Abstract
Background
To close health disparities between Indigenous and non-Indigenous Australians, the Australian government in 2010 reduced medication copayments for Indigenous Australians living with, or at risk of, a chronic disease. Patients were registered for this incentive by their general practitioner.
Objective
To assess rates of hospitalizations for chronic conditions among Indigenous Australians before and after copayment reductions.
Design
Observational time-trend study of hospitalizations for chronic conditions sensitive to medication adherence..
Participants
Indigenous persons age 15 years and older in 16 urban, regional, and remote locations. The population ranged from 40,953 in 2009 to 42,651 in 2011.
Main Outcomes
Hospitalizations for diabetes, asthma, chronic obstructive pulmonary disease, hypertension, heart failure, and cardiovascular events.
Key Results
Approximately 22 % of Indigenous persons registered for the medication copayment incentive in the first 18 months of implementation. In areas with rates of incentive uptake exceeding 22 %, the age-standardized rate of hospitalizations for chronic conditions among Indigenous Australians declined from 103.4/1000 (95 % CI 88.8/1000 to 118.0/1000) in 2009 to 60.0/1000 (95 % CI 49.3/1000 to 70.7/1000) in 2011. In areas with below-average uptake of the incentive, we observed non-significant reductions in age-standardized hospitalization rates (from 63.3/1000 [95 % CI 52.9/1000 to 73.7/1000] in 2009 to 58.0/1000 [95 % CI 48.5/1000 to 67.5/1000] in 2011). Among Indigenous Australians, the rate of admission for acute conditions (pneumonia, influenza, urinary tract infection, pyelonephritis, and dehydration) was 38.4/1000 (95 % CI 32.4/1000 to 44.3/1000) in 2009 and 36.2/1000 (95 % CI 30.4/1000 to 41.8/1000) in 2011. Among the non-Indigenous population, we found substantially lower rates of hospitalizations and modest declines from 2009 to 2011.
Conclusions
Though we cannot make causal inferences from the results of this study, we observed marked declines in hospitalizations for chronic conditions among Indigenous Australians following targeted reductions in medication copayments for this population. These declines were largely limited to areas with higher uptake of the copayment incentive and were not observed for admissions related to acute conditions.
Similar content being viewed by others
INTRODUCTION
The disparity in health status between Indigenous and non-Indigenous Australians is substantial and well-documented.1 – 5 Indigenous Australians have a 13-year lower life expectancy, which is primarily driven by higher prevalence of chronic conditions such as cardiovascular disease and diabetes.3 – 6 The gap in life expectancy between Indigenous and non-Indigenous populations in Australia exceeds those reported in New Zealand, Canada, and the United States.4 Closing these disparities is a public health priority in Australia.
In 2008, the Council of Australian Governments announced a $1.6 billion initiative over 4 years, with the goal of closing the life expectancy gap between Indigenous and non-Indigenous Australians. As part of this effort, the Australian government in July 2010 implemented the Closing the Gap Pharmaceutical Benefit Scheme (PBS) copayment incentive as part of a suite of programs designed to improve chronic disease prevention and management among Indigenous patients (Table 1).7 The incentive reduced medication copayments for patients living with, or at risk of, a chronic disease, and applied to all prescriptions supplied under the PBS, an Australian governmental program that finances prescription medications to all Australian citizens and permanent residents.8 Eligible patients must also be at risk for “setbacks in the prevention or ongoing management of chronic disease if they did not take the prescribed medicine and … unlikely to adhere to their medicines regimen without assistance”, with this determination made by their treating general practitioner.8 Eligible patients were registered at private general practices participating in the Indigenous Health Incentive under the Practice Incentives Program (PIP) or Indigenous Health Services (IHS) that had applied for and been approved to participate in this program. (Table 1) Of note, since 1999, the Australian government has provided free medications for persons receiving care in remote Aboriginal and Torres Strait Islander Health Services, with evidence suggesting that this policy resulted in improved access to prescription drugs for Indigenous persons residing in remote areas.9
In 2010, copayments for PBS medicines were typically $33.30 per prescription for patients without financial assistance, and $5.40 per prescription for Australians who qualified for a means-tested government concession.8 The 2010 PBS copayment incentive reduced copayments to approximately $5.40 per prescription (the concessional copayment) for eligible Indigenous patients. Indigenous patients who already qualified for the concessional copayment level of $5.40 had their copayments waived entirely (i.e., free).
Reducing out-of-pocket costs for medications may promote their appropriate use and improve medication adherence for Indigenous populations with chronic disease.9 – 11 Further, evidence suggests that expanded insurance coverage for medications may be offset by reductions in hospitalizations for conditions that are amenable to medication therapy.12 The extent to which targeted reductions in drug copayments reduced hospitalizations for Indigenous Australians is not known.
In this study, we examined trends in hospitalizations for chronic conditions among Indigenous Australians in areas with higher and lower rates of uptakes of the PBS copayment incentive. We further assessed trends in hospitalizations among non-Indigenous persons, a control population that was not eligible for the incentive; and in hospitalizations for acute conditions that would be unrelated to increased use of chronic medication therapy.
METHODS
Study Design/Sources of Data
We draw on data from the Sentinel Sites Evaluation of the Indigenous Chronic Disease Package; methods are described in more detail elsewhere.13 The evaluation was a mixed-methods place-based study in 24 geographically bounded “sites” across urban, regional, and remote locations in Australia. Data include take-up rates of the PBS copayment incentive among the Indigenous population age 15 years and older. The Australian Department of Health selected each Sentinel Site in consultation with Aboriginal and Torres Strait Islander Health Partnership Forums in each state or territory. The following factors were considerations in the selection of Sentinel Sites: size of the Indigenous population, capacity of each partnership forum to participate in the evaluation, the level of need for improved access and care coordination, and early implementation of increased workforce goals. All Sentinel Sites are defined by a geographic boundary and selected to provide suitable reporting of population health data and use of services financed by Medicare, which is Australia’s publicly-funded national health insurance program. The geographical boundaries of the Sentinel Sites are based on Statistical Local Areas as defined by the Australian Bureau of Statistics (ABS).
To assess hospitalizations, we acquired admissions data from four states: New South Wales (NSW), Victoria (VIC), Queensland (QLD), and Western Australia (WA). These four states included 16 of the 24 Sentinel Sites and approximately 10 % of the Australian population age 15 and older (Table 2). The data included identifiers for each admission that indicated whether the patient was Indigenous or non-Indigenous. The main study population of Indigenous persons age 15 and older ranged from 40,953 in 2009 to 42,651 in 2011.
Outcome Variable
Our main outcome variables were hospitalizations and total hospital days for any of the following six conditions: diabetes, asthma, chronic obstructive pulmonary disease (COPD), hypertension, heart failure, and cardiovascular events (acute myocardial infarction, angina, stroke). Following the approach described by Afendulis et al., we selected these conditions since we considered them to be sensitive to chronic medication therapy.12 Further, the Australian government has designated diabetes, asthma, and cardiovascular conditions as National Health Priority Areas, since they are major contributors to the country’s burden of disease.13
Analyses
We conducted an observational time-trend study assessing rates of hospitalizations for chronic conditions among Indigenous and non-Indigenous Australians. We calculated the total number of admissions for these conditions by Sentinel Site and year, and for Indigenous and non-Indigenous patients. We derived the corresponding population denominator using ABS population projections from the 2006 Census for Indigenous and non-Indigenous persons age 15 and older in each Sentinel Site.14
For each Sentinel Site, we determined the rate of uptake of the PBS copayment incentive over the first 18 months of implementation (July 2010 to December 2011) among Indigenous persons age 15 and older (Table 1). The rate of uptake of the PBS copayment incentive was defined as the number of patients who received at least one subsidized prescription divided by the total number of Indigenous persons age 15 and older. We assessed rates of hospitalizations in 2009 (6–18 months before implementation, 2010 (the year of implementation), and 2011 (6–18 months after implementation). All rates were age-standardized based on the population distribution across all Sentinel Sites. We further conducted stratified analyses for the eight sites with higher than average uptake of the PBS copayment incentive (>22 % of all Indigenous persons registered) and eight sites with lower uptake (<22 % registered). We used the Fay-Feuer method to derive the confidence intervals for age-adjusted rates based on the gamma distribution.15 This method yields valid confidence intervals even when the numbers of events in some cells are small. We repeated the analyses for admissions for four acute conditions that we thought to be unrelated to chronic drug therapy: dehydration, urinary tract infection/pyelonephritis, pneumonia, and influenza. The study received ethical approval from the University of Melbourne, the Aboriginal Health & Medical Research Council of NSW, and the Commonwealth Government Department of Health Ethics Committee project number 10/2012.
RESULTS
The total number of the Indigenous population residing in the Sentinel Sites ranged from 764 (Bairnsdale, Vic; regional site) to 12,285 (Newcastle, NSW; urban site) (Table 2). The proportion of the total population identifying as Indigenous varied from 0.5 % (Dandenong, Vic; urban site) to 61.9 % (Derby, WA; remote site).
The rate of uptake of the PBS copayment incentive varied widely across Sentinel Sites, ranging from 1.5 % of the Indigenous population in Derby, WA, to 69 % of the Indigenous population in Logan/Woodridge, Qld. Uptake rates for the Sentinel Sites that we characterized as high and low uptake are shown in Table 2.
Hospitalizations for Chronic Conditions
Among Indigenous persons, the number of hospitalizations for chronic conditions during the study period totaled 4596. The most common reasons for admission were asthma/COPD (34 %), diabetes (31 %), and cardiovascular events (19 %). Among non-Indigenous persons, the number of hospitalizations for chronic conditions was 104,987, with asthma/COPD (29 %), cardiovascular events (26 %), and diabetes (22 %) as the most common conditions for admission.
Among Indigenous persons, the age-standardized rate of hospitalizations for chronic conditions per 1000 persons declined from 82.3 in 2009 (95 % CI 73.6–90.9) to 61.2 (95 % CI 54.0–68.4) in 2011. We observed a similar trend in the number of hospital days for chronic conditions per 1000 persons, which declined from 397.6 (95 % CI 378.7–416.5) in 2009 to 279.3 (95 % CI 263.7–295.0) in 2011.
Among the non-Indigenous population, the age-standardized rate of hospitalizations for chronic conditions per 1000 declined modestly from 21.7 (95 % CI 21.2–22.2) in 2009 to 18.9 (95 % CI 18.4–19.3) in 2011. The rate of hospital days for chronic conditions per 1000 also declined, from 216.8 (95 % CI 211.9–221.8) in 2009 to 180.4 (95 % CI 176.0–184.8) in 2011.
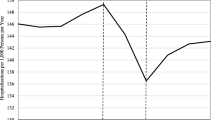
Trends in High-Uptake and Low-Uptake Regions
In areas with uptake of the incentive above the overall average of 22 %, the age-standardized rate of hospitalizations for chronic conditions among Indigenous Australians fell approximately 40 % from 103.4/1000 (95 % CI 88.8/1000 to 118.0/1000) in 2009 to 60.0/1000 (95 % CI 49.3/1000 to 70.7/1000) in 2011 (Fig. 1). Similarly, annual rates of hospital days for chronic conditions in high-uptake regions declined from 526.3/1000 [95 % CI 492.2/1000 to 560.4/1000] in 2009 to 285.4/1000 [95 % CI 262.3/1000 to 308.5/1000] in 2011 (Fig. 2).
In areas with below-average uptake of the incentive, age-standardized rates of hospitalizations for chronic conditions among Indigenous persons were unchanged (63.3/1000 [95 % CI 52.9/1000 to 73.7/1000] in 2009 to 58.0/1000 [95 % CI 48.5/1000 to 67.5/1000] in 2011). In low-uptake areas, annual rates of hospital days for chronic conditions were minimally changed between 2009 (271.3/1000 95 % CI 250.4/1000 to 292.6/1000) and 2011 (256.3/1000 95 % CI 235.8/1000 to 276.7/1000).
Acute Hospitalizations
We observed little change in the rate of hospitalizations for acute conditions (pneumonia, influenza, urinary tract infection, pyelonephritis, and dehydration). Among Indigenous Australians, the rate of admission was 38.4/1000 (95 % CI 32.4/1000 to 44.3/1000) in 2009 and 36.2/1000 (95 % CI 30.4/1000 to 41.8/1000) in 2011. The corresponding trend among non-Indigenous was 9.5/1000 (95 % CI 9.1/1000 to 9.8/1000) in 2009 and 9.8/1000 (95 % CI 9.5/1000 to 10.2/1000) in 2011.
In areas with higher uptake of the incentive, the rate of acute admissions among Indigenous persons was 44.4/1000 (95 % CI 35.2/1000 to 54.6/1000) in 2009 and 38.4/1000 (95 % CI 29.5/1000 to 47.3/1000) in 2011. In areas with lower uptake of the incentive, the rate of acute admissions among Indigenous persons was 34.4/1000 (95 % CI 27.6/1000 to 41.1/1000) in 2009 and 33.7/1000 (95 % CI 26.8/1000 to 40.6/1000) in 2011.
DISCUSSION
We evaluated hospitalizations before and after the implementation of the PBS copayment incentive which reduced or eliminated medication copayments for Indigenous Australians who were identified by their general practitioners as being at risk of or having a chronic disease. We have two main findings. First, we found substantial disparities in hospitalizations for chronic conditions amenable to medication therapy, with Indigenous Australians experiencing approximately three- to fourfold higher rates of admissions compared with those for non-Indigenous persons. Second, we report substantial declines in the rates of hospitalizations related to chronic conditions for Indigenous populations following the implementation of the PBS copayment incentive. These declines were observed in sites with higher uptake of the copayments, but only to a level consistent with hospitalization rates in low-uptake sites at baseline.
Our study was not designed to draw causal inferences between the implementation of the incentive and declines in hospitalizations. However, there are several features of our findings that suggest that the reductions in hospitalization rates may be related to the policy change. First, we observed reductions only in regions with higher than average uptake of the incentive, and found little change in the rates of hospitalizations for chronic conditions in areas with lower uptake of the incentive. Of note, the hospitalization rate before implementation of the incentive was substantially greater in the high-uptake regions, suggesting that there was perhaps a higher burden of illness or greater health needs in those regions. By 2011, the rates of hospitalization were equivalent between the high-uptake and low-uptake regions.
Second, we observe only modest changes in rates of hospitalizations for non-Indigenous Australians who were not eligible for the incentive. Third, we found no change in the rates of hospitalizations for acute conditions that would be unlikely to be related to chronic medication therapy. Finally, as reported in a prior Sentinel Sites Evaluation report, the four most commonly filled medications under the incentive were atorvastatin (lipid-lowering), metformin (glucose-lowering), perindopril (anti-hypertensive), and salbutamol (bronchodilator).16 These medicines correspond to the conditions we included in our study. Nevertheless, these findings are only suggestive. Our data and design do not allow us to draw firm conclusions about the relationship between the implementation of the PBS copayment incentive and lower hospitalization rates.
Other studies have found that increasing access and adherence to prescription medication may be associated with less use of hospital care.17 , 18 For instance, the implementation of a prescription drug benefit in a US Medicare program was associated with fewer hospitalizations for chronic conditions.12 The reductions in hospitalizations occurred within a year of implementation. Encinosa et al. found that increasing adherence to diabetes medications by 50 % was associated with a 23 % reduction in hospitalizations for persons with diabetes.19 The increased spending on diabetes medications due to increased adherence was more than offset by reduced spending on hospital care.
Alternatively, other factors that we could not assess in the study, including other components of the Indigenous Chronic Disease Package, could have accounted for the observed declines in the rate of admissions for chronic conditions. We expected a correlation between PBS uptake and primary care visits, because registration for the PBS copayment incentive was at primary care practices. The PBS copayment incentive may have acted synergistically to promote access to other health services offered as part of the Indigenous Chronic Disease Package, thereby resulting in improved medication adherence.7 For instance, Bailie et al. reported that the PBS copayment incentive might have increased visits to primary care practices, since patients knew that they could afford the medication that would be prescribed to them.7
Our study has three potential policy implications. First, reducing out-of-pocket costs for prescription medications and promoting access to primary care services may reduce disparities in outcomes among minority populations that have difficulty adhering to effective medication and a high burden of chronic disease. Second, the costs of lowering financial barriers to drug coverage may be offset by less hospital spending among this high-risk group of Indigenous Australians. Third, our finding of markedly elevated rates of hospitalizations for chronic conditions among Indigenous persons highlights the urgent need to improve chronic disease care for this population.
Our study has important limitations to consider. First, we cannot ascribe a causal relationship between the implementation of the PBS copayment incentive and declines in hospitalization rates. There could have been other features of high-uptake areas or the implementation of the Indigenous Chronic Disease Package that may have accounted for reductions in hospitalization rates. For instance, hospitalization rates in the high-uptake areas were greater than those in low-uptake areas in 2009, raising the possibility of increased prevalence of chronic disease or other risk factors for admission in those areas. Our data lack information on the health status of Indigenous persons in each site.
Second, we observed rates over a short period following implementation (18 months). Whether reductions persisted is unanswered. Third, our findings pertain to the Sentinel Sites and may not generalize to the rest of Australia. Fourth, rates of hospitalization may be impacted by variations in the diagnostic codes that hospitals use to submit claims to Medicare. Fifth, Indigenous patients may be undercounted in administrative data. Sixth, although hospitalizations for chronic conditions are thought to reflect the quality and accessibility of ambulatory care, few studies have directly assessed whether more effective outpatient care reduces inpatient admissions for ambulatory care-sensitive conditions.20 Finally, we were unable to determine which persons in our study were eligible for free medications through an earlier government program that targeted patients receiving care in remote Aboriginal clinics. However, just two of the sites in our study were located in remote areas.
In conclusion, we observed declines in rates of hospitalizations for chronic conditions following a targeted effort to reduce medication copayments for Indigenous Australians with chronic disease. These reductions were observed primarily in areas with greater uptake of the PBS copayment incentive and for chronic conditions amenable to drug therapy. Reducing out-of-pocket payments for prescription medications for minority populations may be an effective strategy for addressing ethnic disparities in chronic disease outcomes, though further study would be necessary to establish causality.
References
Australian Institute of Health and Welfare. The health and welfare of Australian’s Aboriginal and Torres Strait Islander peoples: Report No. IHW 147. Canberra: AIHW; 2015. Available at www.aihw.gov.au/publication-detail/?id=60129550168. Accessed October 15, 2016.
Hayman N, Reid PM, King M. Improving health outcomes for Indigenous peoples: what are the challenges? Cochrane Database Syst Rev. 2015;8:ED000104.
Hill K, Barker B, Vos T. Excess Indigenous mortality: are Indigenous Australians more severely disadvantaged than other Indigenous populations. Int J Epidemiol. 2007;36:580–589.
Bramley D, Hebert P, Jackson R, Chassin M. Indigenous disparities in disease-specific mortality, a cross-country comparison: New Zealand, Australia, Canada, and the United States. N Z Med J. 2004;117:U1215.
Vos T, Barker B, Begg S, Stanley L, Lopez AD. Burden of disease and injury in Aboriginal and Torres Strait Islander Peoples: the Indigenous health gap. Int J Epidemiol. 2009;38:470–477.
Zhao Y, Dempsey K. Causes of inequality in life expectancy between Indigenous and non-Indigenous people in the Northern Territory, 1981–2000: a decomposition analysis. Med J Aust. 2006;184:490–494.
Bailie J, Schierhout G, Laycock A, et al. Determinants of access to chronic illness care: a mixed-methods evaluation of a national multifaceted chronic disease package for Indigenous Australians. BMJ Open. 2015;5:e008103.
Australian Government. Department of Health Services. Closing the Gap-PBS Co-payment Measure. http://www.medicareaustralia.gov.au/provider/pbs/prescriber/closing-the-gap.jsp. Accessed October 15, 2016.
Kelaher M, Dunt D, Taylor-Thompson D, et al. Improving access to medicines among clients of remote area Aboriginal and Torres Strait Islander Health Services. Aust N Z J Public Health. 2006;30:177–183.
Couzos S, Sheedy V, Delaney Thiele D. Improving Aboriginal and Torres Strait Islander people’s access to medicines—the QUMAX program. Med J Aust. 2011;195:62–63.
Trivedi AN, Pollack AJ, Britt HC, Miller GC, Harrison C, Kelaher MA. General practitioners prescribing of lipid-lowering medications for Indigenous and non-Indigenous Australians, 2001–2013. Med J Aust. 2015;203(10):407–7.e5.
Afendulis CC, He Y, Zaslavsky AM, Chernew ME. The impact of Medicare Part D on hospitalization rates. Health Serv Res. 2011;46(4):1022–1028.
Bailie R, Griffin J, Kelaher M, et al. Sentinel sites evaluation: final report. Prepared for the Australian Government. Australian Institute of Health and Welfare. National Health Priority Areas. http://www.aihw.gov.au/national-health-priority-areas/. Accessed October 15, 2016.
Australian Bureau of Statistics. 2006 Census data. http://abs.gov.au/websitedbs/censushome.nsf/home/historicaldata2006. Accessed October 15, 2016.
Fay MP, Feuer EJ. Confidence intervals for directly standardized rates: a mthod based on the gamma distribution. Stat Med. 1997;16(7):791–801.
Australian Government Department of Health and Ageing. Canberra: Menzies School of Health Research, 2013. http://www.menzies.edu.au/icms_docs/189996_Sentinel_Sites_Evaluation_Final_Report.pdf. Accessed October 15, 2016.
McWilliams JM, Zaslavsky AM, Huskamp HA. Implementation of Medicare Part D and nondrug medical spending for elderly adults with limited prior drug coverage. JAMA. 2011;306(4):402–409.
Zhang Y, Donohue JM, Newhouse JP, Lave JR. The effect of Medicare Part D on drug and medical spending. N Engl J Med. 2009;361(1):52–61.
Encinosa WE, Bernard D, Dor A. Does prescription drug adherence reduce hospitalizations and costs? The case of diabetes. Adv Health Econ Health Serv Res. 2010;22:151–73.
Agency for Healthcare Research and Quality. Guide to Prevention Quality Indicators: Hospital Admission for Ambulatory Care Sensitive Conditions. http://www.ahrq.gov/downloads/pub/ahrqqi/pqiguide.pdf Accessed October 15, 2016.
Acknowledgments
This study was supported by the Commonwealth Fund and the Australian Department of Health. The Sentinel Sites Evaluation was conceived and funded by the Commonwealth Department of Health and Ageing. Successful conduct of the evaluation was made possible through the active support and commitment of key stakeholder organizations, community members, individuals who participated in the evaluation, and the contributions made by the broader evaluation team and the department staff. RB was supported by an ARC Future Fellowship (#FT100 100 087). AB is supported by a Charles and Sylvia Viertel Senior Medical Research Fellowship. ANT reports receiving consulting fees for editing the Merck Manual. This study was presented as an oral abstract at the Health Services Research Association of Australia and New Zealand’s Health Services and Policy Conference on December 8, 2015.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclaimers
The views expressed in this article are those of the authors and do not reflect the policy or position of the US government or the Department of Veterans Affairs.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Rights and permissions
About this article
Cite this article
Trivedi, A.N., Bailie, R., Bailie, J. et al. Hospitalizations for Chronic Conditions Among Indigenous Australians After Medication Copayment Reductions: the Closing the Gap Copayment Incentive. J GEN INTERN MED 32, 501–507 (2017). https://doi.org/10.1007/s11606-016-3912-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-016-3912-y