Abstract
The ATP-gated P2X7 ion channel has emerging roles in amyotrophic lateral sclerosis (ALS) progression. Pharmacological blockade of P2X7 with Brilliant Blue G can ameliorate disease in SOD1G93A mice, but recent data suggests that this antagonist displays poor penetration of the central nervous system (CNS). Therefore, the current study aimed to determine whether the CNS-penetrant P2X7 antagonist, JNJ-47965567, could ameliorate ALS progression in SOD1G93A mice. A flow cytometric assay revealed that JNJ-47965567 impaired ATP-induced cation dye uptake in a concentration-dependent manner in murine J774 macrophages. Female and male SOD1G93A mice were injected intraperitoneally with JNJ-47965567 (30 mg/kg) or 2-(hydroxypropyl)-beta-cyclodextrin (vehicle control) three times a week from disease onset until end stage, when tissues were collected and studied. JNJ-47965567 did not impact weight loss, clinical score, motor (rotarod) coordination or survival compared to control mice. NanoString analysis revealed altered spinal cord gene expression in JNJ-47965567 mice compared to control mice, but such differences were not confirmed by quantitative PCR. Flow cytometric analyses revealed no differences between treatments in the frequencies or activation status of T cell or dendritic cell subsets in lymphoid tissues or in the concentrations of serum cytokines. Notably, serum IL-27, IFNβ and IL-10 were present in relatively high concentrations compared to other cytokines in both groups. In conclusion, JNJ-47965567 administered thrice weekly from disease onset did not alter disease progression or molecular and cellular parameters in SOD1G93A mice.




Similar content being viewed by others
References
Talbott EO, Malek AM, Lacomis D (2016) The epidemiology of amyotrophic lateral sclerosis. Handb Clin Neurol 138:225–238. https://doi.org/10.1016/b978-0-12-802973-2.00013-6
Brown RH, Al-Chalabi A (2017) Amyotrophic lateral sclerosis. N Engl J Med 377:162–172. https://doi.org/10.1056/NEJMra1603471
Jaiswal MK (2019) Riluzole and edaravone: a tale of two amyotrophic lateral sclerosis drugs. Med Res Rev 39:733–748. https://doi.org/10.1002/med.21528
Rosen DR, Siddique T, Patterson D, Figlewicz DA, Sapp P, Hentati A, Donaldson D, Goto J, O'Regan JP, Deng HX et al (1993) Mutations in Cu/Zn superoxide dismutase gene are associated with familial amyotrophic lateral sclerosis. Nature 362:59–62. https://doi.org/10.1038/362059a0
Gurney M, Pu HF, Chiu AY, Dal Canto M, Polchow CY, Alexander DD, Caliendo J, Hentati A, Kwon YW, Deng H-X, Chen W, Zhai P, Sufit RL, Siddique T (1994) Motor neuron degeneration in mice that express a human Cu,Zn superoxide dismutase mutation. Science 264:1772–1775. https://doi.org/10.1126/science.8209258
Tan RH, Ke YD, Ittner LM, Halliday GM (2017) ALS/FTLD: experimental models and reality. Acta Neuropathol 133:177–196. https://doi.org/10.1007/s00401-016-1666-6
Pfohl SR, Halicek MT, Mitchell CS (2015) Characterization of the contribution of genetic background and gender to disease progression in the SOD1 G93A mouse model of amyotrophic lateral sclerosis: a meta-analysis. J Neuromuscul Dis 2:137–150. https://doi.org/10.3233/jnd-140068
McGoldrick P, Joyce PI, Fisher EM, Greensmith L (2013) Rodent models of amyotrophic lateral sclerosis. Biochim Biophys Acta 1832:1421–1436. https://doi.org/10.1016/j.bbadis.2013.03.012
Sluyter R (2017) The P2X7 receptor. Adv Exp Med Biol 1051:17–53. https://doi.org/10.1007/5584_2017_59
Di Virgilio F, Dal Ben D, Sarti AC, Giuliani AL, Falzoni S (2017) The P2X7 receptor in infection and inflammation. Immunity 47:15–31. https://doi.org/10.1016/j.immuni.2017.06.020
Jimenez-Mateos EM, Smith J, Nicke A, Engel T (2018) Regulation of P2X7 receptor expression and function in the brain. Brain Res Bull 151:153–163. https://doi.org/10.1016/j.brainresbull.2018.12.008
Bhattacharya A, Wang Q, Ao H, Shoblock JR, Lord B, Aluisio L, Fraser I, Nepomuceno D, Neff RA, Welty N, Lovenberg TW, Bonaventure P, Wickenden AD, Letavic MA (2013) Pharmacological characterization of a novel centrally permeable P2X7 receptor antagonist: JNJ-47965567. Br J Pharmacol 170:624–640. https://doi.org/10.1111/bph.12314
Fischer W, Franke H, Krugel U, Muller H, Dinkel K, Lord B, Letavic MA, Henshall DC, Engel T (2016) Critical evaluation of P2X7 receptor antagonists in selected seizure models. PLoS One 11:e0156468. https://doi.org/10.1371/journal.pone.0156468
Jimenez-Pacheco A, Diaz-Hernandez M, Arribas-Blazquez M, Sanz-Rodriguez A, Olivos-Ore LA, Artalejo AR, Alves M, Letavic M, Miras-Portugal MT, Conroy RM, Delanty N, Farrell MA, O'Brien DF, Bhattacharya A, Engel T, Henshall DC (2016) Transient P2X7 receptor antagonism produces lasting reductions in spontaneous seizures and gliosis in experimental temporal lobe epilepsy. J Neurosci 36:5920–5932. https://doi.org/10.1523/jneurosci.4009-15.2016
Karasawa A, Kawate T (2016) Structural basis for subtype-specific inhibition of the P2X7 receptor. Elife 5. https://doi.org/10.7554/eLife.22153
Yiangou Y, Facer P, Durrenberger P, Chessell IP, Naylor A, Bountra C, Banati RR, Anand P (2006) COX-2, CB2 and P2X7-immunoreactivities are increased in activated microglial cells/macrophages of multiple sclerosis and amyotrophic lateral sclerosis spinal cord. BMC Neurol 6:12. https://doi.org/10.1186/1471-2377-6-12
Casanovas A, Hernandez S, Tarabal O, Rossello J, Esquerda JE (2008) Strong P2X4 purinergic receptor-like immunoreactivity is selectively associated with degenerating neurons in transgenic rodent models of amyotrophic lateral sclerosis. J Comp Neurol 506:75–92. https://doi.org/10.1002/cne.21527
D'Ambrosi N, Finocchi P, Apolloni S, Cozzolino M, Ferri A, Padovano V, Pietrini G, Carri MT, Volonte C (2009) The proinflammatory action of microglial P2 receptors is enhanced in SOD1 models for amyotrophic lateral sclerosis. J Immunol 183:4648–4656. https://doi.org/10.4049/jimmunol.0901212
Gandelman M, Peluffo H, Beckman JS, Cassina P, Barbeito L (2010) Extracellular ATP and the P2X7 receptor in astrocyte-mediated motor neuron death: implications for amyotrophic lateral sclerosis. J Neuroinflammation 7:33. https://doi.org/10.1186/1742-2094-7-33
Gandelman M, Levy M, Cassina P, Barbeito L, Beckman JS (2013) P2X7 receptor-induced death of motor neurons by a peroxynitrite/FAS-dependent pathway. J Neurochem 126:382–388. https://doi.org/10.1111/jnc.12286
Cieslak M, Roszek K, Wujak M (2019) Purinergic implication in amyotrophic lateral sclerosis-from pathological mechanisms to therapeutic perspectives. Purinergic Signal 15:1–15. https://doi.org/10.1007/s11302-018-9633-4
Volonte C, Apolloni S, Parisi C, Amadio S (2016) Purinergic contribution to amyotrophic lateral sclerosis. Neuropharmacology 104:180–193. https://doi.org/10.1016/j.neuropharm.2015.10.026
Cervetto C, Frattaroli D, Maura G, Marcoli M (2013) Motor neuron dysfunction in a mouse model of ALS: gender-dependent effect of P2X7 antagonism. Toxicology 311:69–77
Apolloni S, Amadio S, Parisi C, Matteucci A, Potenza RL, Armida M, Popoli P, D'Ambrosi N, Volonte C (2014) Spinal cord pathology is ameliorated by P2X7 antagonism in a SOD1-mutant mouse model of amyotrophic lateral sclerosis. Dis Model Mech 7:1101–1109. https://doi.org/10.1242/dmm.017038
Bartlett R, Sluyter V, Watson D, Sluyter R, Yerbury JJ (2017) P2X7 antagonism using brilliant blue G reduces body weight loss and prolongs survival in female SOD1G93A amyotrophic lateral sclerosis mice. PeerJ 5:e3064. https://doi.org/10.7717/peerj.3064
Sluyter R, Bartlett R, Ly D, Yerbury JJ (2017) P2X7 receptor antagonism in amyotrophic lateral sclerosis. Neural Regen Res 12:749–750. https://doi.org/10.4103/1673-5374.206643
Bhattacharya A, Biber K (2016) The microglial ATP-gated ion channel P2X7 as a CNS drug target. Glia 64:1772–1787. https://doi.org/10.1002/glia.23001
Sluyter R, Vine KL (2016) N-alkyl-substituted Isatins enhance P2X7 receptor-induced interleukin-1beta release from murine macrophages. Mediat Inflamm 2016:2097219. https://doi.org/10.1155/2016/2097219
McLeod VM, Lau CL, Chiam MDF, Rupasinghe TW, Roessner U, Djouma E, Boon WC, Turner BJ (2019) Androgen receptor antagonism accelerates disease onset in the SOD1(G93A) mouse model of amyotrophic lateral sclerosis. Br J Pharmacol 176:2111–2130. https://doi.org/10.1111/bph.14657
Scott S, Kranz JE, Cole J, Lincecum JM, Thompson K, Kelly N, Bostrom A, Theodoss J, Al-Nakhala BM, Vieira FG, Ramasubbu J, Heywood JA (2008) Design, power, and interpretation of studies in the standard murine model of ALS. Amyotroph Lateral Scler 9:4–15. https://doi.org/10.1080/17482960701856300
Ludolph AC, Bendotti C, Blaugrund E, Chio A, Greensmith L, Loeffler JP, Mead R, Niessen HG, Petri S, Pradat PF, Robberecht W, Ruegg M, Schwalenstocker B, Stiller D, van den Berg L, Vieira F, von Horsten S (2010) Guidelines for preclinical animal research in ALS/MND: a consensus meeting. Amyotroph Lateral Scler 11:38–45. https://doi.org/10.3109/17482960903545334
Hatzipetros T, Kidd JD, Moreno AJ, Thompson K, Gill A, Vieira FG (2015) A quick phenotypic neurological scoring system for evaluating disease progression in the SOD1-G93A mouse model of ALS. J Vis Exp. https://doi.org/10.3791/53257
Geraghty NJ, Mansfield KJ, Fuller SJ, Watson D, Sluyter R (2017) The P2X7 receptor is not essential for development of imiquimod-induced psoriasis-like inflammation in mice. Purinergic Signal 13:405–415. https://doi.org/10.1007/s11302-017-9569-0
Butovsky O, Jedrychowski MP, Moore CS, Cialic R, Lanser AJ, Gabriely G, Koeglsperger T, Dake B, Wu PM, Doykan CE, Fanek Z, Liu L, Chen Z, Rothstein JD, Ransohoff RM, Gygi SP, Antel JP, Weiner HL (2014) Identification of a unique TGF-beta-dependent molecular and functional signature in microglia. Nat Neurosci 17:131–143. https://doi.org/10.1038/nn.3599
Yoon H, Walters G, Paulsen AR, Scarisbrick IA (2017) Astrocyte heterogeneity across the brain and spinal cord occurs developmentally, in adulthood and in response to demyelination. PLoS One 12:e0180697. https://doi.org/10.1371/journal.pone.0180697
Gustafson MP, Staff NP, Bornschlegl S, Butler GW, Maas ML, Kazamel M, Zubair A, Gastineau DA, Windebank AJ, Dietz AB (2017) Comprehensive immune profiling reveals substantial immune system alterations in a subset of patients with amyotrophic lateral sclerosis. PLoS One 12:e0182002. https://doi.org/10.1371/journal.pone.0182002
Murdock BJ, Zhou T, Kashlan SR, Little RJ, Goutman SA, Feldman EL (2017) Correlation of peripheral immunity with rapid amyotrophic lateral sclerosis progression. JAMA Neurol 74:1446–1454. https://doi.org/10.1001/jamaneurol.2017.2255
Henkel JS, Beers DR, Wen S, Rivera AL, Toennis KM, Appel JE, Zhao W, Moore DH, Powell SZ, Appel SH (2013) Regulatory T-lymphocytes mediate amyotrophic lateral sclerosis progression and survival. EMBO Mol Med 5:64–79. https://doi.org/10.1002/emmm.201201544
Sheean RK, McKay FC, Cretney E, Bye CR, Perera ND, Tomas D, Weston RA, Scheller KJ, Djouma E, Menon P, Schibeci SD, Marmash N, Yerbury JJ, Nutt SL, Booth DR, Stewart GJ, Kiernan MC, Vucic S, Turner BJ (2018) Association of Regulatory T-cell expansion with progression of amyotrophic lateral sclerosis: a study of humans and a transgenic mouse model. JAMA Neurol 75:681–689. https://doi.org/10.1001/jamaneurol.2018.0035
Purvis HA, Anderson AE, Young DA, Isaacs JD, Hilkens CM (2014) A negative feedback loop mediated by STAT3 limits human Th17 responses. J Immunol 193:1142–1150. https://doi.org/10.4049/jimmunol.1302467
Merad M, Sathe P, Helft J, Miller J, Mortha A (2013) The dendritic cell lineage: ontogeny and function of dendritic cells and their subsets in the steady state and the inflamed setting. Annu Rev Immunol 31:563–604. https://doi.org/10.1146/annurev-immunol-020711-074950
Hu Y, Cao C, Qin XY, Yu Y, Yuan J, Zhao Y, Cheng Y (2017) Increased peripheral blood inflammatory cytokine levels in amyotrophic lateral sclerosis: a meta-analysis study. Sci Rep 7:9094. https://doi.org/10.1038/s41598-017-09097-1
Jeyachandran A, Mertens B, McKissick EA, Mitchell CS (2015) Type I Vs. type II cytokine levels as a function of SOD1 G93A mouse amyotrophic lateral sclerosis disease progression. Front Cell Neurosci 9:462. https://doi.org/10.3389/fncel.2015.00462
Fabbrizio P, Amadio S, Apolloni S, Volonte C (2017) P2X7 receptor activation modulates autophagy in SOD1-G93A mouse microglia. Front Cell Neurosci 11:249. https://doi.org/10.3389/fncel.2017.00249
Seyffert C, Schmalzing G, Markwardt F (2004) Dissecting individual current components of co-expressed human P2X1 and P2X7 receptors. Curr Top Med Chem 4:1719–1730
Bo X, Jiang LH, Wilson HL, Kim M, Burnstock G, Surprenant A, North RA (2003) Pharmacological and biophysical properties of the human P2X5 receptor. Mol Pharmacol 63:1407–1416. https://doi.org/10.1124/mol.63.6.1407
Jo S, Bean BP (2011) Inhibition of neuronal voltage-gated sodium channels by brilliant blue G. Mol Pharmacol 80:247–257. https://doi.org/10.1124/mol.110.070276
Qiu F, Dahl G (2009) A permeant regulating its permeation pore: inhibition of pannexin 1 channels by ATP. Am J Phys Cell Physiol 296:C250–C255. https://doi.org/10.1152/ajpcell.00433.2008
Iwamaru Y, Takenouchi T, Murayama Y, Okada H, Imamura M, Shimizu Y, Hashimoto M, Mohri S, Yokoyama T, Kitani H (2012) Anti-prion activity of brilliant blue G. PLoS One 7:e37896. https://doi.org/10.1371/journal.pone.0037896
Grad LI, Yerbury JJ, Turner BJ, Guest WC, Pokrishevsky E, O'Neill MA, Yanai A, Silverman JM, Zeineddine R, Corcoran L, Kumita JR, Luheshi LM, Yousefi M, Coleman BM, Hill AF, Plotkin SS, Mackenzie IR, Cashman NR (2014) Intercellular propagated misfolding of wild-type cu/Zn superoxide dismutase occurs via exosome-dependent and -independent mechanisms. Proc Natl Acad Sci U S A 111:3620–3625. https://doi.org/10.1073/pnas.1312245111
Kovanyi B, Csolle C, Calovi S, Hanuska A, Kato E, Koles L, Bhattacharya A, Haller J, Sperlagh B (2016) The role of P2X7 receptors in a rodent PCP-induced schizophrenia model. Sci Rep 6:36680. https://doi.org/10.1038/srep36680
Rodriguez-Alvarez N, Jimenez-Mateos EM, Engel T, Quinlan S, Reschke CR, Conroy RM, Bhattacharya A, Boylan GB, Henshall DC (2017) Effects of P2X7 receptor antagonists on hypoxia-induced neonatal seizures in mice. Neuropharmacology 116:351–363. https://doi.org/10.1016/j.neuropharm.2017.01.005
Horvath G, Otrokocsi L, Beko K, Baranyi M, Kittel A, Fritz-Ruenes PA, Sperlagh B (2019) P2X7 receptors drive poly(I:C) induced autism-like behavior in mice. J Neurosci 39:2542–2561. https://doi.org/10.1523/JNEUROSCI.1895-18.2019
Donnelly-Roberts DL, Namovic MT, Surber B, Vaidyanathan SX, Perez-Medrano A, Wang Y, Carroll WA, Jarvis MF (2009) [3H]A-804598 ([3H]2-cyano-1-[(1S)-1-phenylethyl]-3-quinolin-5-ylguanidine) is a novel, potent, and selective antagonist radioligand for P2X7 receptors. Neuropharmacology 56:223–229. https://doi.org/10.1016/j.neuropharm.2008.06.012
Apolloni S, Amadio S, Montilli C, Volonte C, D'Ambrosi N (2013) Ablation of P2X7 receptor exacerbates gliosis and motoneuron death in the SOD1-G93A mouse model of amyotrophic lateral sclerosis. Hum Mol Genet 22:4102–4116. https://doi.org/10.1093/hmg/ddt259
Gu BJ, Wiley JS (2018) P2X7 as a scavenger receptor for innate phagocytosis in the brain. Br J Pharmacol 175:4195–4208. https://doi.org/10.1111/bph.14470
Gu BJ, Saunders BM, Jursik C, Wiley JS (2010) The P2X7-nonmuscle myosin membrane complex regulates phagocytosis of nonopsonized particles and bacteria by a pathway attenuated by extracellular ATP. Blood 115:1621–1631. https://doi.org/10.1182/blood-2009-11-251744
Ou A, Gu BJ, Wiley JS (2018) The scavenger activity of the human P2X7 receptor differs from P2X7 pore function by insensitivity to antagonists, genetic variation and sodium concentration: relevance to inflammatory brain diseases. Biochim Biophys Acta Mol basis Dis 1864:1051–1059. https://doi.org/10.1016/j.bbadis.2018.01.012
Bin Dayel A, Evans RJ, Schmid R (2019) Mapping the site of action of human P2X7 receptor antagonists AZ11645373, brilliant blue G, KN-62, Calmidazolium, and ZINC58368839 to the Intersubunit allosteric pocket. Mol Pharmacol 96:355–363. https://doi.org/10.1124/mol.119.116715
Vecsernyes M, Fenyvesi F, Bacskay I, Deli MA, Szente L, Fenyvesi E (2014) Cyclodextrins, blood-brain barrier, and treatment of neurological diseases. Arch Med Res 45:711–729. https://doi.org/10.1016/j.arcmed.2014.11.020
Yao J, Ho D, Calingasan NY, Pipalia NH, Lin MT, Beal MF (2012) Neuroprotection by cyclodextrin in cell and mouse models of Alzheimer disease. J Exp Med 209:2501–2513. https://doi.org/10.1084/jem.20121239
Maulik M, Ghoshal B, Kim J, Wang Y, Yang J, Westaway D, Kar S (2012) Mutant human APP exacerbates pathology in a mouse model of NPC and its reversal by a beta-cyclodextrin. Hum Mol Genet 21:4857–4875. https://doi.org/10.1093/hmg/dds322
Gazzerro E, Baldassari S, Assereto S, Fruscione F, Pistorio A, Panicucci C, Volpi S, Perruzza L, Fiorillo C, Minetti C, Traggiai E, Grassi F, Bruno C (2015) Enhancement of muscle T regulatory cells and improvement of muscular dystrophic process in mdx mice by blockade of extracellular ATP/P2X Axis. Am J Pathol 185:3349–3360. https://doi.org/10.1016/j.ajpath.2015.08.010
Koo TY, Lee JG, Yan JJ, Jang JY, Ju KD, Han M, Oh KH, Ahn C, Yang J (2017) The P2X7 receptor antagonist, oxidized adenosine triphosphate, ameliorates renal ischemia-reperfusion injury by expansion of regulatory T cells. Kidney Int 92:415–431. https://doi.org/10.1016/j.kint.2017.01.031
Moreno-Martinez L, de la Torre M, Toivonen JM, Zaragoza P, Garcia-Redondo A, Calvo AC, Osta R (2019) Circulating cytokines could not be good prognostic biomarkers in a mouse model of amyotrophic lateral sclerosis. Front Immunol 10:801. https://doi.org/10.3389/fimmu.2019.00801
Acknowledgements
The authors kindly acknowledge Sarah Toole (University of Wollongong) for advice regarding adverse events in mice; Kara L. Vine (University of Wollongong) and Anindya Bhattacharya (Janssen Research and Development) for advice regarding drug formulation; and Sam R. Adhikary (University of Wollongong) for assistance with necropsy. The authors also kindly acknowledge the technical staff of the Illawarra Health and Medical Research Institute and the University of Wollongong Rodent Facility.
Funding
This study was supported by grants from the Motor Neurone Disease Research Institute of Australia (R.S.), from the Australian National Health and Medical Research Council (NHMRC) Career Development Fellowship (APP1084144) (J.J.Y) and from the NHMRC Project Grant (APP1104295) (B.J.T). D.L. was a recipient of an Illawarra Health and Medical Research Institute Careers Development Grant. P.C., N.G and R.A.S were recipients of Australian Government Research Training Program (AGRTP) Scholarships.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare they have no conflict of interest.
Ethical approval
All procedures performed in studies involving animals were in accordance with the ethical standards of the University of Wollongong at which the studies were conducted (Animal Ethics Committee protocols AE12/09 and AE16/18). This study does not contain any work with human participants performed by any of the authors.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Fig. S1
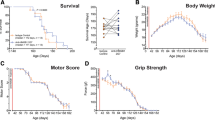
JNJ-47965567 does not alter clinical disease progression in female or male SOD1G93A mice. β-CD- and JNJ-47965567-treated SOD1G93A mice (Fig. 1) were stratified according to sex (female, left panels; male, right panels) to compare (A) ALS score, (B) body weight loss (percent of pre-disease maximum), (C) motor (rotarod) coordination and (D) survival. (A-D) Results are mean ± SEM (β-CD, n = 12 females or 11 males; JNJ-47965567, n = 12 females or 12 males) with differences between groups compared using (A-C) a two-way ANOVA or (D) the log-rank (Mantel-Cox) test. (PNG 36 kb)
Fig. S2
Gating strategies used to determine proportions of leukocyte subsets in SOD1G93A mice. (A) For analysis of T cell subsets, sequential flow cytometric gates were selected left to right as shown (top dot plots) and used to determine the proportion of total CD4+ and CD8+ T cells, as well as conventional CD4+ T cells (Foxp3−) and regulatory T cells (Foxp3+). The proportion of activated T cells (CD44+) in each T cell subset was then determined (bottom dot plots), with the relative CD39 expression on CD44+ T cell subsets also determined (histogram). (B) For analysis of DC subsets, single live cells were gated as for T cells (not shown) and then the proportion of conventional DCs (CD11c+MHC class IIlow cells) and migratory DCs (CD11c+MHC class IIhi cells) determined (left dot plot). The proportion of CD11b+ and CD11b− DCs amongst conventional and migratory DCs was then determined (middle dot plots). Finally, the relative CD80 expression on DC subsets was determined (histograms). (PNG 1937 kb)
Table S1
(DOC 32 kb)
Table S2
(XLSX 100 kb)
Rights and permissions
About this article
Cite this article
Ly, D., Dongol, A., Cuthbertson, P. et al. The P2X7 receptor antagonist JNJ-47965567 administered thrice weekly from disease onset does not alter progression of amyotrophic lateral sclerosis in SOD1G93A mice. Purinergic Signalling 16, 109–122 (2020). https://doi.org/10.1007/s11302-020-09692-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11302-020-09692-4