Abstract
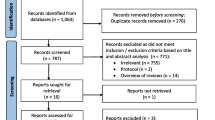
Background Duloxetine is currently approved for chronic pain management; however, despite some evidence, its utility in acute, postoperative pain remains unclear Aim of the review This systematic review and meta-analysis is to determine if duloxetine 60 mg given perioperatively, is safe and effective at reducing postoperative opioid consumption and reported pain following elective orthopedic surgery. Method CINAHL, Medline, Cochrane Central Registry for Clinical Trials, Google Scholar, and Clinicaltrials.gov were searched using a predetermined search strategy from inception to January 15, 2019. Covidence.org was used to screen, select, and extract data by two independent reviewers. Individual study bias was assessed using the Cochrane Risk of Bias tool. Opioid consumption data were converted to oral morphine milligram equivalents (MME) and exported to RevMan where meta-analysis was conducted using a DerSimonian and Laird random effects model. Results Six randomized-controlled trials were included in the literature review of postoperative pain and adverse effects. Five studies were utilized for the meta-analysis of postoperative opioid consumption; totaling 314 patients. Postoperative pain analysis showed variable statistical significance with overall lower pain scores with duloxetine. Adverse effects included an increase in insomnia with duloxetine but lower rates of nausea and vomiting. Meta-analysis revealed statistically significant [mean difference (95% CI)] lower total opioid use with duloxetine postoperatively at 24 h [− 31.9 MME (− 54.22 to − 9.6), p = 0.005], 48 h [− 30.90 MME (− 59.66 to − 2.15), p = 0.04] and overall [− 31.68 MME (− 46.62 to − 16.74), p < 0.0001]. Conclusion These results suggest that adding perioperative administration duloxetine 60 mg to a multimodal analgesia regimen within the orthopedic surgery setting significantly lowers total postoperative opioid consumption and reduces pain without significant adverse effects.


Similar content being viewed by others
References
Rosen JE. Postoperative care. In: Doherty GM, editor. CURRENT Diagnosis & Treatment: Surgery, 14e. McGraw-Hill Education: New York, NY; 2015.
Gerbershagen HJ, Aduckathil S, van Wijck AJ, Peelen LM, Kalkman CJ, Meissner W. Pain intensity on the first day after surgery: a prospective cohort study comparing 179 surgical procedures. Anesthesiology. 2013;118(4):934–44.
Martin BI, Mirza SK, Spina N, Spiker WR, Lawrence B, Brodke DS. Trends in lumbar fusion procedure rates and associated hospital costs for degenerative spinal diseases in the United States, 2004 to 2015. Spine. 2019;44(5):369–76.
Fingar KR, Stocks C, Weiss A, Steiner CA. Most Frequent Operating Room Procedures Performed in U.S. Hospitals, HCUP statistical Brief #186. Agency for Healthcare Research and Quality. 2003–2012.
Koepke EJ, Manning EL, Miller TE, Ganesh A, Williams DGA, Manning MW. The rising tide of opioid use and abuse: the role of the anesthesiologist. Perioper Med (Lond). 2018;7(16):16.
Menendez ME, Ring D, Bateman BT. Preoperative opioid misuse is associated with increased morbidity and mortality after elective Orthopaedic Surgery. ClinOrthopRelat Res. 2015;473(7):2402–12.
Kalakoti P, Hendrickson NR, Bedard NA, Pugely AJ. Opioid utilization following lumbar arthrodesis: trends and factors associated with long-term use. Spine. 2018;43(17):1208–16.
Pugely AJ, Bedard NA, Kalakoti P, Hendrickson NR, Shillingford JN, Laratta JL, et al. Opioid use following cervical spine surgery: trends and factors associated with long-term use. Spine J. 2018;18(11):1974–81.
Mudumbai SC, Lewis ET, Oliva EM, Chung PD, Harris B, Trafton J, et al. Overdose risk associated with opioid use upon hospital discharge in veterans health administration surgical patients. Pain Med. 2019;20(5):1020–31.
Drew JM, Demos HA, Pellegrini JVD. Management of common perioperative complications in orthopedic surgery. In: McKean SC, Ross JJ, Dressler DD, Scheurer DB, editors. Principles and Practice of Hospital Medicine, 2e. McGraw-Hill Education: New York, NY; 2017.
Baldini G, Miller T. Enhanced recovery protocols & optimization of perioperative outcomes. In: Butterworth Iv JF, Mackey DC, Wasnick JD, editors. Morgan & Mikhail’s Clinical Anesthesiology, 6e. McGraw-Hill Education: New York, NY; 2018.
Castro-Alves LJ, Oliveira de Medeiros AC, Neves SP, Carneiro de Albuquerque CL, Modolo NS, De Azevedo VL, et al. Perioperative duloxetine to improve postoperative recovery after abdominal hysterectomy a prospective randomized double-blinded placebo-controlled study. AnesthAnalg. 2016;122(1):98–104.
Nasr D. Efficacy of perioperative duloxetine on acute and chronic postmastectomy pain. Ain-Shams J Anaesthesiol. 2014;7(2):129–33.
Zorrilla-Vaca A, Stone A, Caballero-Lozada AF, Paredes S, Grant MC. Perioperative duloxetine for acute postoperative analgesia: a meta-analysis of randomized trials. RegAnesthesia Pain Med. 2019;44(10):959–65.
Cochrane M. Cochrane Bias - Cochrane Risk of Bias Tool. https://methods.cochrane.org/risk-bias-2. Accessed 19 Nov 2020.
Moher D, Liberati A, Tetzlaff J, Altman DG, Grope P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J ClinEpidemiol. 2009;62(10):1006–12.
YaDeau JT, Brummett CM, Mayman DJ, Lin Y, Goytizolo EA, Padgett DE, et al. Duloxetine and Subacute pain after knee arthroplasty when added to a multimodal analgesic regimen: a randomized, placebo-controlled. Triple-Blinded Trial Anesthesiol. 2016;125(3):561–72.
Saoud A, Elkabarity R. Effect of perioperative duloxetine on postoperative pain relief following anterior cervical microdiscectomy and fusion a pilot study. World Spin Column J. 2013;4(2):57–66.
Covidence lets you create and maintain Systematic Reviews online. 2019. https://www.covidence.org/reviews/active. Accessed 19 Nov 2020.
Centers for Disease Control and P. Analyzing Prescription Data and Morphine Milligram Equivalents (MME). 2018. https://www.cdc.gov/drugoverdose/resources/data.html. Accessed 19 Nov 2020.
University of North Carolina School of M. Opiate Equianalgesic Dosing Chart. 2009. https://www.med.unc.edu/aging/files/2018/06/Analgesic-Equivalent-Chart.pdf. Accessed 19 Nov 2020.
Altiparmak B, Guzel C, Gumus DS. Comparison of preoperative administration of pregabalin and duloxetine on cognitive functions and pain management after spinal surgery: a randomized, double-blind. Placebo-controlled Study Clin J Pain. 2018;34(12):1114–20.
Attia JZ, Mansour HS. Perioperative duloxetine and etoricoxibto improve postoperative pain after lumbar laminectomy: a randomized, double-blind, controlled study. BMC Anesthesiol. 2017;17(1):162.
Ho KY, Tay W, Yeo MC, Liu H, Yeo SJ, Chia SL, et al. Duloxetine reduces morphine requirements after knee replacement surgery. Br J Anaesth. 2010;105(3):371–6.
Bedin A, CaldartBedin RA, Vieira JE, Ashmawi HA. Duloxetine as an analgesic reduces opioid consumption after spine surgery: a randomized, double-blind. Controlled Study Clin J Pain. 2017;33(10):865–9.
Centre for Evidence-Based M. Oxford Centre for Evidence-based Medicine - Levels of Evidence (March 2009). CEBM. 2009. https://www.cebm.net/wp-content/uploads/2014/06/CEBM-Levels-of-Evidence-2.1.pdf Accessed 19 Nov 2020.
Shah A, Hayes CJ, Martin BC. Characteristics of Initial prescription episodes and likelihood of long-term opioid use-United States, 2006–2015. MMWR Morb Mortal Wkly Rep. 2017;66(10):265–9.
Stephan BC, Parsa FD. Avoiding opioids and their harmful side effects in the postoperative patient: exogenous opioids, endogenous endorphins, wellness, mood, and their relation to postoperative pain. Hawaii J Med Pub Health. 2016;75(3):63–7.
Wandner LD, Scipio CD, Hirsh AT, Torres CA, Robinson ME. The perception of pain in others: how gender, race, and age influence pain expectations. J Pain. 2012;13(3):220–7.
Skljarevski V, Desaiah D, Liu-Seifert H, Zhang Q, Chappell AS, Detke MJ, et al. Efficacy and safety of duloxetine in patients with chronic low back pain. Spine. 2010;35(13):E578–85.
Eli L. Cymbalta Prescribing Information. http://uspl.lilly.com/cymbalta/cymbalta.html. Accessed 19 Nov 2020.
Park SH, Wackernah RC, Stimmel GL. Serotonin syndrome: is it a reason to avoid the use of tramadol with antidepressants? J Pharm Pract. 2014;27(1):71–8.
Singh I, Achuthan S, Chakrabarti A, Rajagopalan S, Srinivasan A, Hota D. Influence of pre-operative use of serotonergic antidepressants (SADs) on the risk of bleeding in patients undergoing different surgical interventions: a meta-analysis. Pharmacoepidemiol Drug Saf. 2015;24(3):237–45.
Yaksh T, Wallace M. Opioids, Analgesia, and Pain Management. In: Brunton LL, Hilal-Dandan R, Knollmann BC, editors. Goodman & Gilman’s: The Pharmacological Basis of Therapeutics, 13e. McGraw-Hill Education: New York, NY; 2017.
Kim SH, Yoon KB, Yoon DM, Yoo JH, Ahn KR. Influence of centrally mediated symptoms on postoperative pain in osteoarthritis patients undergoing total knee arthroplasty: a prospective observational evaluation. Pain Pract. 2015;15(6):E46-53.
Koh IJ, Kim MS, Sohn S, Song KY, Choi NY, In Y. Duloxetine reduces pain and improves quality of recovery following total knee arthroplasty in centrally sensitized patients: a prospective, randomized controlled study. J Bone Joint Surg Am. 2019;101(1):64–73.
Govil N, Parag K, Arora P, Khandelwal H, Singh A . Perioperative duloxetine as part of a multimodal analgesia regime reduces postoperative pain in lumbar canal stenosis surgery: a randomized, triple blind, and placebo-controlled trial. Korean J Pain. 2020;33(1):40–7.
de Boer HD, Detriche O, Forget P. Opioid-related side effects: Postoperative ileus, urinary retention, nausea and vomiting, and shivering. A review of the literature. Best Pract Res ClinAnaesthesiol. 2017;31(4):499–504.
Acknowledgements
We thank Jaques YaDeau (Department of Anesthesiology, Hospital for Special Surgeries, New York, USA) for providing us the complete dataset of their study published in Anesthesiology [17].
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors have declared that no conflicts of interest exist.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Branton, M.W., Hopkins, T.J. & Nemec, E.C. Duloxetine for the reduction of opioid use in elective orthopedic surgery: a systematic review and meta-analysis. Int J Clin Pharm 43, 394–403 (2021). https://doi.org/10.1007/s11096-020-01216-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-020-01216-9