Abstract
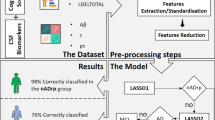
Machine learning methods have been applied to estimate measures of brain aging from neuroimages. However, only rarely have these measures been examined in the context of biologic age. Here, we investigated associations of an MRI-based measure of dementia risk, the Alzheimer’s disease pattern similarity (AD-PS) scores, with measures used to calculate biological age. Participants were those from visit 5 of the Atherosclerosis Risk in Communities Study with cognitive status adjudication, proteomic data, and AD-PS scores available. The AD-PS score estimation is based on previously reported machine learning methods. We evaluated associations of the AD-PS score with all-cause mortality. Sensitivity analyses using only cognitively normal (CN) individuals were performed treating CNS-related causes of death as competing risk. AD-PS score was examined in association with 32 proteins measured, using a Somalogic platform, previously reported to be associated with age. Finally, associations with a deficit accumulation index (DAI) based on a count of 38 health conditions were investigated. All analyses were adjusted for age, race, sex, education, smoking, hypertension, and diabetes. The AD-PS score was significantly associated with all-cause mortality and with levels of 9 of the 32 proteins. Growth/differentiation factor 15 (GDF-15) and pleiotrophin remained significant after accounting for multiple-testing and when restricting the analysis to CN participants. A linear regression model showed a significant association between DAI and AD-PS scores overall. While the AD-PS scores were created as a measure of dementia risk, our analyses suggest that they could also be capturing brain aging.



Similar content being viewed by others
References
Higgins-Chen AT, Thrush KL, Levine ME. Aging biomarkers and the brain. Semin Cell Dev Biol. 2021;116:180–93.
Casanova R, Hsu FC, Sink KM, Rapp SR, Williamson JD, Resnick SM, Espeland MA, Alzheimer’s Disease Neuroimaging I. Alzheimer’s disease risk assessment using large-scale machine learning methods. PLoS ONE. 2013;8: e77949.
Espeland MA, Chen JC, Weitlauf J, Hayden KM, Rapp SR, Resnick SM, Garcia L, Cannell B, Baker LD, Sachs BC, Tindle HA, Wallace R, Casanova R, Women’s Health Initiative Memory Study Magnetic Resonance Imaging Study G. Trajectories of relative performance with 2 measures of global cognitive function. J Am Geriatr Soc. 2018;66:1575–80.
Espeland MA, Luchsinger JA, Neiberg RH, Carmichael O, Laurienti PJ, Pi-Sunyer X, Wing RR, Cook D, Horton E, Casanova R, Erickson K, Nick Bryan R, Action for Health in Diabetes Brain Magnetic Resonance Imaging Research G. Long term effect of intensive lifestyle intervention on cerebral blood flow. J Am Geriatr Soc. 2018;66:120–6.
Younan D, Petkus AJ, Widaman KF, Wang X, Casanova R, Espeland MA, Gatz M, Henderson VW, Manson JE, Rapp SR, Sachs BC, Serre ML, Gaussoin SA, Barnard R, Saldana S, Vizuete W, Beavers DP, Salinas JA, Chui HC, Resnick SM, Shumaker SA, Chen JC. Particulate matter and episodic memory decline mediated by early neuroanatomic biomarkers of Alzheimer’s disease. Brain. 2020;143:289–302.
Younan D, Wang X, Casanova R, Barnard R, Gaussoin SA, Saldana S, Petkus AJ, Beavers DP, Resnick SM, Manson JE, Serre ML, Vizuete W, Henderson VW, Sachs BC, Salinas JA, Gatz M, Espeland MA, Chui HC, Shumaker SA, Rapp SR, Chen JC PM2.5 associated with gray matter atrophy reflecting increased Alzheimers risk in older women. Neurology. 2020.
Casanova R, Hsu FC, Barnard RT, Anderson AM, Talluri R, Whitlow CT, Hughes TM, Griswold M, Hayden KM, Gottesman RF, Wagenknecht LE. Comparing data-driven and hypothesis-driven MRI-based predictors of cognitive impairment in individuals from the Atherosclerosis Risk in Communities (ARIC) study. Alzheimers Dement. 2022;18:561–71.
Kennedy BK, Berger SL, Brunet A, Campisi J, Cuervo AM, Epel ES, Franceschi C, Lithgow GJ, Morimoto RI, Pessin JE, Rando TA, Richardson A, Schadt EE, Wyss-Coray T, Sierra F. Geroscience: linking aging to chronic disease. Cell. 2014;159:709–13.
Kohanski RA, Deeks SG, Gravekamp C, Halter JB, High K, Hurria A, Fuldner R, Green P, Huebner R, Macchiarini F, Sierra F. Reverse geroscience: how does exposure to early diseases accelerate the age-related decline in health? Ann N Y Acad Sci. 2016;1386:30–44.
Justice JN, Ferrucci L, Newman AB, Aroda VR, Bahnson JL, Divers J, Espeland MA, Marcovina S, Pollak MN, Kritchevsky SB, Barzilai N, Kuchel GA. A framework for selection of blood-based biomarkers for geroscience-guided clinical trials: report from the TAME Biomarkers Workgroup. Geroscience. 2018;40:419–36.
LeBrasseur NK, de Cabo R, Fielding R, Ferrucci L, Rodriguez-Manas L, Vina J, Vellas B. Identifying biomarkers for biological age: geroscience and the ICFSR task force. J Frailty Aging. 2021;10:196–201.
Hoffman JM, Hernandez CM, Hernandez AR, Bizon JL, Burke SN, Carter CS, Buford TW. Bridging the gap: a geroscience primer for neuroscientists with potential collaborative applications. J Gerontol A Biol Sci Med Sci. 2021.
Hernandez CM, Hernandez AR, Hoffman JM, King PH, McMahon LL, Buford TW, Carter C, Bizon JL, Burke SN. A neuroscience primer for integrating geroscience with the neurobiology of aging. J Gerontol A Biol Sci Med Sci. 2021.
Franke K, Gaser C. Ten years of BrainAGE as a neuroimaging biomarker of brain aging: what insights have we gained? Front Neurol. 2019;10:789 (PMID: 31474922).
Cole JH. Neuroimaging-derived brain-age: an ageing biomarker? Aging (Albany NY). 2017;9:1861–2.
Cole JH, Franke K. Predicting age using neuroimaging: innovative brain ageing biomarkers. Trends Neurosci. 2017;40:681–90 (PMID: 29074032).
Ning K, Zhao L, Matloff W, Sun F, Toga AW. Association of relative brain age with tobacco smoking, alcohol consumption, and genetic variants. Sci Rep. 2020;10:10 (PMID: 32001736).
Gaser C, Franke K, Kloppel S, Koutsouleris N, Sauer H. BrainAGE in mild cognitive impaired patients: predicting the conversion to Alzheimer’s disease. PLoS ONE. 2013;8: e67346.
Gaser C, Franke K, Kloppel S, Koutsouleris N, Sauer H, Alzheimer’s Disease Neuroimaging I. BrainAGE in mild cognitive impaired patients: predicting the conversion to Alzheimer’s disease. PLoS ONE. 2013;8: e67346 (PMID: 23826273).
Johnson AA, Shokhirev MN, Wyss-Coray T, Lehallier B. Systematic review and analysis of human proteomics aging studies unveils a novel proteomic aging clock and identifies key processes that change with age. Ageing Res Rev. 2020;60: 101070.
Mitnitski AB, Mogilner AJ, Rockwood K. Accumulation of deficits as a proxy measure of aging. ScientificWorldJournal. 2001;1:323–36 (PMID: 12806071).
Knopman DS, Gottesman RF, Sharrett AR, Wruck LM, Windham BG, Coker L, Schneider AL, Hengrui S, Alonso A, Coresh J, Albert MS, Mosley TH Jr. Mild cognitive impairment and dementia prevalence: the Atherosclerosis Risk in Communities Neurocognitive Study (ARIC-NCS). Alzheimers Dement (Amst). 2016;2:1–11.
Casanova R, Barnard RT, Gaussoin SA, Saldana S, Hayden KM, Manson JE, Wallace RB, Rapp SR, Resnick SM, Espeland MA, Chen JC, Group W-MS, the Alzheimer’s disease Neuroimaging I. Using high-dimensional machine learning methods to estimate an anatomical risk factor for Alzheimer’s disease across imaging databases. Neuroimage. 2018;183:401–11.
Walker KA, Chen J, Zhang J, Fornage M, Yang Y, Zhou L, Grams ME, Tin A, Daya N, Hoogeveen RC, Aozhou Wu, Sullivan KJ, Ganz P, Zeger SL, Gudmundsson EF, Emilsson V, Launer LJ, Jennings LL, Gudnason V, Chatterjee N, Gottesman RF, Mosley TH, Boerwinkle E, Ballantyne CM, Coresh J. Large-scale plasma proteomic analysis identifies proteins and pathways associated with dementia risk. Nature Aging. 2021;1:473–89.
Casanova R, Hsu FC, Espeland MA. Classification of structural MRI images in Alzheimer’s disease from the perspective of ill-posed problems. PLoS One. 2012;7: e44877 (PMID: 23071501).
Casanova R, Maldjian JA, Espeland MA. Evaluating the impact of different factors on voxel-wise classification methods of ADNI structural MRI brain images. International Journal of Biomedical Datamining. 2011;1:11.
Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94:496–509.
Franke K, Gaser C, Manor B, Novak V. Advanced BrainAGE in older adults with type 2 diabetes mellitus. Front Aging Neurosci. 2013;5:90.
Cole JH, Poudel RPK, Tsagkrasoulis D, Caan MWA, Steves C, Spector TD, Montana G. Predicting brain age with deep learning from raw imaging data results in a reliable and heritable biomarker. Neuroimage. 2017;163:115–24.
Cole JH, Ritchie SJ, Bastin ME, Valdes Hernandez MC, Munoz Maniega S, Royle N, Corley J, Pattie A, Harris SE, Zhang Q, Wray NR, Redmond P, Marioni RE, Starr JM, Cox SR, Wardlaw JM, Sharp DJ, Deary IJ. Brain age predicts mortality. Mol Psychiatry. 2018;23:1385–92 (PMID: 28439103).
Belsky DW, Caspi A, Houts R, Cohen HJ, Corcoran DL, Danese A, Harrington H, Israel S, Levine ME, Schaefer JD, Sugden K, Williams B, Yashin AI, Poulton R, Moffitt TE. Quantification of biological aging in young adults. Proc Natl Acad Sci U S A. 2015;112:E4104-4110.
Elliott ML, Caspi A, Houts RM, Ambler A, Broadbent JM, Hancox RJ, Harrington H, Hogan S, Keenan R, Knodt A, Leung JH, Melzer TR, Purdy SC, Ramrakha S, Richmond-Rakerd LS, Righarts A, Sugden K, Thomson WM, Thorne PR, Williams BS, Wilson G, Hariri AR, Poulton R, Moffitt TE. Disparities in the pace of biological aging among midlife adults of the same chronological age have implications for future frailty risk and policy. Nat Aging. 2021;1:295–308.
Elliott ML, Belsky DW, Knodt AR, Ireland D, Melzer TR, Poulton R, Ramrakha S, Caspi A, Moffitt TE, Hariri AR. Brain-age in midlife is associated with accelerated biological aging and cognitive decline in a longitudinal birth cohort. Mol Psychiatry. 2021;26:3829–38.
Habes M, Janowitz D, Erus G, Toledo JB, Resnick SM, Doshi J, Van der Auwera S, Wittfeld K, Hegenscheid K, Hosten N, Biffar R, Homuth G, Volzke H, Grabe HJ, Hoffmann W, Davatzikos C. Advanced brain aging: relationship with epidemiologic and genetic risk factors, and overlap with Alzheimer disease atrophy patterns. Transl Psychiatry. 2016;6: e775.
Kuller LH, Arnold AM, Longstreth WT Jr, Manolio TA, O’Leary DH, Burke GL, Fried LP, Newman AB. White matter grade and ventricular volume on brain MRI as markers of longevity in the cardiovascular health study. Neurobiol Aging. 2007;28:1307–15.
Henneman WJ, Sluimer JD, Cordonnier C, Baak MM, Scheltens P, Barkhof F, van der Flier WM. MRI biomarkers of vascular damage and atrophy predicting mortality in a memory clinic population. Stroke. 2009;40:492–8.
Doerstling S, Hedberg P, Ohrvik J, Leppert J, Henriksen E. Growth differentiation factor 15 in a community-based sample: age-dependent reference limits and prognostic impact. Ups J Med Sci. 2018;123:86–93.
Lim JH, Jeon Y, Ahn JS, Kim S, Kim DK, Lee JP, Ryu DR, Seong EY, Ahn SY, Baek SH, Jung HY, Choi JY, Park SH, Kim CD, Kim YL, Cho JH. GDF-15 predicts in-hospital mortality of critically ill patients with acute kidney injury requiring continuous renal replacement therapy: a multicenter prospective study. J Clin Med 10. 2021
Meyer SL, Wolff D, Ridderbos FS, Eshuis G, Hillege H, Willems TP, Ebels T, van Melle JP, Berger RMF. GDF-15 (growth differentiation factor 15) is associated with hospitalization and mortality in patients with a fontan circulation. J Am Heart Assoc. 2020;9: e015521.
Sathyan S, Ayers E, Gao T, Weiss EF, Milman S, Verghese J, Barzilai N. Plasma proteomic profile of age, health span, and all-cause mortality in older adults. Aging Cell. 2020;19: e13250.
Breniere C, Meloux A, Pedard M, Marie C, Thouant P, Vergely C, Bejot Y. Growth differentiation factor-15 (GDF-15) is associated with mortality in ischemic stroke patients treated with acute revascularization therapy. Front Neurol. 2019;10:611.
Chai YL, Hilal S, Chong JPC, Ng YX, Liew OW, Xu X, Ikram MK, Venketasubramanian N, Richards AM, Lai MKP, Chen CP. Growth differentiation factor-15 and white matter hyperintensities in cognitive impairment and dementia. Medicine (Baltimore). 2016;95: e4566.
He L, Barreto PS, Sanchez Sanchez JL, Rolland Y, Guyonnet S, Parini A, Lucas A, Vellas B, Group MD. Prospective associations of plasma growth differentiation factor 15 with physical performance and cognitive functions in older adults. J Gerontol A Biol Sci Med Sci. 2022.
Alcazar J, Frandsen U, Prokhorova T, Kamper RS, Haddock B, Aagaard P, Suetta C. Changes in systemic GDF15 across the adult lifespan and their impact on maximal muscle power: the Copenhagen Sarcopenia Study. J Cachexia Sarcopenia Muscle. 2021;12:1418–27.
Sarkar S, Melchior JT, Henry HR, Syed F, Mirmira RG, Nakayasu ES, Metz TO. GDF15: a potential therapeutic target for type 1 diabetes. Expert Opin Ther Targets. 2022;26:57–67.
Sanchis J, Ruiz V, Bonanad C, Sastre C, Ruescas A, Diaz M, Rodriguez E, Valero E, Garcia-Blas S, Carratala A, Nunez E, Nunez J. Growth differentiation factor 15 and geriatric conditions in acute coronary syndrome. Int J Cardiol. 2019;290:15–20.
Wischhusen J, Melero I, Fridman WH. Growth/differentiation factor-15 (GDF-15): from biomarker to novel targetable immune checkpoint. Front Immunol. 2020;11:951.
Gonzalez-Castillo C, Ortuno-Sahagun D, Guzman-Brambila C, Pallas M, Rojas-Mayorquin AE. Pleiotrophin as a central nervous system neuromodulator, evidences from the hippocampus. Front Cell Neurosci. 2014;8:443.
Lamprou M, Kaspiris A, Panagiotopoulos E, Giannoudis PV, Papadimitriou E. The role of pleiotrophin in bone repair. Injury. 2014;45:1816–23.
Fernandez-Calle R, Vicente-Rodriguez M, Gramage E, Pita J, Perez-Garcia C, Ferrer-Alcon M, Uribarri M, Ramos MP, Herradon G. Pleiotrophin regulates microglia-mediated neuroinflammation. J Neuroinflammation. 2017;14:46.
Toledo JB, Da X, Bhatt P, Wolk DA, Arnold SE, Shaw LM, Trojanowski JQ, Davatzikos C, Alzheimer’s Disease Neuroimaging I. Relationship between plasma analytes and SPARE-AD defined brain atrophy patterns in ADNI. PLoS ONE. 2013;8: e55531.
Nazeri A, Ganjgahi H, Roostaei T, Nichols T, Zarei M, Alzheimer’s Disease Neuroimaging I. Imaging proteomics for diagnosis, monitoring and prediction of Alzheimer’s disease. Neuroimage. 2014;102(Pt 2):657–65.
Kant IMJ, Mutsaerts H, van Montfort SJT, Jaarsma-Coes MG, Witkamp TD, Winterer G, Spies CD, Hendrikse J, Slooter AJC, de Bresser J. The association between frailty and MRI features of cerebral small vessel disease. Sci Rep. 2019;9:11343.
Siejka TP, Srikanth VK, Hubbard RE, Moran C, Beare R, Wood A, Phan T, Callisaya ML. Frailty and cerebral small vessel disease: a cross-sectional analysis of the Tasmanian Study of Cognition and Gait (TASCOG). J Gerontol A Biol Sci Med Sci. 2018;73:255–60.
Franke K, Gaser C. Longitudinal changes in individual BrainAGE in healthy aging, mild cognitive impairment, and Alzheimer’s disease. GeroPsych J Gerontopsychology Geriatr Psychiatry. 2012;25:235–45.
Acknowledgements
The Atherosclerosis Risk in Communities Study is carried out as a collaborative study supported by National Heart, Lung, and Blood Institute contracts (HHSN268201700001I, HHSN268201700002I, HHSN268201700003I, HHSN268201700005I, HHSN268201700004I). Neurocognitive data is collected by U01 2U01HL096812, 2U01HL096814, 2U01HL096899, 2U01HL096902, and 2U01HL096917 from the NIH (NHLBI, NINDS, NIA, and NIDCD), and with previous brain MRI examinations funded by R01-HL70825 from the NHLBI. The authors thank the staff and participants of the ARIC study for their important contributions. SomaLogic Inc. conducted the SomaScan assays in exchange for use of ARIC data. This work was supported in part by NIH/NHLBI grant R01 HL134320. RC and TH receive funding from the Wake Forest Alzheimer’s Disease Core Center (P30AG049638-01A1). We thank the ARIC Neurocognitive Study and the grant P30 AG021332 for funding to develop these analyses. RC and TH receive funding from the P30AG072947. Data collection and sharing for this project were also funded by the Alzheimer’s Disease Neuroimaging Initiative (ADNI) (National Institutes of Health Grant U01 AG024904) and DOD ADNI (Department of Defense award number W81XWH-12-2-0012). ADNI is funded by the National Institute on Aging, the National Institute of Biomedical Imaging and Bioengineering, and through generous contributions from the following: AbbVie, Alzheimer’s Association; Alzheimer’s Drug Discovery Foundation; Araclon Biotech; BioClinica, Inc.; Biogen; Bristol-Myers Squibb Company; CereSpir, Inc.; Cogstate; Eisai Inc.; Elan Pharmaceuticals, Inc.; Eli Lilly and Company; EuroImmun; F. Hoffmann-La Roche Ltd and its affiliated company Genentech, Inc.; Fujirebio; GE Healthcare; IXICO Ltd.; Janssen Alzheimer Immunotherapy Research & Development, LLC.; Johnson & Johnson Pharmaceutical Research & Development LLC.; Lumosity; Lundbeck; Merck & Co., Inc.; Meso Scale Diagnostics, LLC.; NeuroRx Research; Neurotrack Technologies; Novartis Pharmaceuticals Corporation; Pfizer Inc.; Piramal Imaging; Servier; Takeda Pharmaceutical Company; and Transition Therapeutics. The Canadian Institutes of Health Research is providing funds to support ADNI clinical sites in Canada. Private sector contributions are facilitated by the Foundation for the National Institutes of Health (www.fnih.org). The grantee organization is the Northern California Institute for Research and Education, and the study is coordinated by the Alzheimer’s Therapeutic Research Institute at the University of Southern California. ADNI data are disseminated by the Laboratory for Neuro Imaging at the University of Southern California.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Casanova, R., Anderson, A.M., Barnard, R.T. et al. Is an MRI-derived anatomical measure of dementia risk also a measure of brain aging?. GeroScience 45, 439–450 (2023). https://doi.org/10.1007/s11357-022-00650-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11357-022-00650-z