Abstract
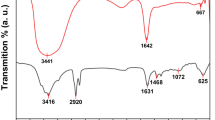
Nitric oxide (NO) is involved in several biological processes, including toxicity against tumor cells. The aim of this study was to synthesize, characterize, and evaluate the cytotoxicity of NO-releasing chitosan nanoparticles. A thiol-containing molecule, mercaptosuccinic acid (MSA), was encapsulated (encapsulation efficiency of 99%) in chitosan/sodium tripolyphosphate nanoparticles (CS NPs). The obtained nanoparticles showed an average hydrodynamic size of 108.40 ± 0.96 nm and polydispersity index of 0.26 ± 0.01. MSA-CS NPs were nitrosated leading to S-nitroso-MSA-CS NPs, which act as NO donor. The cytotoxicity of CS NPs, MSA-CS NPs, and S-nitroso-MSA-CS NPs were evaluated in several tumor cells, including human hepatocellular carcinoma (HepG2), mouse melanoma (B16F10), and human chronic myeloid leukemia (K562) cell lines and Lucena-1, a vincristine-resistant K562 cell line. Both CS NPs and MSA-CS NPs did not cause toxic effects in these cells, whereas S-nitroso-MSA-CS NPs caused potent cytotoxic effects in all the tested tumor cell lines. The half-maximal inhibitory concentration values of S-nitroso-MSA-CS NPs were 19.7, 10.5, 22.8, and 27.8 μg·mL−1 for HepG2, B16F10, K562, and Lucena-1 cells, respectively. In contrast, S-nitroso-MSA-CS NPs exhibited lower cytotoxic to non-tumorigenic melanocytes (Melan-A) when compared with melanoma B16F10. Therefore, the results highlight the potential use of NO-releasing CS NPs in antitumor chemotherapy.

Atomic force microscopy of chitosan nanoparticles for nitric oxide release






Similar content being viewed by others
References
Andrew PJ, Mayer B (1999) Enzymatic function of nitric oxide synthases. Cardiovasc Res 43(3):521–531
Antoniou J, Liu F, Majeed H, Qi J, Yokoyama W, Zhong F (2015) Physicochemical and morphological properties of size-controlled chitosan–tripolyphosphate nanoparticles. Colloids Surf A Physicochem Eng Asp 465:137–146. doi:10.1016/j.colsurfa.2014.10.040
Aranda A, Lopez-Pedrera C, Haba-Rodriguez J, Rodriguez-Ariza A (2012) Nitric oxide and cancer: the emerging role of S-nitrosylation. Curr Mol Med 12(1):50–67. doi:10.2174/156652412798376099
Basudhar D, Bharadwaj G, Cheng RY, Jain S, Shi S, Heinecke JL, Holland RJ, Ridnour LA, Caceres VM, Spadari-Bratfisch RC, Paolocci N, Velázquez-Martínez CA, Wink DA, Miranda KM (2013) Synthesis and chemical and biological comparison of nitroxyl- and nitric oxide-releasing diazeniumdiolate-based aspirin derivatives. J Med Chem 56(20):7804–7820. doi:10.1021/jm400196q
Basudhar D, Cheng RC, Bharadwaj G, Ridnour LA, Wink DA, Miranda KM (2015) Chemotherapeutic potential of diazeniumdiolate-based aspirin prodrugs in breast cancer. Free Radic Biol Med 83:101–114. doi:10.1016/j.freeradbiomed.2015.01.029
Bennett DC, Cooper PJ, Hart IR (1987) A line of non-tumorigenic mouse melanocytes, syngeneic with the B16 melanoma and requiring a tumour promoter for growth. Int J Cancer 39(3):414–418. doi:10.1002/ijc.2910390324
Bonavida B, Garban H (2015) Nitric oxide-mediated sensitization of resistant tumor cells to apoptosis by chemo-immunotherapeutics. Redox Biol 6:486–494. doi:10.1016/j.redox.2015.08.013
Bredt DS, Snyder SH (1994) Nitric oxide: a physiologic messenger molecule. Annu Rev Biochem 63:175–195. doi:10.1146/annurev.bi.63.070194.001135
Cardozo VF, Lancheros CA, Narciso AM, Valereto EC, Kobayashi RKT, Seabra AB, Nakazato G (2014) Evaluation of antibacterial activity of nitric oxide-releasing polymeric particles against Staphylococcus aureus and Escherichia coli from bovine mastitis. Int J Pharm 473:20–29. doi:10.1016/j.ijpharm.2014.06.051
Carpenter AW, Schoenfisch MH (2012) Nitric oxide release: part II. Therapeutic applications. Chem Soc Rev 41(10):3742–3752. doi:10.1039/c2cs15273h
Choi C, Nam JP, Nah JW (2015) Application of chitosan and chitosan derivatives as biomaterials. J Ind Eng Chem 33:1–10. doi:10.1016/j.jiec.2015.10.028
Costa P, Lobo JMS (2001) Modeling and comparison of dissolution profiles. Eur J Pharm Sci 13(2):123–133. doi:10.1016/S0928-0987(01)00095-1
de Faria PA, Bettanin F, Cunha RL, Paredes-Gamero EJ, Homem-de-Mello P, Rodrigues ILT (2015) Cytotoxicity of phenothiazine derivatives associated with mitochondrial dysfunction: a structure-activity investigation. Toxicology 330(1):44–54. doi:10.1016/j.tox.2015.02.004
de Oliveira MG, Shishido SM, Seabra AB, Morgon NH (2002) Thermal stability of primary S-nitrosothiols: roles of autocatalysis and structural effects on the rate of nitric oxide release. J Phys Chem A 106(38):8963–8970. doi:10.1021/jp025756u
dos Santos AC, Akkari AC, Ferreira IR, Maruyama CR, Pascoli M, Guilherme VA, de Paula E, Fraceto LF, Melo PS, de Araújo DR (2015) Poloxamer-based binary hydrogels for delivering tramadol hydrochloride: sol-gel transition studies, dissolution-release kinetics, in vitro toxicity, and pharmacological evaluation. Int J Nanomedicine 10:2391–2401. doi:10.2147/IJN.S72337
Dounighi MN, Eskandari R, Avadi MR, Zolfagharian H, Sadeghi MMA, Rezayat M (2012) Preparation and in vitro characterization of chitosan nanoparticles containing Mesobuthus eupeus scorpion venom as an antigen delivery system. J Venom Anim Toxins incl Trop Dis 18(1):44–52
Duong HTT, Kamarudin ZM, Erlich RB, Li Y, Jones MW, Kavallaris M, Boyer C, Davis TP (2013) Intracellular nitric oxide delivery from stable NO-polymeric nanoparticle carriers. Chem Commun 49:4190–4192. doi:10.1039/C2CC37181B
Elgadir MA, Uddin MS, Ferdosh S, Adam A, Chowdhury AJK, Sarker MZI (2015) Impact of chitosan composites and chitosan nanoparticle composites on various drug delivery systems: a review. J Food Drug Anal 23(4):619–629. doi:10.1016/j.jfda.2014.10.008
Ferreira DM, Saga YY, Aluicio-Sarduy E, Tedesco AC (2013) Chitosan nanoparticles for melanoma cancer treatment by photodynamic therapy and electrochemotherapy using aminolevulinic acid derivatives. Curr Med Chem 20(14):1904–1911. doi:10.2174/0929867311320140007
Gaucher C, Boudier A, Dahboul F, Parent M, Leroy P (2013) S-nitrosation/denitrosation in cardiovascular pathologies: facts and concepts for the rational design of S-nitrosothiols. Curr Pharm Des 19(3):458–472
Gothwal A, Khan I, Gupta U (2016) Polymeric micelles: recent advancements in the delivery of anticancer drugs. Pharm Res 33(1):18–39. doi:10.1007/s11095-015-1784-1
Grillo R, de Melo NFS, de Araújo SR, de Paula E, Rosa AH, Fraceto LH (2010) Polymeric alginate nanoparticles containing the local anesthetic bupivacaine. J Drug Target 18(9):688–699. doi:10.3109/10611861003649738
Gutiérrez V, Seabra AB, Reguera RM, Khandare J, Calderón M (2016) New approaches from nanomedicine for treating leishmaniasis. Chem Soc Rev 45:152–168. doi:10.1039/C5CS00674K
Howard MD, Hood ED, Zern B, Shuvaev VV, Grosser T, Muzykantov VR (2014) Nanocarriers for vascular delivery of anti-inflammatory agents. Annu Rev Pharmacol Toxicol 54:205–226. doi:10.1146/annurev-pharmtox-011613-140002
Huang J, Cheng ZH, Xie HH, Gong JY, Lou J, Ge Q, Wang YJ, Wu YF, Liu SW, Sun PL, Mao JW (2014) Effect of quaternization degree on physiochemical and biological activities of chitosan from squid pens. Int J Biol Macromol 70:545–550. doi:10.1016/j.ijbiomac.2014.07.017
Huerta S, Chilka S, Bonavida B (2008) Nitric oxide donors: novel cancer therapeutics (review). Int J Oncol 33(5):909–927
Hyduke DR, Liao JC (2005) Analysis of nitric oxide donor effectiveness in resistance vessels. Am J Physiol Hear Circ Physiol 288(5):2390–2399. doi:10.1152/ajpheart.00990.2004
Ignarro LJ (2000) Nitric oxide biology and pathobiology. Academic Press, San Diego
Iyer AKV, Rojansukul Y, Azad N (2014) Nitrosothiol signaling and protein nitrosation in cell death. Nitric Oxide 42(15):9–18. doi:10.1016/j.niox.2014.07.002
Jo YS, van der Vlies AJ, Gantz J, Thacher TN, Antonijevic S, Cavadini S, Demurtas S, Stergiopulos N, Hubbell JA (2009) Micelles for delivery of nitric oxide. J Am Chem Soc 131(40):14413–14418. doi:10.1021/ja905123
Katayama N, Nakajou K, Ishima Y, Ikuta S, Yokoe J, Yoshida F, Suenaga A, Maruyama T, Kai T, Otagiri M (2010) Nitrosylated human serum albumin (SNO-HSA) induces apoptosis in tumor cells. Nitric Oxide 22(4):259–265. doi:10.1016/j.niox.2009.09.003
Kim J, Saravanakumar G, Choi HW, Park D, Kim WJ (2014) A platform for nitric oxide delivery. J Mater Chem B 2:341–356. doi:10.1146/annurev-pharmtox-011613-140002
Kim JO, Noh JK, Thapa RK, Hasan N, Choi M, Kim JH, Lee JH, Ku SK, Yoo JW (2015) Nitric oxide-releasing chitosan film for enhanced antibacterial and in vivo wound-healing efficacy. Int J Biol Macromol 79:217–225. doi:10.1016/j.ijbiomac.2015.04.073
Kokubo T, Kushitani H, Sakka S, Kitsugi T, Yamamuro T (1990) Solutions able to reproduce in vivo surface-structure changes in bioactive glass-ceramic A-W. J Biomed Mater Res 24:721–734. doi:10.1002/jbm.820240607
Korsmeyer RW, Gurny R, Doelker E, Buri P, Peppas NA (1983) Mechanisms of solute release from porous hydrophilic polymers. Int J Pharm 15(1):25–35. doi:10.1016/0378-5173(83)90064-9
Kuang Y, Balakrishnan K, Gandhi V, Peng X (2011) Hydrogen peroxide inducible DNA cross-linking agents: targeted anticancer prodrugs. J Am Chem Soc 133(48):19278–19281. doi:10.1021/ja2073824
Lasker GF, Pankey EA, Kadowitz PJ (2013) Modulation of soluble guanylate cyclase for the treatment of erectile dysfunction. Physiology 28(4):262–269. doi:10.1152/physiol.00001.2013
Lu Y, Shah A, Hunter RA, Soto RJ, Schoenfisch MH (2015) S-nitrosothiol-modified nitric oxide-releasing chitosan oligosaccharides as antibacterial agents. Acta Biomater 12:62–69. doi:10.1016/j.actbio.2014.10.028
Marcato PD, Adami LF, Barbosa RM, Melo PS, Ferreira IS, de Paula L, Durán N, Seabra AB (2013) Development of a sustained-release system for nitric oxide delivery using alginate/chitosan nanoparticles. Curr Nanosci 9(1):1–7. doi:10.2174/1573413711309010003
Miller EW, Tulyathan O, Isacoff EY, Chang CJ (2007) Molecular imaging of hydrogen peroxide produced for cell signaling. Nat Chem Biol 3:263–267. doi:10.1038/nchembio871
Molina MM, Seabra AB, de Oliveira MG, Itri R, Haddad PS (2013) Nitric oxide donor superparamagnetic iron oxide nanoparticles. Mater Sci Eng C 33(2):746–751. doi:10.1016/j.msec.2012.10.027
Munaweera I, Shi Y, Koneru B, Patel A, Dang MH, di Pasqua AJ, Balkus KJ (2015) Nitric oxide- and cisplatin-releasing silica nanoparticles for use against non-small cell lung cancer. J Inorg Biochem 153:23–31. doi:10.1016/j.jinorgbio.2015.09.002
Ngo DG, Vo T, Ngo D, Kang K, Je J, Pham HN, Byun H, Kim S (2015) Biological effects of chitosan and its derivatives. Food Hydrocoll 51:200–216. doi:10.1016/j.foodhyd.2015.05.023
Nichols SP, Storm WL, Koh A, Schoenfisch MH (2012) Local delivery of nitric oxide: targeted delivery of therapeutics to bone and connective tissues. Adv Drug Deliv Rev 64(12):1177–1188. doi:10.1016/j.addr.2012.03.002
Okuyama K, Noguchi K, Hanafusa Y, Osawa K, Ogawa K (1999) Structural study of anhydrous tendon chitosan obtained via chitosan/acetic acid complex. Int J Biol Macromol 26(4):285–293. doi:10.1016/S0141-8130(99)00095-1
Oshiro A, Silva DC, de Mello JC, de Moraes VWR, Cavalcanti LP, Franco MKKD, Alkschbirs MI, Fraceto LF, Yokaichiya F, Rodrigues T, de Araújo DR (2014) Pluronics F-127/L-81 binary hydrogels as drug-delivery systems: influence of physicochemical aspects on release kinetics and cytotoxicity. Langmuir 30(45):13689–13698. doi:10.1021/la503021c
Pelegrino MT, Weller RB, Chen X, Bernardes JS, Seabra AB (2017) Chitosan nanoparticles for nitric oxide delivery in human skin. MedChemCommun. doi:10.1039/c6md00502k
Quinn JF, Whittaker MR, Davis TP (2015) Delivering nitric oxide with nanoparticles. J Control Release 205(10):190–205. doi:10.1016/j.jconrel.2015.02.007
Rapozzi V, Pietra ED, Zorzet S, Zacchigna M, Bonavida B, Xodo LE (2013) Nitric oxide-mediated activity in anti-cancer photodynamic therapy. Nitric Oxide 30:26–35. doi:10.1016/j.niox.2013.01.002
Reynolds MM, Witzeling SD, Damodaran VB, Medeiros TN, Knodle RD, Edwards MA, Lookian PP, Brown MA (2013) Applications for nitric oxide in halting proliferation of tumor cells. Biochem Biophys Res Commun 431(4):647–651. doi:10.1016/j.bbrc.2013.01.041
Riddles PW, Blakeley RL, Zerner B (1983) Reassessment of Ellman’s reagent. Methods Enzymol 91:49–60
Rodrigues FP, Carneiro ZA, Mascharak P, Curti C, da Silva RS (2016) Incorporation of a ruthenium nitrosyl complex into liposomes, the nitric oxide released from these liposomes and HepG2 cell death mechanism. Coord Chem Rev 306:701–707. doi:10.1016/j.ccr.2015.03.028
Santos MC, Seabra AB, Pelegrino MT, Haddad PS (2016) Synthesis, characterization and cytotoxicity of glutathione- and PEG-glutathione-superparamagnetic iron oxide nanoparticles for nitric oxide delivery. Appl Surf Sci 367:26–35. doi:10.1016/j.apsusc.2016.01.039
Saville SL, Stone RC, Qi B, Mefford OT (2012) Investigation of the stability of magnetite nanoparticles functionalized with catechol based ligands in biological media. J Mater Chem 22:24909–24917. doi:10.1039/C2JM34902G
Scicinski J, Oronsky B, Ning S, Knox S, Peehl D, Kim MM, Langecker P, Fanger G (2015) NO to cancer: the complex and multifaceted role of nitric oxide and the epigenetic nitric oxide donor, RRx-001. Redox Biol 6:1–8. doi:10.1016/j.redox.2015.07.002
Seabra AB, de Oliveira MG (2004) Poly(vinyl alcohol) and poly(vinyl pyrrolidone) blended films for local nitric oxide release. Biomaterials 25(17):3773–3782. doi:10.1016/j.biomaterials.2003.10.035
Seabra AB, de Souza GFP, da Rocha LL, Eberlin MN, de Oliveira MG (2004) S-nitrosoglutathione incorporated in poly(ethylene glycol) matrix: potential use for topical nitric oxide delivery. Nitric Oxide 11:263–272
Seabra AB, da Silva R, de Oliveira MG (2005) Polynitrosated polyesters: preparation, characterization, and potential use for topical nitric oxide release. Biomacromolecules 6(5):2512–2520. doi:10.1021/bm050216z
Seabra AB, Durán N (2010) Nitric oxide-releasing vehicles for biomedical applications. J Mater Chem 20:1624–1637. doi:10.1039/B912493B
Seabra AB, Martins D, Simões MMSG, da Silva R, Brocchi M, de Oliveira MG (2010) Antibacterial nitric oxide-releasing polyester for the coating of blood-contacting artificial materials. Artif Organs 34(7):204–214. doi:10.1111/j.1525-1594.2010.00998
Seabra AB, Durán N (2012) Nanotechnology allied to nitric oxide release materials for dermatological applications. Curr Nanosci 8:520–525. doi:10.2174/157341312801784159
Seabra AB, Pasquoto T, Ferrarini ACF, Santos MDC, Haddad PS, de Lima R (2014) Preparation, characterization, cytotoxicity, and genotoxicity evaluations of thiolated- and S-nitrosated superparamagnetic iron oxide nanoparticles: implications for cancer treatment. Chem Res Toxicol 27(7):1207–1218. doi:10.1021/tx500113u
Seabra AB, de Lima R, Calderon M (2015a) Nitric oxide releasing nanomaterials for cancer treatment: current status and perspectives. Curr Top Med Chem 15(4):298–308
Seabra AB, Justo GZ, Haddad PS (2015b) State of the art, challenges and perspectives in the design of nitric oxide-releasing polymeric nanomaterials for biomedical applications. Biotechnol Adv 33:1370–1379. doi:10.1016/j.biotechadv.2015.01.005
Seabra AB, Kitice NA, Pelegrino MT, Lancheros CAC, Yamauchi LM, Pinge-Filho P, Yamada-Ogatta SF (2015c) Nitric oxide-releasing polymeric nanoparticles against Trypanosoma cruzi. J Phys Conf Ser 617(1):12–20
Sharma K, Chakrapani H (2014) Site-directed delivery of nitric oxide to cancers. Nitric Oxide 43:8–16. doi:10.1016/j.niox.2014.07.005
Shishido SM, Seabra AB, Loh W, de Oliveira MG (2003) Thermal and photochemical nitric oxide release from S-nitrosothiols incorporated in Pluronic F127 gel: potential uses for local and controlled nitric oxide release. Biomaterials 24(20):3543–3553
Sipoli CC, Santana N, Shimojo AAM, Azzoni A, Torre LG (2015) Scalable production of highly concentrated chitosan/TPP nanoparticles in different pHs and evaluation of the in vitro transfection efficiency. Biochem Eng J 94:65–73. doi:10.1016/j.bej.2014.11.008
Suchyta DJ, Schoenfisch MH (2015) Encapsulation of N-diazeniumdiolates within liposomes for enhanced nitric oxide donor stability and delivery. Mol Pharm 12(10):3569–3574. doi:10.1021/acs.molpharmaceut.5b00248
Sun L, Du Y, Fan L, Chen X, Yang J (2006) Preparation, characterization and antimicrobial activity of quaternized carboxymethyl chitosan and application as pulp-cap. Polymer 47(6):1796–1804. doi:10.1016/j.polymer.2006.01.073
Tripathy S, Das S, Chakraborty SP, Sahu SK, Pramanik P, Roy S (2012) Synthesis, characterization of chitosan-tripolyphosphate conjugated chloroquine nanoparticle and its in vivo anti-malarial efficacy against rodent parasite: a dose and duration dependent approach. Int J Pharm 434:292–305. doi:10.1016/j.ijpharm.2012.05.064
Tsai M, Chen R, Bai S, Chen W (2011) The storage stability of chitosan/tripolyphosphate nanoparticles in a phosphate buffer. Carbohyd Polym 84:756–761. doi:10.1016/j.carbpol.2010.04.040
Venkatesan C, Vimal S, Hameed ASS (2013) Synthesis and characterization of chitosan tripolyphosphate nanoparticles and its encapsulation efficiency containing russell’s viper snake venom. J Biochem Mol Toxicol 27(8):406–411. doi:10.1002/jbt.21502
Wu W, Gaucher C, Diab R, Fries I, Xiao YL, Hu XM, Maincent P, Sapin-Minet A (2015) Time lasting S-nitrosoglutathione polymeric nanoparticles delay cellular protein S-nitrosation. Eur J Pharm Biopharm 89:1–8. doi:10.1016/j.ejpb.2014.11.005
Zou P, Yang X, Wang J, Li Y, Yu H, Zhang Y, Liu G (2016) Advances in characterization and biological activities of chitosan and chitosan oligosaccharides. Food Chem 190(1):1174–1181. doi:10.1016/j.foodchem.2015.06.076
Acknowledgements
This work was supported by FAPESP (Proc. 2016/10347-6, 2015/00393-8, 2014/13913-7), the Brazilian Network on Nanotoxicology (Grant number: 552120/2011-1) (MCTI/CNPq), the Laboratory of Nanostructure Synthesis and Biosystem Interactions-Nanobioss (MCTI) (Grant number: 402280-2013), Newton Advanced Fellowship (The Royal Society NA140046), Complexo Laboratorial Nanotecnológico (CLN)–UFABC–SisNano (Grant number: 402289/2013-7). The authors wish to thank Dr. Joyce C. Mello for helpful assistance with cytotoxicity measurements, Prof. Dr. Fabio Furlan Ferreira for his assistance with XRD measurements, Dr. Patrícia Fernanda Andrade for her assistance with scanning electron microscopy measurements, Dr. Juliana S. Bernardes for her assistance with AFM, and Genilce Scopiato Paganotti for revising the manuscript. The authors thank the Brazilian Nanotechnology National Laboratory/Center for Research in Energy and Materials (LNNano/CNPEM) for technical support AFM analyses.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Pelegrino, M.T., Silva, L.C., Watashi, C.M. et al. Nitric oxide-releasing nanoparticles: synthesis, characterization, and cytotoxicity to tumorigenic cells. J Nanopart Res 19, 57 (2017). https://doi.org/10.1007/s11051-017-3747-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11051-017-3747-4