Abstract
Summary
Compliance and persistence with daily, weekly, and monthly bisphosphonates (BPs) for osteoporosis were assessed using data from the Platform for Clinical Information Statistical Analysis (CISA) database that contains data of prescriptions in 13 university hospitals in Japan. The analysis revealed compliance and persistence improved as the dosing interval increases.
Purpose
BPs are an effective first-line therapy for osteoporosis, but adherence is low. Compliance (medication possession ratio, MPR) and persistence (time to discontinuation) with daily, weekly, and monthly BPs were compared to ensure better adherence.
Methods
Using data from the CISA database containing prescription data in 13 university hospitals in Japan, adherence to oral BPs of osteoporotic patients was investigated. Daily and weekly BPs were compared for compliance and persistence over 5 and 8 years, and daily, weekly, and monthly BPs for those over 1 and 2 years.
Results
MPR over 5 years was 20.8 and 60.9 % for daily and weekly BPs (p < 0.001), respectively. MPR over 1 year was 38.6, 70.6, and 77.7 % for daily, weekly, and monthly BPs (P < 0.001), respectively. Persistence over 8 years was significantly higher in weekly than daily BPs (p < 0.001), and that over 5 years was highest in patients receiving BPs monthly (p < 0.01).
Conclusion
The present analysis indicates that a monthly regimen has better adherence to treatment as compared with weekly and daily regimens.
Similar content being viewed by others
Introduction
Bisphosphonates (BPs) are an effective first-line therapy for the treatment of osteoporosis, but adherence to therapy could be lower than other drugs for the treatment of chronic diseases with the exception of gout treatment and others [1, 2]. The poor adherence to BP therapy has been related to the complexity of required dosing procedures and the severity of possible adverse drug reactions. As poor adherence to BP therapy has been reported to increase the risk of osteoporotic fractures [3, 4], better adherence must be ensured to continue treatment.
As a wide variety of BP products including those for daily, weekly, and monthly oral dosing, and those for monthly intravenous injection/infusion have been launched in Japan, physicians are able to select from diverse options to ensure better adherence to BP therapy. Although reports in Japan and other countries [5–7] have suggested better adherence with monthly than weekly dosing, there have been no published analyses using prescription databases in Japan.
Adherence to treatment is generally expressed with compliance, which is calculated as medication possession ratio (MPR), and persistence, which is defined as time to discontinuation [8]. In the present study, we used data from the Platform for Clinical Information Statistical Analysis (CISA) database that contains data of prescriptions in 13 university hospitals in Japan (http://www.cisa.jp) to calculate compliance (MPR) and persistence with oral BPs with different dosing intervals in osteoporotic patients.
Patients and methods
Data from the CISA database were used to investigate adherence with oral BP therapy in patients with osteoporosis. Drug dispensing data at the individual level were retrieved from the CISA database, which contains substantial clinical information obtained in Japan. Data from CISA are provided in a fully anonymized form to 13 national university hospitals in this study. In the CISA database, each prescription record contains basic patient characteristics (anonymous identifier, gender, and date of birth) and information on the drug name, anatomical therapeutic chemical code, dosage, and dispensing date. Osteoporosis was diagnosed by Japanese guidelines which included the data of BMD, fracture history, and other risk factors [9].
Adherence to BP therapy was assessed with compliance and persistence. Compliance was measured with MPR, which was calculated by dividing the duration of prescription by the duration of observation. Persistence was calculated as the ratio of patients receiving BP therapy to patients prescribed with BPs at each time point. According to a previous report [6], a limit on the number of days allowed between refills, the permissible gap, was specified as 30, 30, and 45 days for daily, weekly, and monthly BPs, respectively [6] and 90 days for all in additional analysis [10].
Compliance
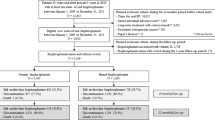
Data of 12,230 patients who were newly prescribed with oral BPs during the period between April 2006 and August 2008 were assessed for MPR over 5 years (Table 1). The patients consisted of 4178 and 8052 patients receiving BPs daily and weekly, and 2353 men and 9877 women. The mean age was 59.8 years.
Since oral BPs for monthly dosing were launched in September 2011, and became available in the 13 university hospitals in November 2011, a comparison of daily, weekly, and monthly BPs was made using data of 5039 patients who were newly prescribed with BPs during the period between November 2011 and January 2013 by calculating MPR over 1 year of daily, weekly, and monthly BPs. These patients consist of 242, 2516, and 2281 patients receiving BPs daily, weekly, and monthly, and 1150 men and 3889 women. The mean age was 62.0 years.
Persistence
Persistence over 8 years was calculated using data from 21,972 ambulatory patients who were newly prescribed with oral BPs during the period from April 2006 to January 2014 (Table 1). These patients consisted of 6768 and 15,204 patients receiving BPs daily and weekly, and 4751 men and 17,221 women. The mean age was 60.8 years.
A comparison of persistence over 2 years with daily, weekly, and monthly BPs was made using data from 9326 ambulatory patients who were newly prescribed with oral BPs during the period from November 2011 to January 2014. Patients consisted of 396, 4392, and 4538 patients receiving BPs daily, weekly, and monthly, and 2066 men and 7260 women. The mean age was 62.2 years.
Statistical analysis
Analyses in the present study were conducted in the CISA data center. The significance of the difference in MPR between two groups was tested using the Wilcoxon test, a non-parametric test, and that among three groups was tested using the Kruskal-Wallis test followed by the Bonferroni test to compare all pairs of the three groups. The persistent curve was estimated using the Kaplan-Meier method. The log-rank test was used to compare persistence between groups. All analyses were conducted using the statistical package R, version 3.1.2.
Results
Compliance
In 12,230 ambulatory patients who were newly prescribed with daily or weekly oral BP therapy during the period from April 2006 to August 2008, MPR over 5 years was 20.8 and 60.9 % for patients receiving BPs daily and weekly, respectively (p < 0.001) (Table 2).
MPR over 1 year in 5039 patients newly prescribed with daily, weekly, and monthly BP therapy from November 2011 to January 2013 was 38.6, 70.6, and 77.7 % in patients receiving the drug daily, weekly and monthly, respectively (p < 0.001). MPR was highest in patients receiving BPs monthly (Table 2).
Persistence
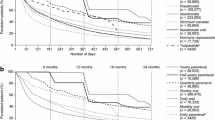
Figures 1 and 2 illustrate persistence over 8 years with daily and weekly BP therapy in 21,972 ambulatory patients who were newly prescribed with daily or weekly oral BP therapy during the period between April 2006 and January 2014. Persistence with permissible gaps of 30 and 90 days was significantly higher in patients receiving weekly than daily BP therapy at all time points (p < 0.001).
A comparison of persistence over 2 years with the three different dosing intervals in 9326 patients newly prescribed with oral BP therapy from November 2011 to January 2014 revealed that persistence was significantly higher in patients receiving BPs monthly throughout the 2-year period (p < 0.001) (Fig. 3). In an additional analysis using a permissible gap of 90 days, the persistence curve was shown with the same pattern as in Fig. 3 (Fig. 4).
Discussion
Currently, a wide variety of BP products have been developed and are available in the clinical setting. Physicians are able to select from daily, weekly, or monthly oral therapy, or monthly intravenous injection/infusion to improve adherence to BP therapy. In the present study, we were able to calculate MPR over 5 years and persistence over 8 years to investigate the relationship between dosing interval of oral BPs and adherence to BP therapy in osteoporotic patients.
In previous studies where two dosing intervals of BPs were compared in Japan and other countries [5–7, 10–18], weekly and monthly regimens were superior to daily and weekly regimens, respectively, in terms of adherence. In the present study where daily, weekly, and monthly oral BP therapies were compared, adherence increased as the dosing interval increased.
Although the better adherence of monthly than weekly BPs is generally attributable to the convenience in using monthly BPs, it has also been reported that weekly BPs show persistence superior to monthly BPs [19] and that weekly and monthly BPs did not differ significantly in terms of persistence [20]. Researchers have pointed out that detailed explanation to the patient about the fracture prevention effects, possible adverse drug reactions, and safety of BP therapy is more important than dosing interval in terms of ensuring persistence [21–24]. Persistence of BP therapy should be improved not only through prolonging the dosing interval but through individualizing the treatment to meet the patient’s preference and circumstance and thereby motivate him/her to continue treatment [25–27].
As a difference in the permissible gap may result in different findings, an additional analysis using permissible gaps of 90, 90, and 90 days for daily, weekly, and monthly BPs was conducted in addition to the analysis with 30, 30, and 45 days according to a previous report [6]. Persistence was also higher for monthly BPs than daily and weekly BPs in the additional analysis.
It has been reported that MPR, a measure of compliance, of BP (alendronate or risedronate) closely correlates with the incidence of osteoporotic fracture, and that the incidence of fracture decreases substantially in patients with a MPR of >80 % although no fracture risk reduction was observed in patients with a MPR of <50 % [4]. As it has also been reported that for each decrease of the MPR by 1 %, the risk of hip fracture increased by 0.4 % [3], it is essential to encourage patients to continue treatment as instructed and maintain a high MPR, i.e., 80 % or higher, in order to prevent fractures. Compliance to treatment for osteoporosis is generally low [28]. In order to facilitate patients to understand the efficacy of treatment and continue treatment, drugs must exhibit noticeable effects such as improvement in bone mineral density [29]. In fact, BPs have favorable effects on bone mineral density that motivate patients to continue treatment. However, compliance with BP therapy must be improved further, although compliance increases as dosing intervals increase [11]. In the present study, MPR was highest in patients receiving BPs monthly, but MPR with monthly regimens over 1 year was 77.7 %, which did not exceed 80 %. Further approaches should be made to improve compliance [7, 28, 30].
One limitation of this study is that we could not obtain data on patient’s fracture history, details of examination results, and communication between healthcare professionals and patients in the clinical setting, such as explanation about the disease, from the CISA database we used to obtain prescription data. We could not assess the effects of communication between patients and healthcare professionals. Second, as the present study was conducted in patients who visited university hospitals for the treatment of osteoporosis, the results may not be generalized to patients treated in other settings. Thirteen national university hospitals are widely located without geographical deviation, but these data from CISA are not expressed for general Japanese data.
In conclusion, adherence with BP therapy was higher in monthly regimens than in daily and weekly regimens. Monthly regimens are considered beneficial in improving adherence to oral BPs for osteoporosis treatment.
References
Briesacher BA, Andrade SE, Fouayzi H, Chan KA (2008) Comparison of drug adherence rates among patients with seven different medical conditions. Pharmacotherapy 28:437–443
Yeaw J, Benner JS, Walt JG, Sian S, Smith DB (2009) Comparing adherence and persistence across 6 chronic medication classes. J Manag Care Pharm 15:728–740
Rabenda V, Mertens R, Fabri V, Vanoverloop J, Sumkay F, Vannecke C, Deswaef A, Verpooten GA, Reginster JY (2008) Adherence to bisphosphonates therapy and hip fracture risk in osteoporotic women. Osteoporos Int 19:811–818
Siris ES, Harris ST, Rosen CJ, Barr CE, Arvesen JN, Abbott TA, Silverman S (2006) Adherence to bisphosphonate therapy and fracture rates in osteoporotic women: relationship to vertebral and nonvertebral fractures from 2 US claims databases. Mayo Clin Proc 81:1013–1022
Sakai A, Ikeda S, Okimoto N, Matsumoto H, Teshima K, Okazaki Y, Fukuda F, Arita S, Tsurukami H, Nagashima M, Yoshioka T (2014) Clinical efficacy and treatment persistence of monthly minodronate for osteoporotic patients unsatisfied with, and shifted from, daily or weekly bisphosphonates: the BP-MUSASHI study. Osteoporos Int 25:2245–2253
Cotté FE, Fardellone P, Mercier F, Gaudin AF, Roux C (2010) Adherence to monthly and weekly oral bisphosphonates in women with osteoporosis. Osteoporos Int 21:145–155
Confavreux CB, Canoui-Poitrine F, Schott AM, Ambrosi V, Tainturier V, Chapurlat RD (2012) Persistence at 1 year of oral antiosteoporotic drugs: a prospective study in a comprehensive health insurance database. Eur J Endocrinol 166:735–741
Cramer JA, Roy A, Burrell A, Fairchild CJ, Fuldeore MJ, Ollendorf DA, Wong PK (2008) Medication compliance and persistence: terminology and definitions. Value Health 11:44–47
Orimo H, Nakamura T, Hosoi T, Iki M, Uenishi K, Endo N, Ohta H, Shiraki M, Sugimoto T, Suzuki T, Soen S, Nishizawa Y, Hagino H, Fukunaga M, Fujiwara S (2012) Japanese 2011 guidelines for prevention and treatment of osteoporosis—executive summary. Arch Osteoporos 7:3–20
Weycker D, Macarios D, Edelsberg J, Oster G (2006) Compliance with drug therapy for postmenopausal osteoporosis. Osteoporos Int 17:1645–1652
Recker RR, Gallagher R, MacCosbe PE (2005) Effect of dosing frequency on bisphosphonate medication adherence in a large longitudinal cohort of women. Mayo Clin Proc 80:856–861
Cramer JA, Gold DT, Silverman SL, Lewiecki EM (2007) A systematic review of persistence and compliance with bisphosphonates for osteoporosis. Osteoporos Int 18:1023–1031
Emkey R, Koltun W, Beusterien K, Seidman L, Kivitz A, Devas V, Masanauskaite D (2005) Patient preference for once-monthly ibandronate versus once-weekly alendronate in a randomized, open-label, cross-over trial: the Boniva Alendronate Trial in Osteoporosis (BALTO). Curr Med Res Opin 21:1895–1903
Cooper A, Drake J, Brankin E (2006) Treatment persistence with once-monthly ibandronate and patient support vs. once-weekly alendronate: results from the PERSIST study. Int J Clin Pract 60:896–905
Hadji P, Minne H, Pfeifer M, Bourgeois P, Fardellone P, Licata A, Devas V, Masanauskaite D, Barrett-Connor E (2008) Treatment preference for monthly oral ibandronate and weekly oral alendronate in women with postmenopausal osteoporosis: a randomized, crossover study (BALTO II). Joint Bone Spine 75:303–310
Kastelan D, Lozo P, Stamenkovic D, Miskic B, Vlak T, Kolak Z, Milas Ahic J, Altabas V, Crncevic Orlic Z, Korsic M (2009) Preference for weekly and monthly bisphosphonates among patients with postmenopausal osteoporosis: results from the Croatian PROMO Study. Clin Rheumatol 28:321–326
Chung YS, Lim SK, Chung HY, Lee IK, Park IH, Kim GS, Min YK, Kang MI, Chung DJ, Kim YK, Choi WH, Shong MH, Park JH, Byun DW, Yoon HK, Shin CS, Lee YS, Kwon NH (2009) Comparison of monthly ibandronate versus weekly risedronate in preference, convenience, and bone turnover markers in Korean postmenopausal osteoporotic women. Calcif Tissue Int 85:389–397
Briesacher BA, Andrade SE, Harrold LR, Fouayzi H, Yood RA (2010) Adoption of once-monthly oral bisphosphonates and the impact on adherence. Am J Med 123:275–280
Gold DT, Trinh H, Safi W (2009) Weekly versus monthly drug regimens: 1-year compliance and persistence with bisphosphonate therapy. Curr Med Res Opin 25:1831–1839
Weiss TW, Henderson SC, McHorney CA, Cramer JA (2007) Persistence across weekly and monthly bisphosphonates: analysis of US retail pharmacy prescription refills. Curr Med Res Opin 23:2193–2203
Weiss TW, Gold DT, Silverman SL, McHorney CA (2006) An evaluation of patient preferences for osteoporosis medication attributes: results from the PREFER-US study. Curr Med Res Opin 22:949–960
Gold DT, Safi W, Trinh H (2006) Patient preference and adherence: comparative US studies between two bisphosphonates, weekly risedronate and monthly ibandronate. Curr Med Res Opin 22:2383–2391
McHorney CA, Schousboe JT, Cline RR, Weiss TW (2007) The impact of osteoporosis medication beliefs and side-effect experiences on non-adherence to oral bisphosphonates. Curr Med Res Opin 23:3137–3152
Keen R, Jodar E, Iolascon G, Kruse HP, Varbanov A, Mann B, Gold DT (2006) European women’s preference for osteoporosis treatment: influence of clinical effectiveness and dosing frequency. Curr Med Res Opin 22:2375–2381
Breuil V, Cortet B, Cotté FE, Arnould B, Dias-Barbosa C, Gaudin AF, Regnault A, Roborel de Climens A, Legrand E (2012) Validation of the adherence evaluation of osteoporosis treatment (ADEOS) questionnaire for osteoporotic post-menopausal women. Osteoporos Int 23:445–455
Silverman SL, Schousboe JT, Gold DT (2011) Oral bisphosphonate compliance and persistence: a matter of choice? Osteoporos Int 22:21–26
Silverman S, Gold DT (2010) Compliance and persistence with osteoporosis medications: a critical review of the literature. Rev Endocr Metab Disord 11:275–280
Solomon DH, Avorn J, Katz JN, Finkelstein JS, Arnold M, Polinski JM, Brookhart MA (2005) Compliance with osteoporosis medications. Arch Intern Med 165:2414–2419
Yood RA, Emani S, Reed JI, Lewis BE, Charpentier M, Lydick E (2003) Compliance with pharmacologic therapy for osteoporosis. Osteoporos Int 14:965–968
Clowes JA, Peel NF, Eastell R (2004) The impact of monitoring on adherence and persistence with antiresorptive treatment for postmenopausal osteoporosis: a randomized controlled trial. J Clin Endocrinol Metab 89:1117–1123
Acknowledgments
This study was performed with funding support from Ajinomoto Pharmaceuticals Co., Ltd., and the data were analyzed by the assistance of the CISA.
Conflicts of interest
H. Kishimoto has received consulting fees from Ajinomoto Pharmaceuticals Co., Ltd., Asahi Kasei Pharma, and Takeda Pharmaceutical Co., Ltd. M. Maehara is an employee of Ajinomoto Pharmaceuticals Co., Ltd.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Kishimoto, H., Maehara, M. Compliance and persistence with daily, weekly, and monthly bisphosphonates for osteoporosis in Japan: analysis of data from the CISA. Arch Osteoporos 10, 27 (2015). https://doi.org/10.1007/s11657-015-0231-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11657-015-0231-6