & tailored activity coaching. In: Rodrigues PP, editor. Opportunities for smart & tailored activity coaching; 2013. Piscataway, NJ: IEEE; 546–547.
Hayes E, Kalmakis KA. From the sidelines: coaching as a nurse practitioner strategy for improving health outcomes. J Am Acad Nurse Pract. 2007;19(11):555–562.
Engbers LH, van Poppel MNM, Chin A, Paw MJM, van Mechelen W. Worksite health promotion programs with environmental changes: a systematic review. Am J Prev Med. 2005;29(1):61–70.
Ryan RM, Deci EL. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol. 2000;55(1):68–78.
Prochaska JO, DiClemente CC. Transtheoretical therapy: toward a more integrative model of change. Psychotherapy. 1982;19(3):267–288.
Bandura A. Social foundations of thought and action: a social cognitive theory. Englewood Cliffs: Prentice-Hall Inc.; 1986.
Michie S, Richardson M, Johnston M, et al. The behavior change technique taxonomy (v1) of 93 hierarchically clustered techniques: building an international consensus for the reporting of behavior change interventions. Ann Behav Med. 2013;46(1):81–95.
Michie S, Abraham C, Whittington C, McAteer J, Gupta S. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychol. 2009;28(6):690–701.
Barrett S, Begg S, O’Halloran P, Kingsley M. A physical activity coaching intervention can improve and maintain physical activity and health-related outcomes in adult ambulatory hospital patients: the Healthy4U-2 randomised controlled trial. Int J Behav Nutr Phys Act. 2020;17(1):156.
Brodin N, Eurenius E, Jensen I, Nisell R, Opava CH. Coaching patients with early rheumatoid arthritis to healthy physical activity: a multicenter, randomized, controlled study. Arthritis Rheum. 2008;59(3):325–331.
Coultas DB, Jackson BE, Russo R, et al. Home-based physical activity coaching, physical activity, and health care utilization in chronic obstructive pulmonary disease. Chronic obstructive pulmonary disease self-management activation research trial secondary outcomes. Ann Am Thorac Soc. 2018;15(4):470–478.
van Hoecke A-S, Delecluse C, Opdenacker J, Lipkens L, Martien S, Boen F. Long-term effectiveness and mediators of a need-supportive physical activity coaching among Flemish sedentary employees. Health Promot Int. 2013;28(3):407–417.
Venditti EM, Wylie-Rosett J, Delahanty LM, Mele L, Hoskin MA, Edelstein SL. Short and long-term lifestyle coaching approaches used to address diverse participant barriers to weight loss and physical activity adherence. Int J Behav Nutr Phys Act. 2014;11:16.
Howlett N, Trivedi D, Troop NA, Chater AM. Are physical activity interventions for healthy inactive adults effective in promoting behavior change and maintenance, and which behavior change techniques are effective? A systematic review and meta-analysis. Transl Behav Med. 2019;9(1):147–157.
Kivelä K, Elo S, Kyngäs H, Kääriäinen M. The effects of health coaching on adult patients with chronic diseases: a systematic review. Patient Educ Couns. 2014;97(2):147–157.
Oliveira JS, Sherrington C, Amorim AB, Dario AB, Tiedemann A. What is the effect of health coaching on physical activity participation in people aged 60 years and over? A systematic review of randomised controlled trials. Br J Sports Med. 2017;51(19):1425–1432.
Ofli F, Kurillo G, Obdržálek Š, Bajcsy R, Jimison HB, Pavel M. Design and evaluation of an interactive exercise coaching system for older adults: lessons learned. IEEE J Biomed Health Inform. 2016;20(1):201–212.
Abraham C, Graham-Rowe E. Are worksite interventions effective in increasing physical activity? A systematic review and meta-analysis. Health Psychol Rev. 2009;3(1):108–144.
Page MJ, McKenzie JE, Bossuyt PM, The PRISMA, et al. statement: an updated guideline for reporting systematic reviews. BMJ. 2020. https://doi.org/10.1136/bmj.n71.
Kamphorst BA. E-coaching systems: what they are, and what they aren’t. Pers Ubiquit Comput. 2017;21(4):625–632.
Foster C. Guidelines for health-enhancing physical activity promotion programmes: UKK Institute for Health Promotion Research; 2000. Available from: https://www.panh.ch/hepaeurope/materials/Guidelines%20HEPA%20Europe.pdf .
Van Uffelen JG, Wong J, Chau JY, Van Der Ploeg HP, Riphagen I, Gilson ND, Burton NW, Healy GN, Thorp AA, Clark BK, Gardiner PA. Occupational sitting and health risks: a systematic review. Am J Prev Med. 2010;39(4):379–388.
Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898.
Sterne JAC, Hernán MA, Reeves BC, et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919.
Tucker S, Farrington M, Lanningham-Foster LM, et al. Worksite physical activity intervention for ambulatory clinic nursing staff. Workplace Health Saf. 2016;64(7):313–325.
Arrogi A, Schotte A, Bogaerts A, Boen F, Seghers J. Short- and long-term effectiveness of a three-month individualized need-supportive physical activity counseling intervention at the workplace. BMC Public Health. 2017;17(1):52.
Chae D, Kim S, Park Y, Hwang Y. The effects of an academic—workplace partnership intervention to promote physical activity in sedentary office workers. Workplace Health Saf. 2015;63(6):259–266.
Nooijen CFJ, Blom V, Ekblom Ö, et al. The effectiveness of multi-component interventions targeting physical activity or sedentary behaviour amongst office workers: a three-arm cluster randomised controlled trial. BMC Public Health. 2020;20(1):1329.
Poirier J, Bennett WL, Jerome GJ, et al. Effectiveness of an activity tracker- and internet-based adaptive walking program for adults: a randomized controlled trial. J Med Internet Res. 2016;18(2):e34.
Boerema S, van Velsen L, Hermens H. An intervention study to assess potential effect and user experience of an mHealth intervention to reduce sedentary behaviour among older office workers. BMJ Health Care Inform. 2019;26(1):e100014.
Gilson ND, Pavey TG, Wright OR, et al. The impact of an m-Health financial incentives program on the physical activity and diet of Australian truck drivers. BMC Public Health. 2017;17(1):467.
Proper KI, Hildebrandt VH, van der Beek AJ, Twisk JW, van Mechelen W. Effect of individual counseling on physical activity fitness and health. Am J Prev Med. 2003;24(3):218–226.
Sternfeld B, Block C, Quesenberry CP, et al. Improving diet and physical activity with ALIVE: a worksite randomized trial. Am J Prev Med. 2009;36(6):475–483.
Spring B, Champion KE, Acabchuk R, Hennessy EA. Self-regulatory behaviour change techniques in interventions to promote healthy eating, physical activity, or weight loss: a meta-review. Health Psychol Rev. 2021;15(4):508–539.
Opdenacker J, Boen F. Effectiveness of face-to-face versus telephone support in increasing physical activity and mental health among university employees. J Phys Act Health. 2008;5(6):830–843.
Ribeiro MA, Martins MA, Carvalho CRF. Interventions to increase physical activity in middle-age women at the workplace: a randomized controlled trial. Med Sci Sports Exerc. 2014;46(5):1008–1015.
Bort-Roig J, Chirveches-Pérez E, Giné-Garriga M, et al. An mHealth workplace-based “Sit Less, Move More” Program: impact on employees’ sedentary and physical activity patterns at work and away from work. Int J Environ Res Public Health. 2020;17(23):8844.
Lee S-H, Ha Y, Jung M, Yang S, Kang W-S. The effects of a mobile wellness intervention with fitbit use and goal setting for workers. Telemed J E Health. 2019;25(11):1115–1122.
Purath J, Michaels Miller A, McCabe G, Wilbur J. A brief intervention to increase physical activity in sedentary working women. CJNR. 2004;36(1):76–91.
Dwan K, Altman DG, Arnaiz JA, et al. Systematic review of the empirical evidence of study publication bias and outcome reporting bias. PLoS ONE. 2008;3(8):e3081.
Minozzi S, Cinquini M, Gianola S, Castellini G, Gerardi C, Banzi R. Risk of bias in nonrandomized studies of interventions showed low inter-rater reliability and challenges in its application. J Clin Epidemiol. 2019;112:28–35.
Minozzi S, Dwan K, Borrelli F, Filippini G. Reliability of the revised Cochrane risk-of-bias tool for randomised trials (RoB2) improved with the use of implementation instruction. J Clin Epidemiol. 2022;141:99–105.
Geidl W, Semrau J, Pfeifer K. Health behaviour change theories: contributions to an ICF-based behavioural exercise therapy for individuals with chronic diseases. Disabil Rehabil. 2014;36(24):2091–2100.
Michie S, Fixsen D, Grimshaw JM, Eccles MP. Specifying and reporting complex behaviour change interventions: the need for a scientific method. Implement Sci. 2009;4:40.
Schwarzer R. Modeling health behavior change: how to predict and modify the adoption and maintenance of health behaviors. Appl Psychol. 2008;57(1):1–29.
Acknowledgements
We would like to thank Stefanie Haberstock and Annika Breuker for their assistance with the bibliography and graphical preparation of data as well as Dorothee Schwieters for the linguistic advice.
Funding
Open Access funding enabled and organized by Projekt DEAL. No funding was received to assist with the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
Idea of the article: Angeli Gawlik, Jens Kleinert; Literature search: Angeli Gawlik, Aliza Neuhausen, Jonas Lüdemann; Data analysis: Angeli Gawlik, Jonas Lüdemann, Christian Zepp, Jens Kleinert; Quality assessment: Angeli Gawlik, Aliza Neuhausen, Christian Zepp; Draft: Angeli Gawlik, Jens Kleinert, Jonas Lüdemann; Review and editing: Angeli Gawlik, Jens Kleinert, Frank Vitinius, Jonas Lüdemann, Christian Zepp, Aliza Neuhausen.
Corresponding author
Ethics declarations
Competing interests
The authors have no competing interests to declare that are relevant to the content of this review.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gawlik, A., Lüdemann, J., Neuhausen, A. et al. A Systematic Review of Workplace Physical Activity Coaching. J Occup Rehabil 33, 550–569 (2023). https://doi.org/10.1007/s10926-023-10093-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10926-023-10093-8