Abstract
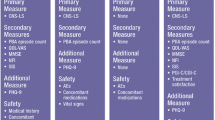
Pseudobulbar affect is a debilitating condition that significantly reduces quality of life for many individuals following traumatic brain injury (TBI). It is characterized by embarrassing and often uncontrollable episodes of crying or laughter. The aim of this systematic review was to evaluate the effectiveness of pharmacotherapy as compared to all other comparators for the management of pseudobulbar affect in adults who have sustained TBI. Six databases were searched, with additional hand searching of journals, clinical trials registries and international drug regulators to identify published and unpublished studies in English up to June 2018. Studies were eligible for this review if they included adults who had sustained a medically confirmed TBI and presented with pseudobulbar affect. All pharmacotherapy and comparator interventions were considered for inclusion, and study design was not limited to randomised controlled trials. Evidence quality was assessed using Joanna Briggs Institute Critical Appraisal Instruments. Two quasi-experimental studies examining the effectiveness of dextrometamorphan/quinidine (DM/Q) were identified. These studies reported that DM/Q was effective in reducing symptoms of pseudobulbar affect and had a positive safety profile, over follow-up periods of 3 months (n = 87) and 12 months (n = 23). However, both studies were limited by lack of a control group and a high dropout rate. The findings of twelve case reports examining the effectiveness of DM/Q (n = 6) and anti-depressants (n = 6) are also discussed. Further research is required to determine which pharmacological interventions provide the best outcomes for individuals with pseudobulbar affect following TBI, with consideration given to side effect profiles and financial costs.

Similar content being viewed by others
Abbreviations
- CT:
-
computed tomography
- CNS-LS:
-
Center for Neurologic studies Emotional Lability Scale
- DM/Q:
-
dextrometamorphan/quinidine
- Dur:
-
duration
- Freq:
-
Frequency
- GCS:
-
Glasgow Coma Scale
- HI:
-
head injury
- hrs:
-
hours
- JBI:
-
Joanna Briggs Institute
- MRI:
-
magnetic resonance imaging
- mths:
-
months
- NR:
-
not reported
- N/A:
-
not applicable
- PBA:
-
pseudobulbar affect
- PLCS:
-
Pathological Laughter and Crying Scale
- PRN:
-
pro re nata (i.e. as needed)
- PTA:
-
post traumatic amnesia
- RoB:
-
Risk of Bias
- SSRI:
-
selective serotonin reuptake inhibitor
- TBI:
-
traumatic brain injury
- TCA:
-
tricyclic anti-depressant
- wk.:
-
weeks
- yrs.:
-
years
References
Adams, J. H., Doyle, D., Ford, I., Gennarelli, T., Graham, D., & McLellan, D. (1989). Diffuse axonal injury in head injury: Definition, diagnosis and grading. Histopathology, 15(1), 49–59.
Ahmed, A., & Simmons, Z. (2013). Pseudobulbar affect: prevalence and management. Therapeutics and Clinical Risk Management, 9, 483–489. https://doi.org/10.2147/TCRM.S53906
Allman, P., Hope, R. A., & Fairburn, C. G. (1990). Emotionalism following brain damage: A complex phenomenon. Postgraduate Medical Journal, 66(780), 818–821.
Anderson, I. M. (2000). Selective serotonin reuptake inhibitors versus tricyclic antidepressants: A meta-analysis of efficacy and tolerability. Journal of Affective Disorders, 58(1), 19–36.
Arciniegas, D. B., Lauterbach, E. C., Ginsberg, D. L., Anderson, K. E., Chow, T. W., Flashman, L. A., et al. (2014). The differential diagnosis of Pseudobulbar affect (PBA): Distinguishing PBA among disorders of mood and affect. CNS Spectrums, 10(S5), 1–16. https://doi.org/10.1017/s1092852900026602
Arciniegas, D. B., & Wortzel, H. S. (2014). Emotional and behavioral dyscontrol after traumatic brain injury. Psychiatric Clinics of North America, 37(1), 31–53. https://doi.org/10.1016/j.psc.2013.12.001
Atkinson, K. M., Koenka, A. C., Sanchez, C. E., Moshontz, H., & Cooper, H. (2015). Reporting standards for literature searches and report inclusion criteria: Making research syntheses more transparent and easy to replicate. Research Synthesis Methods, 6(1), 87–95. https://doi.org/10.1002/jrsm.1127
Beller, E. M., Glasziou, P. P., Altman, D. G., Hopewell, S., Bastian, H., Chalmers, I., … PRISMA for Abstracts Group. (2013). PRISMA for abstracts: Reporting systematic reviews in journal and conference abstracts. PLoS Medicine, 10(4), e1001419. https://doi.org/10.1371/journal.pmed.1001419
Beresford, T. P., Arciniegas, D., Clapp, L., Martin, B., & Alfers, J. (2005). Reduction of affective lability and alcohol use following traumatic brain injury: A clinical pilot study of anti-convulsant medications. Brain Injury, 19(4), 309–313. https://doi.org/10.1080/02699050410001720121
Brooks, B. R., Crumpacker, D., Fellus, J., Kantor, D., & Kaye, R. E. (2013). PRISM: A novel research tool to assess the prevalence of pseudobulbar affect symptoms across neurological conditions. PLoS One, 8(8), e72232. https://doi.org/10.1371/journal.pone.0072232
Brooks, B. R., Thisted, R. A., Appel, S. H., Bradley, W. G., Olney, R. K., Berg, J. E., … AVP-923 ALS Study Group. (2004). Treatment of pseudobulbar affect in ALS with dextromethorphan/quinidine: A randomized trial. Neurology, 63(8), 1364–1370. https://doi.org/10.1212/01.WNL.0000142042.50528.2F
Chahine, L. M., & Chemali, Z. (2006). Du rire aux larmes: Pathological laughing and crying in patients with traumatic brain injury and treatment with lamotrigine. Epilepsy & Behavior, 8(3), 610–615. https://doi.org/10.1016/j.yebeh.2006.01.017
Chen, J. J. (2017). Pharmacotherapeutic management of pseudobulbar affect. American Journal of Managed Care, 23(18 Suppl), S345–S350.
Clay, F., Hicks, A. J., Perry, L. J., Ponsford, J. L., Jayaram, M., & Hopwood, M. (2018). Pharmacotherapy for the pseudobulbar affect in individuals who have sustained a traumatic brain injury: A systematic review protocol. JBI Database of Systematic Reviews and Implementation Reports, 9 In Press.
Colamonico, J., Formella, A., & Bradley, W. (2012). Pseudobulbar affect: Burden of illness in the USA. Advances in Therapy, 29(9), 775–798. https://doi.org/10.1007/s12325-012-0043-7
Cruz, M. P. (2013). Nuedexta for the treatment of pseudobulbar affect: A condition of involuntary crying or laughing. P T, 38(6), 325–328.
Cummings, J. L., Arciniegas, D. B., Brooks, B. R., Herndon, R. M., Lauterbach, E. C., Pioro, E. P., et al. (2014). Defining and diagnosing involuntary emotional expression disorder. CNS Spectrums, 11(S6), 1–11. https://doi.org/10.1017/s1092852900026614
Cummings, J., Gilbart, J., & Andersen, G. (2013). Pseudobulbar affect. A disabling but under-recognized consequence of neurological disease and brain injury. European Neurological Review, 8(2), 74–81.
Duda, J. E. (2014). History and prevalence of involuntary emotional expression disorder. CNS Spectrums, 12(S5), 6–10. https://doi.org/10.1017/s1092852900025955
Fellus, J., DeFina, P., Carson, C., Machado, C., & Chinchilla, M. (2014). Dextromethorphan/quinidine alleviates pseudobulbar affect and rapidly eliminates suicidal ideation in individuals with traumatic brain injury. Functional Neurology, Rehabilitation, and Ergonomics, 4(4), 253.
Fonda, J. R., Hunt, P. R., McGlinchey, R. E., Rudolph, J. L., Milberg, W. P., Reynolds, M. W., et al. (2015). Identification of pseudobulbar affect symptoms in veterans with possible traumatic brain injury. Journal of Rehabilitation Research and Development, 52(7), 839–849. https://doi.org/10.1682/JRRD.2014.08.0191
Garcia-Baran, D., Johnson, T. M., Wagner, J., Shen, J., & Geers, M. (2016). Therapeutic approach of a high functioning individual with traumatic brain injury and subsequent emotional volatility with features of pathological laughter and crying with dextromethorphan/quinidine. Medicine (Baltimore), 95(12), e2886. https://doi.org/10.1097/MD.0000000000002886
Gennarelli, T. A., Thibault, L. E., & Graham, D. I. (1998). Diffuse axonal injury: An important form of traumatic brain damage. The Neuroscientist, 4(3), 202–215.
Hammond, F. M., Alexander, D. N., Cutler, A. J., D’Amico, S., Doody, R. S., Sauve, W., et al. (2016). PRISM II: An open-label study to assess effectiveness of dextromethorphan/quinidine for pseudobulbar affect in patients with dementia, stroke or traumatic brain injury. BMC Neurology, 16(1), 89.
Hammond, F. M., Sauve, W., Ledon, F., Davis, C., & Formella, A. E. (2018). Safety, tolerability, and effectiveness of dextromethorphan/quinidine for Pseudobulbar affect among study participants with traumatic brain injury: Results from the PRISM-II open label study. PM&R.
Johnston, S. C., & Hauser, S. L. (2007). Marketing and drug costs: Who is laughing and crying? Annals of Neurology, 61(2), 11A–12A. https://doi.org/10.1002/ana.21100
Lawson, I. R., & MacLoed, R. D. (1969). The use of imipramine (" Tofranil") and other psychotropic drugs in organic emotionalism. The British Journal of Psychiatry, 115(520), 281–285.
Liberati, A., Altman, D. G., Tetzlaff, J., Mulrow, C., Gøtzsche, P. C., Ioannidis, J. P., … Moher, D. (2009). The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Medicine, 6(7), e1000100.
Lo, E. H., Singhal, A. B., Torchilin, V. P., & Abbott, N. J. (2001). Drug delivery to damaged brain. Brain Research. Brain Research Reviews, 38(1–2), 140–148. https://doi.org/10.1016/S0165-0173(01)00083-2
Miller, A., Pratt, H., & Schiffer, R. B. (2011). Pseudobulbar affect: The spectrum of clinical presentations, etiologies and treatments. Expert Review of Neurotherapeutics, 11(7), 1077–1088. https://doi.org/10.1586/ern.11.68
Moher, D. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Annals of Internal Medicine, 151(4), 264. https://doi.org/10.7326/0003-4819-151-4-200908180-00135
Moore, S. R., Gresham, L. S., Bromberg, M. B., Kasarkis, E. J., & Smith, R. A. (1997). A self report measure of affective lability. Journal of Neurology, Neurosurgery and Psychiatry, 63(1), 89–93.
Muller, U., Murai, T., Bauer-Wittmund, T., & von Cramon, D. Y. (1999). Paroxetine versus citalopram treatment of pathological crying after brain injury. Brain Injury, 13(10), 805–811.
Panitch, H. S., Thisted, R. A., Smith, R. A., Wynn, D. R., Wymer, J. P., Achiron, A., … Psuedobulbar Affect in Multiple Sclerosis Study Group. (2006). Randomized, controlled trial of dextromethorphan/quinidine for pseudobulbar affect in multiple sclerosis. Annals of Neurology, 59(5), 780–787. https://doi.org/10.1002/ana.20828
Parizel, P., Özsarlak, Ö., Van Goethem, J., Van Den Hauwe, L., Dillen, C., Verlooy, J., et al. (1998). Imaging findings in diffuse axonal injury after closed head trauma. European Radiology, 8(6), 960–965.
Parvizi, J. (2001). Pathological laughter and crying: A link to the cerebellum. Brain, 124(9), 1708–1719. https://doi.org/10.1093/brain/124.9.1708
Parvizi, J., Arciniegas, D. B., Bernardini, G. L., Hoffmann, M. W., Mohr, J. P., Rapoport, M. J., … Tuhrim, S. (2006). Diagnosis and management of pathological laughter and crying. Mayo Clinic Proceedings, 81(11), 1482–1486. https://doi.org/10.4065/81.11.1482
Parvizi, J., Coburn, K. L., Shillcutt, S. D., Coffey, C. E., Lauterbach, E. C., & Mendez, M. F. (2009). Neuroanatomy of pathological laughing and crying: A report of the American neuropsychiatric association committee on research. Journal of Neuropsychiatry and Clinical Neurosciences, 21(1), 75–87. https://doi.org/10.1176/appi.neuropsych.21.1.75
Pattee, G. L., Wymer, J. P., Lomen-Hoerth, C., Appel, S. H., Formella, A. E., & Pope, L. E. (2014). An open-label multicenter study to assess the safety of dextromethorphan/quinidine in patients with pseudobulbar affect associated with a range of underlying neurological conditions. Current Medical Research and Opinion, 30(11), 2255–2265. https://doi.org/10.1185/03007995.2014.940040
Pioro, E. P. (2011). Current concepts in the pharmacotherapy of pseudobulbar affect. Drugs, 71(9), 1193–1207. https://doi.org/10.2165/11591450-000000000-00000
Pioro, E. P., Brooks, B. R., Cummings, J., Schiffer, R., Thisted, R. A., Wynn, D., … Efficacy Results Trial of AVP-923 in PBA Investigators. (2010). Dextromethorphan plus ultra low-dose quinidine reduces pseudobulbar affect. Annals of Neurology, 68(5), 693–702. https://doi.org/10.1002/ana.22093
Plantier, D., Luaute, J., & Group, S. (2016). Drugs for behavior disorders after traumatic brain injury: Systematic review and expert consensus leading to French recommendations for good practice. Annals of Physical and Rehabilitation Medicine, 59(1), 42–57. https://doi.org/10.1016/j.rehab.2015.10.003
Presecki, P., & Mimica, N. (2007). Involuntary emotional expression disorder - new/old disease in psychiatry and neurology. Psychiatria Danubina, 19(3), 184–188.
Rabins, P. V., & Arciniegas, D. B. (2007). Pathophysiology of involuntary emotional expression disorder. CNS Spectrums, 12(4 Suppl 5), 17–22.
Robinson, R. G., Parikh, R. M., Lipsey, J. R., Starkstein, S. E., & Price, T. R. (1993). Pathological laughing and crying following stroke: Validation of a measurement scale and a double-blind treatment study. American Journal of Psychiatry, 150(2), 286–293. https://doi.org/10.1176/ajp.150.2.286
Robinson-Smith, G., & Grill, J. D. (2007, 2007/08//). Recognizing involuntary emotional expression disorder. [disease/disorder overview]. Journal of Neuroscience Nursing, p. 202+.
Rosen, H. (2008). Dextromethorphan/quinidine sulfate for pseudobulbar affect. Drugs Today (Barc), 44(9), 661–668. https://doi.org/10.1358/dot.2008.44.9.1258664
Roy, D., McCann, U., Han, D., & Rao, V. (2015). Pathological laughter and crying and psychiatric comorbidity after traumatic brain injury. Journal of Neuropsychiatry and Clinical Neurosciences, 27(4), 299–303. https://doi.org/10.1176/appi.neuropsych.15030045
Rudolph, J. L., Fonda, J. R., Hunt, P. R., McGlinchey, R. E., Milberg, W. P., Reynolds, M. W., et al. (2016). Association of Pseudobulbar Affect symptoms with quality of life and healthcare costs in veterans with traumatic brain injury. Journal of Affective Disorders, 190, 150–155. https://doi.org/10.1016/j.jad.2015.10.003
Sauve, W. M. (2016). Recognizing and treating pseudobulbar affect. CNS Spectrums, 21(S1), 34–44. https://doi.org/10.1017/S1092852916000791
Schiffer, R., & Pope, L. E. (2005). Review of pseudobulbar affect including a novel and potential therapy. Journal of Neuropsychiatry and Clinical Neurosciences, 17(4), 447–454. https://doi.org/10.1176/jnp.17.4.447
Schoedel, K. A., Morrow, S. A., & Sellers, E. M. (2014). Evaluating the safety and efficacy of dextromethorphan/quinidine in the treatment of pseudobulbar affect. Neuropsychiatric Disease and Treatment, 10, 1161–1174. https://doi.org/10.2147/NDT.S30713
Sloan, R., Brown, K., & Pentland, B. (1992). Fluoxetine as a treatment for emotional lability after brain injury. Brain Injury 6(4): 315–319
Tateno, A., Jorge, R. E., & Robinson, R. G. (2004). Pathological laughing and crying following traumatic brain injury. Journal of Neuropsychiatry and Clinical Neurosciences, 16(4), 426–434. https://doi.org/10.1176/jnp.16.4.426
Team, N. D. R. (2010). Risk assessment and risk mitigation review - 021879Orig1s000. In D. o. H. a. H. services (Ed.): Food and Drug Administration; Centre for Drug Evaluation Research
The Joanna Briggs Institute. (2014). Joanna Briggs institute reviewers’ manual (2014th ed.). Australia: The Joanna Briggs Institute.
Traumatic Brain Injury Medical Treatment Guidelines (2012). In D. O. W. C. Department of Labor and Employment (Ed.). State of Colorado.
Turner-Stokes, L., Hassan, N., Pierce, K., & Clegg, F. (2002). Managing depression in brain injury rehabilitation: The use of an integrated care pathway and preliminary report of response to sertraline. Clinical Rehabilitation, 16(3), 261–268. https://doi.org/10.1191/0269215502cr489oa
Werling, L. L., Keller, A., Frank, J. G., & Nuwayhid, S. J. (2007). A comparison of the binding profiles of dextromethorphan, memantine, fluoxetine and amitriptyline: Treatment of involuntary emotional expression disorder. Experimental Neurology, 207(2), 248–257. https://doi.org/10.1016/j.expneurol.2007.06.013
Willyerd, F. A., Empey, P. E., Kochanek, P. M., & Clark, R. S. (2014). Barriers to drug delivery for brain trauma. In Vascular Mechanisms in CNS Trauma (pp. 125-140): Springer.
Work, S. S., Colamonico, J. A., Bradley, W. G., & Kaye, R. E. (2011). Pseudobulbar affect: An under-recognized and under-treated neurological disorder. Advances in Therapy, 28(7), 586–601. https://doi.org/10.1007/s12325-011-0031-3
Wortzel, H. S., Oster, T. J., Anderson, C. A., & Arciniegas, D. B. (2008). Pathological laughing and crying : Epidemiology, pathophysiology and treatment. CNS Drugs, 22(7), 531–545.
Yang, L. P. H., & Deeks, E. D. (2015). Dextromethorphan/quinidine: A review of its use in adults with Pseudobulbar affect. Drugs, 75(1), 83–90. https://doi.org/10.1007/s40265-014-0328-z
Acknowledgements
The authors acknowledge with thanks the input of our information specialist Farhad Shokraneh in the design of search strategies.
Funding
The project was funded by the Transport Accident Commission (TAC) through the Institute for Safety, Compensation and Recovery Research (ISCRR).The funder was not involved in any other aspect of the project. This includes study design, data collection, analysis and interpretation of data, writing of the report or decision to submit the article for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
One of the chief investigators (MH) has given talks on this topic for which travel and accommodation has been paid by the organizers. In addition, he has accepted fees for consulting and research from the pharmaceutical companies Bionomics, Eli Lilly, Janssen-Cilag, Lundbeck, Novartis, Pfizer, Praxisand Servier. Lundbeck. All other authors declare no known competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 42 kb)
Appendix 1: Search strategy
Appendix 1: Search strategy
MEDLINE Search Strategy
-
1.
Exp Brain Hemorrhage, Traumatic/ OR Brain Injuries/ OR Brain Injury, Chronic/ OR Cerebral Hemorrhage, Traumatic/ OR Cerebrovascular Trauma/ OR Craniocerebral Trauma/ OR Diffuse Axonal Injury/ OR Exp Head Injuries, Closed/ OR Head Injuries, Penetrating/ OR Exp Intracranial Hemorrhage, Traumatic/ OR Exp Pneumocephalus/ OR (((Brain OR Cerebr$ OR Crani$ OR Crushing Skull OR Diffuse Axonal OR Head OR Hemisphere?) adj1 (Injur$ OR Trauma$)) OR ((Cerebr$ OR Crani$ OR Head) adj (Lesion? OR Wound?)) OR ((Posttraumatic OR Traumatic) adj Encephalopath$) OR (Traumatic adj (Brain OR Cerebr$)) OR Concuss$ OR DAI OR DAIs OR Pneumocephalus OR TBI OR TBIs).ti,ab.
-
2.
“Anti-Anxiety Agents”/ OR “Anticonvulsants”/ OR “Antidepressive Agents”/ OR “Antipsychotic Agents”/ OR “Benzodiazepines”/ OR “Adrenergic Beta-Antagonists”/ OR Alprazolam/ OR Amitriptyline/ OR Amoxapine/ OR Aripiprazole/ OR Atenolol/ OR Atomoxetine Hydrochloride/ OR Benztropine/ OR Bromazepam/ OR Bupropion/ OR Buspirone/ OR Carbamazepine/ OR Chlordiazepoxide/ OR Chlorpromazine/ OR Citalopram/ OR Clomipramine/ OR Clonazepam/ OR Clopenthixol/ OR Clorazepate Dipotassium/ OR Clozapine/ OR Desipramine/ OR Desvenlafaxine Succinate/ OR Dextroamphetamine/ OR Diazepam/ OR Valproic Acid/ OR Domperidone/ OR Dothiepin/ OR Doxepin/ OR Droperidol/ OR Duloxetine Hydrochloride/ OR Estazolam/ OR Eszopiclone/ OR Flunitrazepam/ OR Fluoxetine/ OR Flupenthixol/ OR Fluphenazine/ OR Fluvoxamine/ OR Guanfacine/ OR Haloperidol/ OR Imipramine/ OR Isocarboxazid/ OR Methotrimeprazine/ OR Lithium/ OR Lithium Carbonate/ OR Lorazepam/ OR Loxapine/ OR Lurasidone Hydrochloride/ OR Methylphenidate/ OR Mianserin/ OR Midazolam/ OR Moclobemide/ OR Molindone/ OR Nitrazepam/ OR Nortriptyline/ OR Oxazepam/ OR Paliperidone Palmitate/ OR Paroxetine/ OR Phenelzine/ OR Phenobarbital/ OR Pindolol/ OR Prazepam/ OR Pregabalin/ OR Prochlorperazine/ OR Promazine/ OR Promethazine/ OR Propranolol/ OR Protriptyline/ OR Quetiapine Fumarate/ OR Remoxipride/ OR Risperidone/ OR Selegiline/ OR Sertraline/ OR Sulpiride/ OR Temazepam/ OR Thioridazine/ OR Thiothixene/ OR Tranylcypromine/ OR Trazodone/ OR Triazolam/ OR Trifluoperazine/ OR Trimipramine/ OR Venlafaxine Hydrochloride/ OR Vigabatrin/ OR ((Adrenergic adj Beta adj2 (Antagonist OR Block$)) OR Anti Anxiety OR Anti Convuls$ OR Anti Depress$ OR Anti Epilep$ OR Anti Psychotic? OR Antianxiety OR Anticonvuls$ OR Antidepress$ OR Antiepilep$ OR Antipsychotic$ OR Anxiolytic$ OR Benzodiazepine$ OR (Beta adj Block$) OR (Beta adj1 Adrenergic adj2 Block$) OR Thymoanaleptic$ OR Thymoleptic$ OR Agomelatine OR “S 20098” OR S20098 OR Thymanax OR Valdoxan OR “AGO 178” OR AGO178 OR Alprazolam OR Alprazolan OR “Apo Alpraz” OR ApoAlpraz OR Cassadan OR “D 65MT” OR D65MT OR Xanax OR Tafil OR Trankimazin OR “Novo Alprazol” OR NovoAlprazol OR “Nu Alpraz” OR NuAlpraz OR Ralozam OR “U-31,889” OR “U31,889” OR Alprox OR Esparon OR Kalma OR Amisulpride OR Sultopride OR Barnetil OR “DAN 2163” OR Solian OR “LIN 1418” OR Amitriptyline OR Amineurin OR Amitrip OR Amitriptylin OR Amitrol OR Tryptine OR ApoAmitriptyline OR Damilen OR Domical OR Laroxyl OR Endep OR Lentizol OR Novoprotect OR Saroten OR Sarotex OR Syneudon OR Triptafen OR Tryptizol OR Tryptanol OR Elavil OR Anapsique OR Amoxapine OR Desmethylloxapine OR “CL 67,772” OR “CL67,772” OR Demolox OR Asendin OR Defanyl OR Asendis OR Aripiprazole OR Aripiprazol OR “OPC 14597” OR Abilify OR Asenapine OR Saphris OR “ OR G 5222” OR Atenolol OR Tenormine OR Tenormin OR “ICI 66082” OR ICI66082 OR Atomoxetine OR Tomoxetine OR Strattera OR “LY 139603” OR Benztropine OR Benzatropine OR Bensylate OR PMSBenztropine OR Cogentin OR Cogentinol OR Methylbenztropine OR ApoBenztropine OR Brexpiprazole OR Bromazepam OR BromaLich OR “Bromaz 1A Pharma” OR Bromazanil OR “Bromazep von CT” OR Durazanil OR Lexotan OR Lexotanil OR Lexatin OR Lexomil OR “Ro 5–3350” OR “Ro 53,350” OR Anxyrex OR Bupropion OR Amfebutamone OR Zyntabac OR Quomen OR Wellbutrin OR Zyban OR Buspirone OR “MJ 9022 1” OR MJ90221 OR Neurosine OR Busp OR Anxut OR Buspar OR Bespar OR Carbamazepine OR Tegretol OR Carbazepin OR Epitol OR Finlepsin OR Neurotol OR Amizepine OR Cariprazine OR “RGH 188” OR Chlordiazepoxide OR Methaminodiazepoxide OR Librium OR Chlozepid OR Elenium OR Chlorpromazine OR Thorazine OR Aminazine OR Largactil OR Chlordelazine OR Contomin OR Fenactil OR Propaphenin OR Chlorazine OR Citalopram OR Cytalopram OR “Lu 10 171” OR Lu10171 OR Escitalopram OR Lexapro OR Clobazam OR “HR 376” OR Onfi OR “LM 2717” OR Frisium OR Urbanyl OR Clomipramine OR Chlomipramine OR Chlorimipramine OR Hydiphen OR Anafranil OR Clonazepam OR “Ro 5 4023” OR “Ro 54,023” OR Antelepsin OR Rivotril OR Clopenthixol OR Zuclopenthixol OR Cisordinol OR Clorazepate OR Chlorazepate OR Tranxene OR Tranxilium OR “4306 CB” OR Clozapine OR Clozaril OR Leponex OR Desipramine OR Desmethylimipramine OR Demethylimipramine OR Norpramin OR Pertofrane OR Pertrofran OR Pertofran OR Petylyl OR Desvenlafaxine OR “O Desmethylvenlafaxine” OR “WY 45,233” OR “WY 45,233” OR “WY45,233” OR “WY 45233” OR WY45233 OR Pristiq OR Dextroamphetamine OR Dexamphetamine OR Dexamfetamine OR “Dextro Amphetamine” OR “D Amphetamine” OR Dexedrine OR DextroStat OR Oxydess OR Diazepam OR Diazemuls OR Faustan OR Valium OR Seduxen OR Sibazon OR Stesolid OR Apaurin OR Relanium OR “Valproic Acid” OR Divalproex OR “Propylisopropylacetic Acid” OR “2 Propylpentanoic Acid” OR Convulsofin OR Depakene OR Depakine OR Depakote OR Vupral OR Valproate OR Ergenyl OR “Dipropyl Acetate” OR Domperidone OR Domperidon OR Domidon OR Gastrocure OR Motilium OR Nauzelin OR Peridys OR “R 33,812” OR “R33,812” OR “R 33812” OR R33812 OR Dothiepin OR Dosulepin OR Prothiaden OR Doxepin OR Deptran OR Desidox OR Doneurin OR Doxepia OR Espadox OR Mareen OR Prudoxin OR Quitaxon OR Sinequan OR Sinquan OR Zonalon OR Xepin OR Aponal OR ApoDoxepin OR Droperidol OR Inapsine OR Dehidrobenzperidol OR Dehydrobenzperidol OR Droleptan OR Duloxetine OR “LY 248686” OR LY248686 OR “LY 227942” OR LY227942 OR Cymbalta OR Estazolam OR Tasedan OR ProSom OR “D 40TA” OR D40TA OR Nuctalon OR Eszopiclone OR Lunesta OR Estorra OR Flunitrazepam OR Fluridrazepam OR Flunibeta OR Flunimerck OR Fluninoc OR Rohypnol OR Rohipnol OR Narcozep OR “Flunizep von CT” OR “RO 5 4200” OR RO54200 OR Fluoxetine OR Fluoxetin OR “Lilly 110,140” OR Lilly110140 OR Sarafem OR Prozac OR Flupenthixol OR Flupentixol OR Emergil OR Fluanxol OR Fluphenazine OR Flufenazin OR Lyogen OR Prolixin OR Fluvoxamine OR Fluvoxadura OR Fluvoxamin OR Fluvoxamina OR Luvox OR Fevarin OR Floxyfral OR Dumirox OR Faverin OR Desiflu OR “DU 23000” OR DU23000 OR Guanfacine OR Tenex OR Lon798 OR “BS 100 141” OR BS100141 OR Estulic OR Haloperidol OR Haldol OR Iloperidone OR Zomaril OR Fanapt OR “HP 873” OR Imipramine OR Imizin OR Norchlorimipramine OR Imidobenzyle OR Tofranil OR Melipramine OR Pryleugan OR Janimine OR Isocarboxazid OR Lamotrigine OR Crisomet OR Lamictal OR Lamiktal OR “BW 430C” OR Labileno OR Methotrimeprazine OR Levomepromazine OR Levopromazine OR Levomeprazin OR Tisercin OR Tizercine OR Tizertsin OR Lithium OR Dilithium OR Lithane OR Lithobid OR Lithonate OR “CP-15,467 61” OR “CP15,46,761” OR Micalith OR “NSC 16895” OR NSC16895 OR Priadel OR “Quilinorm Retard” OR Quilinormretard OR Eskalith OR Lithotabs OR Lorazepam OR Ativan OR Temesta OR “Orfidal Wyeth” OR Donix OR Duralozam OR Durazolam OR Idalprem OR Laubeel OR “Lorazep von CT” OR “Novo Lorazem” OR NovoLorazem OR “Nu Loraz” OR NuLoraz OR Sedicepan OR Sinestron OR Somagerol OR Tolid OR “WY 4036” OR WY4036 OR ApoLorazepam OR Loxapine OR Cloxazepine OR Oxilapine OR Loxitane OR Loxipine OR Loxapinsuccinate OR “CL 71,563” OR “CL71,563” OR Lurasidone OR “SM 13496” OR SM13496 OR “SM-13,496” OR “SM13,496” OR Latuda OR Methylphenidate OR Metadate OR Equasym OR Methylin OR Concerta OR Phenidylate OR Ritalin OR Ritaline OR Tsentedrin OR Centedrin OR Daytrana OR Mianserin OR Tolvon OR Lerivon OR Org GB 94 OR Midazolam OR Dormicum OR Versed OR “Ro 21 3981” OR “Ro 213,981” OR Milnacipran OR Midalcipran OR Levomilnacipran OR Savella OR “F 2207” OR Ixel OR Mirtazapine OR “6 Azamianserin” OR Esmirtazapine OR Remeron OR Remergil OR Zispin OR Norset OR Rexer OR “Org 50,081” OR “ OR G 3770” OR Moclobemide OR Moclobamide OR Arima OR Aurorix OR Manerix OR Moclamine OR Aurorex OR Deprenorm OR Feraken OR Moclobemid OR Moclobeta OR Moclodura OR Moclonorm OR Rimoc OR “Ro 11 1163” OR Modafinil OR Benzhydrylsulfinylacetamide OR “CRL 40476” OR Vigil OR Provigil OR Sparlon OR Alertec OR Modiodal OR Molindone OR Moban OR Nefazodone OR Rulivan OR Serzone OR Dutonin OR Nefadar OR Menfazona OR Nitrazepam OR Nitrodiazepam OR “Dormo Puren” OR Eatan OR Imadorm OR Imeson OR Mogadon OR Nitrazadon OR Nitrazep OR Novanox OR Radedorm OR Remnos OR Serenade OR Somnite OR Alodorm OR Dormalon OR Nortriptyline OR Desmethylamitriptylin OR Desitriptyline OR Aventyl OR Paxtibi OR Allegron OR Norfenazin OR Pamelor OR Nortrilen OR Olanzapine OR Zolafren OR “LY 170052” OR Zyprexa OR “LY 170053” OR Oxazepam OR Serax OR Tazepam OR Adumbran OR Oxcarbazepine OR Timox OR Trileptal OR “GP 47680” OR Paliperidone OR “9 OH Risperidone” OR “9 Hydroxy Risperidone” OR “9 Hydroxyrisperidone” OR Invega OR “R 76477” OR R76477 OR Paroxetine OR “BRL 29060” OR BRL29060 OR “FG 7051” OR FG7051 OR Seroxat OR Paxil OR Aropax OR Periciazine OR Propericiazine OR Pericyazine OR Neuleptil OR Neuleptyl OR Aolept OR Phenelzine OR “Beta Phenylethylhydrazine” OR “2 Phenethylhydrazine” OR Fenelzin OR Phenethylhydrazine OR Nardelzine OR Nardil OR Phenobarbital OR Phenobarbitone OR “Phenylethylbarbituric Acid” OR Phenemal OR Phenylbarbital OR Hysteps OR Luminal OR Gardenal OR Pindolol OR Prindolol OR Visken OR “LB 46” OR LB46 OR Prazepam OR Lysanxia OR Reapam OR Centrax OR Demetrin OR Pregabalin OR “3 Isobutyl GABA” OR Lyrica OR “CI 1008” OR CI1008 OR Prochlorperazine OR Compazine OR Promazine OR Sparine OR Sinophenin OR Protactyl OR Promethazine OR Prometazin OR Proazamine OR Rumergan OR Diprazin OR Phenergan OR Phenargan OR Phensedyl OR Pipolfen OR Pipolphen OR Promet OR Prothazin OR Pyrethia OR Remsed OR Atosil OR Diphergan OR Propranolol OR Propanolol OR Inderal OR Avlocardyl OR “AY 20694” OR AY20694 OR Rexigen OR Dexpropranolol OR Dociton OR Obsidan OR Obzidan OR Anaprilin OR Anapriline OR Betadren OR Protriptyline OR Vivactil OR Quetiapine OR “ICI 204,636” OR “ICI 204636” OR ICI204636 OR Seroquel OR Reboxetine OR Vestra OR Remoxipride OR “FLA 731” OR FLA731 OR Risperidone OR Risperdal OR Risperidal OR “R 64,766” OR “R64,766” OR “R 64766” OR R64766 OR Selegiline OR Selegyline OR “L Deprenyl” OR “E 250” OR E250 OR Eldepryl OR Emsam OR Zelapar OR Deprenil OR Deprenalin OR Yumex OR Jumex OR Humex OR Deprenyl OR Sertindole OR Serlect OR “Lu 23 174” OR Serdolect OR Sertraline OR Zoloft OR Altruline OR Lustral OR Aremis OR Besitran OR Sealdin OR Gladem OR Sulpiride OR Sulperide OR Arminol OR Deponerton OR Meresa OR Desisulpid OR Digton OR Dogmatil OR Dolmatil OR Eglonyl OR Ekilid OR Guastil OR Lebopride OR Neogama OR Pontiride OR Psicocen OR Sulp OR Sulpitil OR Sulpivert OR Sulpor OR Synedil OR Tepavil OR Aiglonyl OR Temazepam OR Hydroxydiazepam OR Methyloxazepam OR Signopam OR Tenox OR “WY 3917” OR WY3917 OR Dasuen OR Euhypnos OR Levanxol OR “Norkotral Tema” OR Normison OR Nocturne OR Temtabs OR Normitab OR Nortem OR Planum OR “Pronervon T” OR Remestan OR Restoril OR “Ro 5 5345” OR Ro55345 OR “SaH 47 603” OR “SaH 47,603” OR Temaze OR “Temazep von CT” OR Thioridazine OR ApoThioridazine OR Meleril OR Melleril OR Melleryl OR Mellaril OR Melleretten OR Melzine OR Thiozine OR Sonapax OR Thioridazineneurazpharm OR Aldazine OR Rideril OR Thiothixene OR Tiotixene OR Navane OR Topiramate OR USL255 OR “McN 4853” OR Topamax OR Epitomax OR Tranylcypromine OR “Trans 2 Phenylcyclopropylamine” OR Jatrosom OR Transamine OR Parnate OR Trazodone OR Tradozone OR “AF 1161” OR AF1161 OR Deprax OR Desyrel OR Molipaxin OR Trittico OR Thombran OR “Trazodon Hexal” OR “Trazodon Neuraxpharm” OR Trazon OR Triazolam OR “U 33,030” OR “U33,030” OR Halcion OR Trilam OR “Apo Triazo” OR Trifluoperazine OR Trifluoroperazine OR Trifluperazine OR Eskazine OR Flupazine OR Terfluzine OR Triftazin OR Stelazine OR Trimipramine OR Trimeprimine OR Herphonal OR Trimineurin OR NovoTripramine OR Rhotrimine OR Stangyl OR Surmontil OR Trimidura OR Trimineurin OR Trimipramin OR “Apo Trimip” OR ApoTrimip OR Eldoral OR Venlafaxine OR “Wy 45,030” OR Wy45030 OR “Wy 45,030” OR “Wy45,030” OR Effexor OR Trevilor OR Vandral OR Efexor OR Dobupal OR Vigabatrin OR “Gamma Vinyl GABA” OR “Gamma Vinyl Gamma Aminobutyric Acid” OR Sabril OR Sabrilex OR Vortioxetine OR Brintellix OR “Lu AA21004” OR LuAA21004 OR Zaleplon OR “SKP 1041” OR Sonata OR Zelepion OR Starnoc OR “CL 284,846” OR “CL284,846” OR “CL 284846” OR “L 846” OR Ziprasidone OR Ziprazidone OR “CP 88,059” OR “CP 88059” OR Zolpidem OR Amsic OR Bikalm OR Dalparan OR “SL 80.0750” OR “SL 800750 23 N” OR Stilnoct OR Stilnox OR Zodormdura OR Zoldem OR Zolirin OR “Zolpi Lich” OR Zolpinox OR Zolpimist OR Ambien OR Zopiclone OR Zop OR Zopicalma OR Zopiclodura OR Zopiclon OR Zopitan OR Zorclone OR Imovane OR Ximovan OR Zimovane OR Limovan OR Optidorm OR Rhovane OR “RP 27 267” OR Siaten OR Somnosan OR Zileze OR Zimoclone OR “Zopi Puren” OR Zopicalm OR Zotepine OR Zoleptil OR Nipolept OR Zuclopenthixol OR Zuclopentixol OR Clopixol OR Zuclopenthixole OR Acuphase).ti,ab.
-
3.
(1 AND 2) NOT (Animals NOT (Humans NOT Animals)).sh.
Limit 3 to English.
Rights and permissions
About this article
Cite this article
Hicks, A.J., Clay, F.J., Ponsford, J.L. et al. Pharmacotherapy for the Pseudobulbar Affect in Individuals Who Have Sustained a Traumatic Brain Injury: a Systematic Review. Neuropsychol Rev 30, 28–50 (2020). https://doi.org/10.1007/s11065-020-09427-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11065-020-09427-7