Abstract
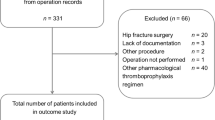
Hallux valgus surgery (HVS) is one of the most common orthopedic procedures, often occurring in older adults. Guidelines provide inconsistent recommendations about venous thromboembolism (VTE) prophylaxis after HVS and data are scarce regarding VTE presentation and outcomes in this population. We reported the clinical characteristics and outcomes of VTE following HVS among patients enrolled in Registro Informatizado Enfermedad TromboEmbolica (RIETE), a prospective multicenter VTE registry. We compared the findings with those of other patients in RIETE. Consecutive patients with VTE post HVS were included in the study. Baseline characteristics, administration of VTE prophylaxis prior to diagnosis, presenting symptoms and signs, risk factors for VTE, and 90-day outcomes including recurrent VTE, major bleeding and death were determined. A total of 54 patients with VTE post HVS were identified in RIETE [median age: 64 (interquartile range 56–71) years; 85.2% female] and were compared with 74,111 VTE patients who had not undergone HVS. Among those with VTE post HVS, 63.0% had received VTE prophylaxis, in contrast to 35.6% in the rest of the RIETE cohort. Simplified Pulmonary Embolism Severity Index was zero in 66.7% of the patients with pulmonary embolism post HVS and 33.3% of other RIETE patients (P = 0.011). Compared with other VTE patients, use of estrogens was higher in HVS group (13.0% vs 5.4%, P = 0.01). All patients with VTE post HVS (100%) and most of other VTE patients (99.6%) were treated with anticoagulation, most commonly with low-molecular weight heparins. In contrast to the rest of the patients in RIETE, the absolute number of all fatal and non-fatal outcomes at 90 days was zero in the post HVS group (i.e. no deaths, no recurrence of VTE, and no major bleeding). In a large registry of patients with VTE, all patients with VTE post HVS underwent anticoagulation. These patients had much better outcomes than the rest of VTE patients, with no deaths, recurrences or major bleeding events at 90-day follow-up.

Similar content being viewed by others
References
Gilheany MF, Landorf KB, Robinson P (2008) Hallux valgus and hallux rigidus: a comparison of impact on health-related quality of life in patients presenting to foot surgeons in Australia. J Foot Ankle Res 1:14
Mann RA, Coughlin MJ (1993) Adult hallux valgus. In: Mann RA Coughlin MJ (eds) Surgery of the foot and ankle, 6th edn. Mosby, St. Louis, pp 167–296
Harrison WD, Walker CR (2016) Controversies and trends in United Kingdom Bunion Surgery. Foot Ankle Clin 21:207–217
Menz HB, Lord SR (2001) Foot pain impairs balance and functional ability in community-dwelling older people. J Am Podiatri Med Assoc 91:222–229
Nix S, Smith M, Vicenzino B (2010) Prevalence of hallux valgus in the general population: a systematic review and meta-analysis. J Foot Ankle Res 3:21
Torkki M, Malmivaara A, Seitsalo S, Hoikka V, Laippala P, Paavolainen P (2001) Surgery vs orthosis vs watchful waiting for hallux valgus: a randomized controlled trial. JAMA 285:2474–2480
Belatti DA, Phisitkul P (2014) Economic burden of foot and ankle surgery in the US Medicare population. Foot Ankle Int 35:334–340
MedicareAustralia (2018) Medicare Item Reports. https://medicarestatistics.humanservices.gov.au/statistics/do.jsp?_PROGRAM=%2Fstatistics%2Fmbs_item_standard_report&DRILL=ag&group=49821%2C49824%2C49827%2C49830%2C49833%2C49836%2C49837%2C49838%2C49839%2C49842%2C47933&VAR=services&STAT=count&RPT_FMT=by+state&PTYPE=finyear&START_DT=201707&END_DT=201806. 2017–2018
Jameson SS, Augustine A, James P, Serrano-Pedraza I, Oliver K, Townshend D, Reed MR (2011) Venous thromboembolic events following foot and ankle surgery in the English National Health Service. J Bone Jt Surg Br 93:490–497
Radl R, Kastner N, Aigner C, Portugaller H, Schreyer H, Windhager R (2003) Venous thrombosis after hallux valgus surgery. J Bone Jt Surg Am 85a:1204–1208
Ferrao P, Saragas N, Saragas E, Jacobson B (2014) Venous thromboembolic disease in hallux surgery. Orthop Proc 96:35–35
Bikdeli B, Bikdeli B, Visvanathan R (2018) Use of prophylaxis for prevention of venous thromboembolism in patients with isolated foot or ankle surgery: a systematic review and meta-analysis. Aust J Ageing 37:24–25
Bikdeli B, Jimenez D, Hawkins M, Ortiz S, Prandoni P, Brenner B, Decousus H, Masoudi FA, Trujillo-Santos J, Krumholz HM, Monreal M, Investigators R (2018) Rationale design and methodology of the computerized registry of patients with venous thromboembolism (RIETE). Thromb Haemost 118:214–224
Saro C (2007) Hallux valgus surgery: epidemiological aspects and clinical outcome. Institutionen för klinisk vetenskap/Department of Clinical Sciences, Stockholm
Wang T-F, Wong CA, Milligan PE, Thoelke MS, Woeltje KF, Gage BF (2014) Risk factors for inpatient venous thromboembolism despite thromboprophylaxis. Thromb Res 133:25–29
Northup A, Wilcox S (2017) Thromboprophylaxis failure in the adult medical inpatient. Am J Med Sci 354:107–116
Lim W, Meade M, Lauzier F, Zarychanski R, Mehta S, Lamontagne F, Dodek P, McIntyre L, Hall R, Heels-Ansdell D, Fowler R, Pai M, Guyatt G, Crowther MA, Warkentin TE, Devereaux PJ, Walter SD, Muscedere J, Herridge M, Turgeon AF, Geerts W, Finfer S, Jacka M, Berwanger O, Ostermann M, Qushmaq I, Friedrich JO, Cook DJ (2015) Failure of anticoagulant thromboprophylaxis: risk factors in medical-surgical critically ill patients. Crit Care Med 43:401–410
Graham WC, Flanigan DC (2014) Venous thromboembolism following arthroscopic knee surgery: a current concepts review of incidence, prophylaxis, and preoperative risk assessment. Sports Med 44:331–343
Egermayer P (1999) Mortality of untreated deep vein thrombosis following knee arthroscopy. Chest 115:604
Kelly J, Rudd A, Lewis R, Hunt B (2001) Screening for subclinical deep-vein thrombosis. QJM 94:511–519
Robert-Ebadi H, Righini M (2010) Anticoagulation in the elderly. Pharmaceuticals 3:3543–3569
Gage BF, Yan Y, Milligan PE, Waterman AD, Culverhouse R, Rich MW, Radford MJ (2006) Clinical classification schemes for predicting hemorrhage: results from the National Registry of Atrial Fibrillation (NRAF). Am Heart J 151:713–719
Ruiz-Gimenez N, Suarez C, Gonzalez R, Nieto JA, Todoli JA, Samperiz AL, Monreal M (2008) Predictive variables for major bleeding events in patients presenting with documented acute venous thromboembolism—findings from the RIETE Registry. Thromb Haemost 100:26–31
Acknowledgements
We express our gratitude to Sanofi Spain for supporting this Registry with an unrestricted educational grant. We also express our gratitude to Bayer Pharma AG for supporting this Registry. Bayer Pharma AG’s support was limited to the part of RIETE outside Spain, which accounts for a 25.28% of the total patients included in the RIETE Registry. We also thank the RIETE Registry Coordinating Center, S&H Medical Science Service, for their quality control data, logistic and administrative support and Prof.
Funding
RIETE registry is supported by research grants from Sanofi Spain and Bayer Pharma AG. The funders have no access to the database nor had any role in the design of the current study. They did not have access to the prepared manuscript, and did not have a role in the decision to submit the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Behnood Bikdeli was supported by the National Heart, Lung, and. Blood Institute, National Institutes of Health, through Grant Number T32 HL007854. The content is the responsibility of the authors and does not necessarily represent the views of the NIH. Dr. Bikdeli reports that he has been a consulting expert (on behalf of the plaintiff) for litigation related to a specific type of IVC filters. Dr Ido Weinberg is on the scientific advisory board for Novate Medical and a non-compensated advisor for BTG. The current study is the idea of the investigators and has not been prepared at the request of a third party. Other authors have no conflict of interest to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
Coordinator of the RIETE Registry: Manuel Monreal.
RIETE Steering Committee Members: Paolo Prandoni, Benjamin Brenner and Dominique Farge-Bancel.
RIETE National Coordinators: Raquel Barba (Spain), Pierpaolo Di Micco (Italy), Laurent Bertoletti (France), Sebastian Schellong (Germany), Inna Tzoran (Israel), Abilio Reis (Portugal), Marijan Bosevski (R. Macedonia), Henri Bounameaux (Switzerland), Radovan Malý (Czech Republic), Peter Verhamme (Belgium), Joseph A. Caprini (USA), Hanh My Bui (Vietnam).
RIETE Registry Coordinating Center: S & H Medical Science Service. Members of the RIETE Group.
SPAIN: Adarraga MD, Agud M, Aibar MA, Amado C, Arcelus JI, Ballaz A, Barba R, Barbagelata C, Barrón M, Barrón-Andrés B, Blanco-Molina A, Camon AM, Cañas I, Carrasco C, Castro J, de Ancos C, del Toro J, Demelo P, Díaz-Pedroche C, Díaz-Peromingo JA, Encabo M, Falgá C, Farfán AI, Fernández de Roitegui K, Fernández-Capitán C, Fernández-Criado MC, Fidalgo MA, Flores K, Font C, Font L, Furest I, Galián JD, García MA, García-Bragado F, García-Morillo M, García-Raso A, Gavín O, Gayol MC, Gil-Díaz A, Gómez V, Gómez-Cuervo C, González-Martínez J, Grau E, Gutiérrez J, Hernández-Blasco LM, Hermosa-Los Arcos MJ, Iglesias M, Jara-Palomares L, Jaras MJ, Jiménez D, Jiménez R, Joya MD, Jou I, Lima J, Llamas P, Lobo JL, López-Jiménez L, López-Miguel P, López-Núñez JJ, López-Reyes R, López-Sáez JB, Lorente MA, Lorenzo A, Loring M, Lumbierres M, Madridano O, Maestre A, Marchena PJ, Martín del Pozo M, Martínez-García MA, Mella C, Mellado M, Monreal M, Morales MV, Nieto ML, Nieto JA, Núñez MJ, Olivares MC, Otalora S, Otero R, Panadero-Macía M, Pedrajas JM, Pellejero G, Pérez-Ductor C, Pérez-Jacoiste A, Pérez-Rus G, Peris ML, Porras JA, Rivas A, Rodríguez-Cobo A, Rodríguez-Hernández A, Rubio CM, Ruiz-Ruiz J, Ruiz-Sada P, Sahuquillo JC, Sala-Sainz MC, Salazar V, Salgueiro G, Sampériz A, Sánchez-Muñoz-Torrero JF, Sancho T, Soler S, Suriñach JM, Tolosa C, Torres MI, Uresandi F, Valle R, Vela JR, Vidal G, Villares P, ARGENTINA: Gutiérrez P, Vázquez FJ, Vilaseca A, BELGIUM: Vanassche T, Vandenbriele C, Verhamme P, BRAZIL: Yoo HHB, CZECH REPUBLIC: Hirmerova J, Malý R, ECUADOR: Salgado E, FRANCE: Benzidia I, Bertoletti L, Bura-Riviere A, Debourdeau P, Farge-Bancel D, Helfer H, Hij A, Mahé I, Moustafa F, GERMANY: Schellong S, ISRAEL: Braester A, Brenner B, Tzoran I, IRAN: Sharif-Kashani B, ITALY: Barillari G, Bilora F, Bortoluzzi C, Brandolin B, Ciammaichella M, Dentali F, Di Micco P, Folath M, Imbalzano E, Landolfi R, Maida R, Mastroiacovo D, Pace F, Pallotti G, Pesavento R, Prandoni P, Quintavalla R, Rocci A, Siniscalchi C, Tufano A, Visonà A, Zalunardo B, LATVIA: Gibietis V, Kigitovica D, Skride A, REPUBLIC OF MACEDONIA: Bosevski M, SWITZERLAND: Bounameaux H, Mazzolai L, USA: Bikdeli B, Caprini J, VIETNAM: Bui HM. Salvador Ortiz, Universidad Autónoma Madrid and Silvia Galindo, both Statistical Advisors in S&H Medical Science Service for the statistical analysis of the data presented in this paper.
Rights and permissions
About this article
Cite this article
Bikdeli, B., Visvanathan, R., Weinberg, I. et al. Clinical characteristics and outcomes of venous thromboembolic events after hallux valgus surgery: insights from the RIETE registry. J Thromb Thrombolysis 49, 651–658 (2020). https://doi.org/10.1007/s11239-019-02025-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11239-019-02025-2