Abstract
Introduction
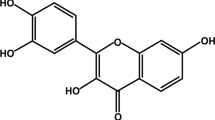
Neurodegenerative disorders are a diverse variety of diseases that can be distinguished from developing degeneration of neurons in the CNS. Several alkaloids have shown mounting effects in neurodegenerative disorders, and berberine is one of them. Demethyleneberberine is a metabolite of berberine that has better blood-brain barrier crossing capacity. Demethyleneberberine possesses anti-inflammatory, anti-oxidant, and mitochondrial targeting properties. However, neither the pharmacological action nor the molecular mechanism of action of demethyleneberberine on neurodegenerative disorders has been explored yet.
Materials and methods
A systematic literature review of PubMed, Medline, Bentham, Scopus, and EMBASE (Elseveier) databases was carried out with the help of keywords like “Demethyleneberberine; neuroinflammation; oxidative stress; Neuroprotective; Neurodegenerative disorders” till date.
Conclusion
This review focus on the neuroprotective potential of demethyleneberberine in neurodegenerative disorders by attenuating different pathways, i.e., NF-κB, MAPK, and AMPK signalling.



Similar content being viewed by others
Abbreviations
- DMB:
-
Demethyleneberberine
- BBR:
-
Berberine
- NDDs:
-
Neurodegenerative disorders
- CNS:
-
Central nervous system
- ROS:
-
Reactive oxygen species
- Ca2+ :
-
Calcium
- Htt:
-
Huntingtin
- NAFLD:
-
Non-Alcoholic Fatty Liver Disease
- ALD:
-
Alcohol liver disease
- MDA:
-
Malonaldehyde
- GSH:
-
Glutathione
- ECM:
-
Extracellular matrix
- MMPs:
-
Matrix metalloproteinases
- TIMPS:
-
Tissue inhibitors of metalloproteinases
- TGF-1:
-
Transforming growth factor-1
- CYP2E1:
-
Cytochrome P450 2E1
- HIF-1α:
-
Hypoxia-inducible factor 1-alpha
- iNOS:
-
Inducible nitric oxide synthase
- qPCR:
-
Quantitative polymerase chain reaction
- IHC:
-
Immunohistochemical
- TNF-α:
-
Tumour necrosis factor-alpha
- CO:
-
Cyclooxygenase
- IL:
-
Interleukin
- iNOS:
-
Inducible nitric oxide synthase
- NFT:
-
Neurofibrillary tangles
- TAA:
-
Thioacetamide
- MAPK:
-
Mitogen-activated protein kinase
- AMPK:
-
AMP-activated protein kinase
- MAO-B:
-
Monoamine oxidase-B
- UTI:
-
Ulinastatin
- CYP2E1:
-
Cytochrome P450 2E1
- MDA:
-
Malondialdehyde
- INF-γ:
-
Interferon-gamma
References
Tiwari P, Khan H, Singh TG, Grewal AK (2022) Poly (ADP-ribose) polymerase: an overview of mechanistic approaches and therapeutic opportunities in the management of stroke. Neurochem Res 18:1–23. https://doi.org/10.1007/s11064-022-03595-z
Khan H, Garg N, Singh TG, Kaur A, Thapa K (2022) Calpain inhibitors as potential therapeutic modulators in neurodegenerative diseases. Neurochem Res 4:1–25. https://doi.org/10.1007/s11064-021-03521-9
Sun AY, Wang Q, Simonyi A, Sun GY (2008) Botanical phenolics and brain health. Neuromol Med 10:259–274. https://doi.org/10.1007/s12017-008-8052-z
Hussain G, Rasul A, Anwar H, Aziz N, Razzaq A, Wei W, Ali M, Li J, Li X (2018) Role of plant derived alkaloids and their mechanism in neurodegenerative disorders. Int J Biol Sci 14:341. https://doi.org/10.7150/ijbs.23247
Strain JJ, Karim A, Caliendo G, Brodsky M, Lowe RS III, Himelein C (2003) Neurologic drug–psychotropic drug update. Dis Mon 49:326–371. https://doi.org/10.1067/mda.2003.25
Egbuna C, Mishra AP, Goyal MR (2020) Preparation of phytopharmaceuticals for the management of disorders: the development of nutraceuticals and traditional medicine. Academic Press, Cambridge
Schmitt F, Hussain G, Dupuis L, Loeffler JP, Henriques A (2014) A plural role for lipids in motor neuron diseases: energy, signaling and structure. Front Cell Neurosci 20(8):25. https://doi.org/10.3389/fncel.2014.00025
Akbar M, Shabbir A, Rehman K, Akash MS, Shah MA (2021) Neuroprotective potential of berberine in modulating Alzheimer’s disease via multiple signaling pathways. J Food Biochem 10:e13936. https://doi.org/10.1111/jfbc.13936
Kim M, Cho KH, Shin MS, Lee JM, Cho HS, Kim CJ, Shin DH, Yang HJ (2014) Berberine prevents nigrostriatal dopaminergic neuronal loss and suppresses hippocampal apoptosis in mice with Parkinson’s disease. Int J Mol Med 33:870–878. https://doi.org/10.3892/ijmm.2014.1656
Jiang W, Wei W, Gaertig MA, Li S, Li XJ (2015) Therapeutic effect of berberine on Huntington’s disease transgenic mouse model. PLoS ONE 10:e0134142. https://doi.org/10.1371/journal.pone.0134142
Liu YJ, Ju TC, Chen HM, Jang YS, Lee LM, Lai HL, Tai HC, Fang JM, Lin YL, Tu PH, Chern Y (2015) Activation of AMP-activated protein kinase α1 mediates mislocalization of TDP-43 in amyotrophic lateral sclerosis. Hum Mol Genet 24:787–801. https://doi.org/10.1093/hmg/ddu497
Hong JS, Chu YK, Lee H, Ahn BH, Park JH, Kim MJ, Lee S, Ryoo HS, Jang JH, Lee SR, Park JW (2012) Effects of berberine on hippocampal neuronal damage and matrix metalloproteinase-9 activity following transient global cerebral ischemia. J Neurosci Res 90:489–497. https://doi.org/10.1002/jnr.22756
Gao F, Gao Y, Liu YF, Wang L, Li YJ (2014) Berberine exerts an anticonvulsant effect and ameliorates memory impairment and oxidative stress in a pilocarpine-induced epilepsy model in the rat. Neuropsychiatr Dis Treat 10:2139. 10.2147%2FNDT.S73210
Pirillo A, Catapano AL (2015) Berberine, a plant alkaloid with lipid-and glucose-lowering properties: from in vitro evidence to clinical studies. Atherosclerosis 243:449–461. https://doi.org/10.1016/j.atherosclerosis.2015.09.032
Jiang W, Wei W, Gaertig MA, Li S, Li XJ (2015) Therapeutic effect of berberine on Huntington’s disease transgenic mouse model. PLoS ONE 30(10):e0134142. https://doi.org/10.1371/journal.pone.0134142
Wang J, Jiang Y, Wang B, Zhang N (2019) A review on analytical methods for natural berberine alkaloids. J Sep Sci 42:1794–1815. https://doi.org/10.1002/jssc.201800952
Gupta S, Khan A, Vishwas S, Gulati M, Singh TG, Dua K, Singh SK, Najda A, Sayed AA, Almeer R, Abdel-Daim MM (2021) Demethyleneberberine: a possible treatment for Huntington’s disease. Med Hypotheses 1(153):110639. https://doi.org/10.1016/j.mehy.2021.110639
Chen WW, Zhang XI, Huang WJ (2016) Role of neuroinflammation in neurodegenerative diseases. Mol Med Rep 13:3391–3396. https://doi.org/10.3892/mmr.2016.4948
Guzman-Martinez L, Maccioni RB, Andrade V, Navarrete LP, Pastor MG, Ramos-Escobar N (2019) Neuroinflammation as a common feature of neurodegenerative disorders. Front Pharmacol 12(10):1008. https://doi.org/10.3389/fphar.2019.01008
Pievan M, Filippini N, Van Den Heuvel MP, Cappa SF, Frisoni GB (2014) Brain connectivity in neurodegenerative diseases—from phenotype to proteinopathy. Nat Rev Neurol 10(11):620–633. https://doi.org/10.1038/nrneurol.2014.178
Gil-Bea F, Akterin S, Persson T, Mateos L, Sandebring A, Avila-Cariño J, Gutierrez-Rodriguez A, Sundström E, Holmgren A, Winblad B, Cedazo-Minguez A (2012) Thioredoxin-80 is a product of alpha-secretase cleavage that inhibits amyloid-beta aggregation and is decreased in Alzheimer’s disease brain. EMBO Mol Med 4(10):1097–1111. https://doi.org/10.1002/emmm.201201462
Rosenblum WI (2014) Why Alzheimer trials fail: removing soluble oligomeric beta amyloid is essential, inconsistent, and difficult. Neurobiol Aging 1(35):969–974. https://doi.org/10.1016/j.neurobiolaging.2013.10.085
Mogi M, Kondo T, Mizuno Y, Nagatsu T (2007) p53 protein, interferon-γ, and NF-κB levels are elevated in the parkinsonian brain. Neurosci Lett 27(414):94–97. https://doi.org/10.1016/j.neulet.2006.12.003
Khan H, Singh TG, Dahiya RS, Abdel-Daim MM (2022) α-Lipoic acid, an organosulfur biomolecule a novel therapeutic agent for neurodegenerative disorders: an mechanistic perspective. Neurochem Res 21:1–2. https://doi.org/10.1007/s11064-022-03598-w
Khan H, Tiwari P, Kaur A, Singh TG (2021) Sirtuin acetylation and deacetylation: a complex paradigm in neurodegenerative disease. Mol Neurobiol 58(8):3903–3917. https://doi.org/10.1007/s12035-021-02387-w
Chen CC, Hung TH, Lee CY, Wang LF, Wu CH, Ke CH, Chen SF (2014) Berberine protects against neuronal damage via suppression of glia-mediated inflammation in traumatic brain injury. PLoS ONE 29(9):e115694. https://doi.org/10.1371/journal.pone.0115694
Zhang P, Qiang X, Zhang M, Ma D, Zhao Z, Zhou C, Liu X, Li R, Chen H, Zhang Y (2015) Demethyleneberberine, a natural mitochondria-targeted antioxidant, inhibits mitochondrial dysfunction, oxidative stress, and steatosis in alcoholic liver disease mouse model. J Pharmacol Exp 352(1):139–147. https://doi.org/10.1124/jpet.114.219832
Chen YY, Li RY, Shi MJ, Zhao YX, Yan Y, Xu XX, Zhang M, Zhao XT, Zhang YB (2017) Demethyleneberberine alleviates inflammatory bowel disease in mice through regulating NF-κB signaling and T-helper cell homeostasis. J Inflamm Res 66(2):187–196. https://doi.org/10.1007/s00011-016-1005-3
Wang Y, Zhao Z, Yan Y, Qiang X, Zhou C, Li R, Chen H, Zhang Y (2016) Demethyleneberberine protects against hepatic fibrosis in mice by modulating NF-κB signaling. Int J Mol Sci 17(7):1036. https://doi.org/10.3390/ijms17071036
Khan H, Kashyap A, Kaur A, Singh TG (2020) Pharmacological postconditioning: a molecular aspect in ischemic injury. J Pharm Pharmacol 72(11):1513–1527. https://doi.org/10.1111/jphp.13336
Gandhi S, Abramov AY (2012) Mechanism of oxidative stress in neurodegeneration. Oxid Med Cell Longev. https://doi.org/10.1155/2012/428010
Khan H, Singh A, Thapa K, Garg N, Grewal AK, Singh TG (2021) Therapeutic modulation of the phosphatidylinositol 3-kinases (PI3K) pathway in cerebral ischemic injury. Brain Res 15(1761):147399. https://doi.org/10.1016/j.brainres.2021.147399
Qiang X, Xu L, Zhang M, Zhang P, Wang Y, Wang Y, Zhao Z, Chen H, Liu X, Zhang Y (2016) Demethyleneberberine attenuates non-alcoholic fatty liver disease with activation of AMPK and inhibition of oxidative stress. Biochem Biophys Res Commun 472(4):603–609. https://doi.org/10.1016/j.bbrc.2016.03.019
Zhang M, Li Q, Zhou C, Zhao Y, Li R, Zhang Y (2020) Demethyleneberberine attenuates concanavalin A-induced autoimmune hepatitis in mice through inhibition of NF-κB and MAPK signaling. Int Immunopharmacol 1(80):106137. https://doi.org/10.1016/j.intimp.2019.106137
Raghu G, Striker LJ, Hudson LD, Striker GE (1985) Extracellular matrix in normal and fibrotic human lungs. Am Rev Respir Dis 131(2):281–289. https://doi.org/10.1164/arrd.1985.131.2.281
Hemmann S, Graf J, Roderfeld M, Roeb E (2007) Expression of MMPs and TIMPs in liver fibrosis–a systematic review with special emphasis on anti-fibrotic strategies. J Hepatol 46(5):955–975. https://doi.org/10.1016/j.jhep.2007.02.003
Morawski M, Filippov M, Tzinia A, Tsilibary E, Vargova L (2014) ECM in brain aging and dementia. Prog Brain Res 214:207–227. https://doi.org/10.1016/B978-0-444-63486-3.00010-4
Xu L, He D, Bai Y (2016) Microglia-mediated inflammation and neurodegenerative disease. Mol Neurobiol 53(10):6709–6715. https://doi.org/10.1007/s12035-015-9593-4
Glass CK, Saijo K, Winner B, Marchetto MC, Gage FH (2010) Mechanisms underlying inflammation in neurodegeneration. Cell 140(6):918–934. https://doi.org/10.1016/j.cell.2010.02.016
Durairajan SS, Liu LF, Lu JH, Chen LL, Yuan Q, Chung SK, Huang L, Li XS, Huang JD, Li M (2012) Berberine ameliorates β-amyloid pathology, gliosis, and cognitive impairment in an Alzheimer’s disease transgenic mouse model. Neurobiol Aging 33:2903–2919. https://doi.org/10.1016/j.neurobiolaging.2012.02.016
Panahi N, Mahmoudian M, Mortazavi P, Hashjin GS (2013) Effects of berberine on β-secretase activity in a rabbit model of Alzheimer's disease. Arch Med Sci 9:146. 10.5114%2Faoms.2013.33354
Palomo V, Tosat-Bitrian C, Nozal V, Nagaraj S, Martin-Requero A, Martinez A (2019) TDP-43: a key therapeutic target beyond amyotrophic lateral sclerosis. ACS Chem Neurosci 10:1183–1196. https://doi.org/10.1021/acschemneuro.9b00026
Kim M, Shin MS, Lee JM, Cho HS, Kim CJ, Kim YJ, Choi HR, Jeon JW (2014) Inhibitory effects of isoquinoline alkaloid berberine on ischemia-induced apoptosis via activation of phosphoinositide 3-kinase/protein kinase B signaling pathway. Int Neurourol J 18:115. 10.5213%2Finj.2014.18.3.115
Bhutada P, Mundhada Y, Bansod K, Dixit P, Umathe S, Mundhada D (2010) Anticonvulsant activity of berberine, an isoquinoline alkaloid in mice. Epilepsy Behav 18:207–210. https://doi.org/10.1016/j.yebeh.2010.03.007
Zhang Y, Liu D, Yao X, Zhang Y (2021) DMTHB ameliorates memory impairment in Alzheimer's disease mice through inhibition of IL-16 signaling. https://doi.org/10.21203/rs.3.rs-882646/v1
Sharma VK, Mehta V, Singh TG (2020) Alzheimer’s disorder: epigenetic connection and associated risk factors. Curr Neuropharmacol 18(8):740–753. https://doi.org/10.2174/1570159X18666200128125641
Sharma VK, Singh TG (2020) CREB: a multifaceted target for Alzheimer’s disease. Curr Alzheimer Res 17(14):1280–1293. https://doi.org/10.2174/1567205018666210218152253
Karunaweera N, Raju R, Gyengesi E, Münch G (2015) Plant polyphenols as inhibitors of NF-κB induced cytokine production—a potential anti-inflammatory treatment for Alzheimer’s disease? Front Mol Neurosci 16(8):24. https://doi.org/10.3389/fnmol.2015.00024
Escarcega RO, Fuentes-Alexandro S, Garcia-Carrasco M, Gatica A, Zamora A (2007) The transcription factor nuclear factor-kappa B and cancer. Clin Oncol 19(2):154–161. https://doi.org/10.1016/j.clon.2006.11.013
Figuera-Losada M, Rojas C, Slusher BS (2014) Inhibition of microglia activation as a phenotypic assay in early drug discovery. J Biomol Screen 19(1):17–31. https://doi.org/10.1177/1087057113499406
Munoz L, Ammit AJ (2010) Targeting p38 MAPK pathway for the treatment of Alzheimer’s disease. Neuropharmacology 58(3):561–568. https://doi.org/10.1016/j.neuropharm.2009.11.010
Yang L, Jiang Y, Shi L, Zhong D, Li Y, Li J, Jin R (2020) AMPK: Potential therapeutic target for Alzheimer’s disease. Curr Protein Pept Sci 21(1):66–77. https://doi.org/10.2174/1389203720666190819142746
Sharma T, Kaur D, Grewal AK, Singh TG (2021) Therapies modulating insulin resistance in Parkinson’s disease: a cross talk. Neurosci Lett 18:135754. https://doi.org/10.1016/j.neulet.2021.135754
Charvin D, Medori R, Hauser RA, Rascol O (2018) Therapeutic strategies for Parkinson disease: beyond dopaminergic drugs. Nat Rev Drug Discov 17(11):804–822. https://doi.org/10.1038/nrd.2018.136
Armstrong MJ, Okun MS (2020) Diagnosis and treatment of Parkinson disease: a review. JAMA 323(6):548–560. https://doi.org/10.1001/jama.2019.22360
Jha SK, Jha NK, Kar R, Ambasta RK, Kumar P (2015) p38 MAPK and PI3K/AKT signalling cascades in Parkinson’s disease. Int J Mol Cell Med 4(2):67
Gui C, Ren Y, Chen J, Wu X, Mao K, Li H, Yu H, Zou F, Li W (2020) p38 MAPK-DRP1 signaling is involved in mitochondrial dysfunction and cell death in mutant A53T α-synuclein model of Parkinson’s disease. Toxicol Appl Pharmacol 1(388):114874. https://doi.org/10.1016/j.taap.2019.114874
Tobón-Velasco JC, Limón-Pacheco JH, Orozco-Ibarra M, Macías-Silva M, Vázquez-Victorio G, Cuevas E, Ali SF, Cuadrado A, Pedraza-Chaverrí J, Santamaría A (2013) RETRACTED: 6-OHDA-induced apoptosis and mitochondrial dysfunction are mediated by early modulation of intracellular signals and interaction of Nrf2 and NF-κB factors. Toxicology. https://doi.org/10.1016/j.tox.2012.12.011
Ghosh A, Roy A, Liu X, Kordower JH, Mufson EJ, Hartley DM, Ghosh S, Mosley RL, Gendelman HE, Pahan K (2007) Selective inhibition of NF-κB activation prevents dopaminergic neuronal loss in a mouse model of Parkinson’s disease. Proc Natl Acad Sci 104(47):18754–18759. https://doi.org/10.1073/pnas.0704908104
Curry DW, Stutz B, Andrews ZB, Elsworth JD (2018) Targeting AMPK signaling as a neuroprotective strategy in Parkinson’s disease. J Parkinsons Dis 8(2):161–181. https://doi.org/10.3233/JPD-171296
Schapira AH (2011) Monoamine oxidase B inhibitors for the treatment of Parkinson’s disease. CNS Drugs 25(12):1061–1071. https://doi.org/10.2165/11596310-000000000-00000
Tao C, Hu SQ, Chen J, Chen YJ, Sun KH, Cui GZ, Ma M, Wu ZZ (2020) Highly efficient synthesis and monoamine oxidase B inhibitory profile of demethyleneberberine, columbamine and palmatine. Neurochem Int 139:104807. https://doi.org/10.1016/j.neuint.2020.104807
Testa CM, Jankovic J (2019) Huntington disease: a quarter century of progress since the gene discovery. J Neurol Sci 15(396):52–68. https://doi.org/10.1016/j.jns.2018.09.022
Mestre TA (2019) Recent advances in the therapeutic development for Huntington disease. Parkinsonism Relat Disord 59:125–130. https://doi.org/10.1016/j.parkreldis.2018.12.003
Yang X, Chu SF, Wang ZZ, Li FF, Yuan YH, Chen NH (2021) Ginsenoside Rg1 exerts neuroprotective effects in 3-nitropronpionic acid-induced mouse model of Huntington’s disease via suppressing MAPKs and NF-κB pathways in the striatum. Acta Pharmacol Sin 49:1409–1421. https://doi.org/10.1016/j.neulet.2007.09.056
Napolitano M, Zei D, Centonze D, Palermo R, Bernardi G, Vacca A, Calabresi P, Gulino A (2008) NF-kB/NOS cross-talk induced by mitochondrial complex II inhibition: implications for Huntington’s disease. Neurosci Lett 434:241–246. https://doi.org/10.1016/j.neulet.2007.09.056
Walter C, Clemens LE, Müller AJ, Fallier-Becker P, Proikas-Cezanne T, Riess O, Metzger S, Nguyen HP (2016) Activation of AMPK-induced autophagy ameliorates Huntington disease pathology in vitro. Neuropharmacology 108:24–38. https://doi.org/10.1016/j.neuropharm.2016.04.041
Arti AK, Singh M, Arora S, Dhiman S, Satija S, Singh TG (2019) Pharmacotherapy of amyotrophic lateral sclerosis: an insight. Plant Arch 19:1385–1397
Bucchia M, Ramirez A, Parente V, Simone C, Nizzardo M, Magri F, Dametti S, Corti S (2015) Therapeutic development in amyotrophic lateral sclerosis. Clin Ther 37:668–680. https://doi.org/10.1016/j.clinthera.2014.12.020
Sahana TG, Zhang K (2021) Mitogen-activated protein kinase pathway in amyotrophic lateral sclerosis. Biomedicines 9:969. https://doi.org/10.3390/biomedicines9080969
Hu H, Lin H, Duan W, Cui C, Li Z, Liu Y, Wang W, Wen D, Wang Y, Li C (2018) Intrathecal Injection of scAAV9–hIGF1 prolongs the survival of ALS model mice by inhibiting the NF-kB pathway. Neuroscience 381:1–10. https://doi.org/10.1016/j.neuroscience.2018.02.004
Coughlan KS, Mitchem MR, Hogg MC, Prehn JH (2015) “Preconditioning” with latrepirdine, an adenosine 5′-monophosphate-activated protein kinase activator, delays amyotrophic lateral sclerosis progression in SOD1G93A mice. Neurobiol Aging 36:1140–1150. https://doi.org/10.1016/j.neurobiolaging.2014.09.022
Jayaraj RL, Azimullah S, Beiram R, Jalal FY, Rosenberg GA (2019) Neuroinflammation: friend and foe for ischemic stroke. J Neuroinflammation 16:1–24. https://doi.org/10.1186/s12974-019-1516-2
Fann DY, Lim YA, Cheng YL, Lok KZ, Chunduri P, Baik SH, Drummond GR, Dheen ST, Sobey CG, Jo DG, Chen CL (2018) Evidence that NF-κB and MAPK signaling promotes NLRP inflammasome activation in neurons following ischemic stroke. Mol Neurobiol 55:1082–1096. https://doi.org/10.1007/s12035-017-0394-9
Chang D, Wang YC, Bai YY, Lu CQ, Xu TT, Zhu L, Ju S (2015) Role of P38 MAPK on MMP activity in photothrombotic stroke mice as measured using an ultrafast MMP activatable probe. Sci Rep 5:1–11. https://doi.org/10.1038/srep16951
Li X, Su L, Zhang X, Zhang C, Wang L, Li Y, Zhang Y, He T, Zhu X, Cui L (2017) Ulinastatin downregulates TLR4 and NF-kB expression and protects mouse brains against ischemia/reperfusion injury. Neurol Res 39:367–373. https://doi.org/10.1080/01616412.2017.1286541
Duan J, Cui J, Yang Z, Guo C, Cao J, Xi M, Weng Y, Yin Y, Wang Y, Wei G, Qiao B (2019) Neuroprotective effect of Apelin 13 on ischemic stroke by activating AMPK/GSK-3β/Nrf2 signaling. J Neuroinflammation 16:1–16. https://doi.org/10.1080/01616412.2017.1286541
Farrell JS, Wolff MD, Teskey GC (2017) Neurodegeneration and pathology in epilepsy: clinical and basic perspectives. J Neurodegener Dis. https://doi.org/10.1007/978-3-319-57193-5_12
De Simoni MG, Perego C, Ravizza T, Moneta D, Conti M, Marchesi F, De Luigi A, Garattini S, Vezzani A (2000) Inflammatory cytokines and related genes are induced in the rat hippocampus by limbic status epilepticus. Eur J Neurosci 12:2623–2633. https://doi.org/10.1046/j.1460-9568.2000.00140.x
Landgrave-Gómez J, Mercado-Gómez OF, Vázquez-García M, Rodríguez-Molina V, Córdova-Dávalos L, Arriaga-Ávila V, Miranda-Martínez A, Guevara-Guzmán R (2004) Anticonvulsant effect of time-restricted feeding in a pilocarpine-induced seizure model: metabolic and epigenetic implications. Front Cell Neurosci 10:7. https://doi.org/10.3389/fncel.2016.00007
Shao Y, Wang C, Hong Z, Chen Y (2016) Inhibition of p38 mitogen-activated protein kinase signaling reduces multidrug transporter activity and anti-epileptic drug resistance in refractory epileptic rats. J Neurochem 136:1096–1105. https://doi.org/10.1111/jnc.13498
Bulavin DV, Phillips C, Nannenga B, Timofeev O, Donehower LA, Anderson CW, Appella E, Fornace AJ (2004) Inactivation of the Wip1 phosphatase inhibits mammary tumorigenesis through p38 MAPK–mediated activation of the p16 Ink4a-p19 Arf pathway. Nat Genet 36:343–350. https://doi.org/10.1038/ng1317
Singh S, Singh TG, Rehni AK, Sharma V, Singh M, Kaur R (2021) Reviving mitochondrial bioenergetics: a relevant approach in epilepsy. Mitochondrion 58:213–226. https://doi.org/10.1016/j.mito.2021.03.009
Singh S, Singh TG, Rehni AK (2020) An insight into molecular mechanisms and novel therapeutic approaches in epileptogenesis. CNS Neurol Disord Drug Targets 19:750–779. https://doi.org/10.2174/1871527319666200910153827
Acknowledgements
The authors are grateful to the Chitkara College of Pharmacy, Chitkara University, Rajpura, Patiala, Punjab, India for providing the necessary facilities to carry out the research work.
Funding
Nil.
Author information
Authors and Affiliations
Contributions
Conceptualization: Conceived and designed the experiments: HK, AKG, TGS. Analyzed the data: SG, AKG, TGS. Wrote the manuscript: PS, HK. Editing of the manuscript: TGS. Critically reviewed the article: TGS.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Not applicable.
Patient consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Saklani, P., Khan, H., Singh, T.G. et al. Demethyleneberberine, a potential therapeutic agent in neurodegenerative disorders: a proposed mechanistic insight. Mol Biol Rep 49, 10101–10113 (2022). https://doi.org/10.1007/s11033-022-07594-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11033-022-07594-9