ABSTRACT
Purpose
To understand the relationship between the risk of opioid-related gastrointestinal adverse effects (AEs) and exposure to tapentadol and oxycodone as well as its active metabolite, oxymorphone, using pharmacokinetic/pharmacodynamic models.
Methods
The analysis was based on a study in patients with moderate-to-severe pain following bunionectomy. Population PK modeling was conducted to estimate population PK parameters for tapentadol, oxycodone, and oxymorphone. Time to AEs was analyzed using Cox proportional-hazards models.
Results
Risk of nausea, vomiting, and constipation significantly increased with exposure to tapentadol or oxycodone/oxymorphone. However, elevated risk per drug exposure of AEs for tapentadol was ~3–4 times lower than that of oxycodone, while elevated AE risk per drug exposure of oxycodone was ~60 times lower than that for oxymorphone, consistent with reported in vitro receptor binding affinities for these compounds. Simulations show that AE incidence following administration of tapentadol IR is lower than that following oxycodone IR intake within the investigated range of analgesic noninferiority dose ratios.
Conclusions
This PK/PD analysis supports the clinical findings of reduced nausea, vomiting and constipation reported by patients treated with tapentadol, compared to patients treated with oxycodone.



Similar content being viewed by others
REFERENCES
Bhamb B, Brown D, Hariharan J, Anderson J, Balousek S, Fleming MF. Survey of select practice behaviors by primary care physicians on the use of opioids for chronic pain. Curr Med Res Opin. 2006;22(9):1859–65.
Arnold R. Why patients do not take their opioids. J Palliat Med. 2004;7(5):716–7.
Morley-Forster PK, Clark AJ, Speechley M, Moulin DE. Attitudes toward opioid use for chronic pain: a Canadian physician survey. Pain Res Manag. 2003;8(4):189–94.
Oderda GM, Said Q, Evans RS, Stoddard GJ, Lloyd J, Jackson K, et al. Opioid-related adverse drug events in surgical hospitalizations: impact on costs and length of stay. Ann Pharmacother. 2007;41(3):400–6.
Oderda GM, Evans RS, Lloyd J, Lipman A, Chen C, Ashburn M, et al. Cost of opioid-related adverse drug events in surgical patients. J Pain Symptom Manage. 2003;25(3):276–83.
Furlan AD, Sandoval JA, Mailis-Gagnon A, Tunks E. Opioids for chronic noncancer pain: a meta-analysis of effectiveness and side effects. Cmaj. 2006;174(11):1589–94.
Strassels SA, McNicol E, Suleman R. Postoperative pain management: a practical review, part 2. Am J Health Syst Pharm. 2005;62(19):2019–25.
Gregorian RS, Jr., Gasik A, Kwong WJ, Voeller S, Kavanagh S. Importance of side effects in opioid treatment: a trade-off analysis with patients and physicians. J Pain Nov;11(11):1095–108.
Riley J, Eisenberg E, Muller-Schwefe G, Drewes AM, Arendt-Nielsen L. Oxycodone: a review of its use in the management of pain. Curr Med Res Opin. 2008;24(1):175–92.
Poyhia R, Vainio A, Kalso E. A review of oxycodone’s clinical pharmacokinetics and pharmacodynamics. J Pain Symptom Manage. 1993;8(2):63–7.
Smith HS. Clinical pharmacology of oxymorphone. Pain Med. 2009;10(S1):S3–S10.
Volpe DA, McMahon Tobin GA, Mellon RD, Katki AG, Parker RJ, Colatsky T, et al. Uniform assessment and ranking of opioid Mu receptor binding constants for selected opioid drugs. Regul Toxicol Pharmacol Apr;59(3):385–90.
Lalovic B, Kharasch E, Hoffer C, Risler L, Liu-Chen LY, Shen DD. Pharmacokinetics and pharmacodynamics of oral oxycodone in healthy human subjects: role of circulating active metabolites. Clin Pharmacol Ther. 2006;79(5):461–79.
Tzschentke TM, Christoph T, Kogel B, Schiene K, Hennies H-H, Englberger W, et al. (−)-(1R,2R)-3-(3-dimethylamino-1-ethyl-2-methyl-propyl)-phenol hydrochloride (tapentadol HCl): a novel mu-opioid receptor agonist/norepinephrine reuptake inhibitor with broad-spectrum analgesic properties. J Pharmacol Exp Ther. 2007;323(1):323.
Nucynta TM Product Label. Available From: http://www.accessdata.fda.gov/drugsatfda_docs/label/2010/022304s003lbl.pdf. [Accessed 2011 July 6].
Stegmann JU, Weber H, Steup A, Okamoto A, Upmalis D, Daniels S. The efficacy and tolerability of multiple-dose tapentadol immediate release for the relief of acute pain following orthopedic (bunionectomy) surgery. Curr Med Res Opin. 2008;24(11):3185–96.
Hartrick CT. Tapentadol immediate release for the relief of moderate-to-severe acute pain. Expert Opin Pharmacother. 2009;10(16):2687–96.
Hartrick C, Van Hove I, Stegmann JU, Oh C, Upmalis D. Efficacy and tolerability of tapentadol immediate release and oxycodone HCl immediate release in patients awaiting primary joint replacement surgery for end-stage joint disease: a 10-day, phase III, randomized, double-blind, active- and placebo-controlled study. Clin Ther. 2009;31(2):260–71.
Daniels SE, Upmalis D, Okamoto A, Lange C, Haeussler J. A randomized, double-blind, phase III study comparing multiple doses of tapentadol IR, oxycodone IR, and placebo for postoperative (bunionectomy) pain. Curr Med Res Opin. 2009;25(3):765–76.
Daniels S, Casson E, Stegmann JU, Oh C, Okamoto A, Rauschkolb C, et al. A randomized, double-blind, placebo-controlled phase 3 study of the relative efficacy and tolerability of tapentadol IR and oxycodone IR for acute pain. Curr Med Res Opin. 2009;25(6):1551–61.
Xu XS, Smit JW, Lin R, Stuyckens K, Terlinden R, Nandy P. Population pharmacokinetics of tapentadol immediate release (IR) in healthy subjects and patients with moderate or severe pain. Clin Pharmacokinet. 2010;49(10):671–82.
Mandema JW, Kaiko RF, Oshlack B, Reder RF, Stanski DR. Characterization and validation of a pharmacokinetic model for controlled-release oxycodone. Br J Clin Pharmacol. 1996;42(6):747–56.
Boeckman A, Sheiner LB, Beal SL. NONMEM VI. Ellicott City: GloboMax, Icon Development Solutions; 2007.
Beal SL, Sheiner LB. NONMEM Users Guides. Ellicott City, MD, USA: GloboMax, Icon Development Solutions; 1989–1998.
R Development Core Team. R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2008.
Cox DR. Regression models and life tables (with discussion). J R Stat Soc Ser B. 1972;34:187–220.
Hooker AC, Staatz CE, Karlsson MO. Conditional weighted residuals (CWRES): a model diagnostic for the FOCE method. Pharm Res. 2007;24(12):2187–97.
Bergstrand M, Hooker AC, Wallin JE, Karlsson MO. Prediction-corrected visual predictive checks for diagnosing nonlinear mixed-effects models. Aaps J Jun;13(2):143–51.
Prommer E. Oxymorphone: a review. Support Care Cancer. 2006;14(2):109–15.
Sinclair DR, Chung F, Mezei G. Can postoperative nausea and vomiting be predicted? Anesthesiology. 1999;91(1):109–18.
Cepeda MS, Farrar JT, Baumgarten M, Boston R, Carr DB, Strom BL. Side effects of opioids during short-term administration: effect of age, gender, and race. Clin Pharmacol Ther. 2003;74(2):102–12.
Liukas A, Kuusniemi K, Aantaa R, Virolainen P, Neuvonen M, Neuvonen PJ, et al. Elimination of intravenous oxycodone in the elderly: a pharmacokinetic study in postoperative orthopaedic patients of different age groups. Drugs Aging. 2011;28(1):41–50.
Grambsch P, Therneau T. Proportional hazards tests and diagnostics based on weighted residuals. Biometrika. 1994;81:515–26.
Matthes HW, Maldonado R, Simonin F, Valverde O, Slowe S, Kitchen I, et al. Loss of morphine-induced analgesia, reward effect and withdrawal symptoms in mice lacking the mu-opioid-receptor gene. Nature. 1996;383(6603):819–23.
Kieffer BL. Opioids: first lessons from knockout mice. Trends Pharmacol Sci. 1999;20(1):19–26.
Roberts GW, Bekker TB, Carlsen HH, Moffatt CH, Slattery PJ, McClure AF. Postoperative nausea and vomiting are strongly influenced by postoperative opioid use in a dose-related manner. Anesth Analg. 2005;101(5):1343–8.
Chen ZR, Irvine RJ, Somogyi AA, Bochner F. Mu receptor binding of some commonly used opioids and their metabolites. Life Sci. 1991;48(22):2165–71.
Heiskanen T, Olkkola KT, Kalso E. Effects of blocking CYP2D6 on the pharmacokinetics and pharmacodynamics of oxycodone. Clin Pharmacol Ther. 1998;64(6):603–11.
Shaheen PE, Walsh D, Lasheen W, Davis MP, Lagman RL. Opioid equianalgesic tables: are they all equally dangerous? J Pain Symptom Manage. 2009;38(3):409–17.
Hanks GW, Forbes K. Opioid responsiveness. Acta Anaesthesiol Scand. 1997;41(1 Pt 2):154–8.
ACKNOWLEDGMENTS AND DISCLOSURES
All authors are employees of Janssen Research and Development. The analyses and studies described in this report were funded by Janssen Research and Development. Steven Xu is an adjunct assistant professor in the School of Public Health at the University of Medicine and Dentistry of New Jersey.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
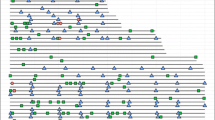
Supplementary Figure 1A
Diagnostic Plots for the Final Joint PK Model for Oxycodone (A) and Oxymorphone (B). The dashed line represents a LOWESS smoother. In the residual plots, the ordinate value of zero is presented (solid horizontal line). In the plots of observed vs. population and individual predictions, the solid line represents the line of identity. (PPT 525 kb)
Supplementary Figure 1B
Diagnostic Plots for the Final Joint PK Model for Oxycodone (A) and Oxymorphone (B). The dashed line represents a LOWESS smoother. In the residual plots, the ordinate value of zero is presented (solid horizontal line). In the plots of observed vs. population and individual predictions, the solid line represents the line of identity. (PPT 442 kb)
Supplementary Figure 2
Distribution of estimated steady-state AUC for tapentadol (50, 75, and 100 mg), oxycodone, and oxymorphone. (PPT 124 kb)
Supplementary Figure 3
Comparison of predicted event-free probability based on the PK/PD models to the observed event-free probability over time (Kaplan-Meier [KM] curves according to tapentadol dose groups). The solid lines represent the observed KM curves; the shaded areas represent the 95% confidence intervals of model prediction, which were constructed using the uncertainty (standard error) for the model parameters. (PPT 151 kb)
Rights and permissions
About this article
Cite this article
Xu, X.S., Etropolski, M., Upmalis, D. et al. Pharmacokinetic and Pharmacodynamic Modeling of Opioid-Induced Gastrointestinal Side Effects in Patients Receiving Tapentadol IR and Oxycodone IR. Pharm Res 29, 2555–2564 (2012). https://doi.org/10.1007/s11095-012-0786-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-012-0786-5