Abstract
Purpose
The purpose of this study was to determine associations of objectively assessed moderate-to-vigorous intensity physical activity (MVPA) and sedentary time with psychological health outcomes including depression symptoms, anxiety symptoms, and overall satisfaction with life in colon cancer survivors.
Methods
Colon cancer survivors (N = 180) from Alberta, Canada (n = 91), and Western Australia (n = 89) completed a mailed survey that assessed depression symptom severity, state anxiety, and satisfaction with life (SWL). Sedentary time and MVPA were assessed using the Actigraph® GT3X+ accelerometer (60-s epochs) via a 7-day monitoring protocol. MVPA and sedentary time were corrected for wear time and then examined as quartiles (Q). Multivariate analysis of variance was used to examine associations of MVPA and sedentary time with psychological health.
Results
There was a significant association between psychological health outcomes and objectively assessed MVPA [Wilks’ λ = 0.886, F(3382.2) = 2.156, p = 0.024] that suggested a small and significant association between MVPA and SWL (p = 0.032). A significant multivariate analysis of variance (MANOVA) [Wilks’ λ = 0.945, F(3159) = 3.1, p = 0.028] suggested participants meeting guidelines reported significantly fewer anxiety symptoms (M diff = −1.23, p = 0.027) and higher perceptions of SWL (M diff = 3.0, p = 0.008). No significant associations emerged for sedentary time [Wilks’ λ = 0.956, F(9382.3) = 0.788, p = 0.628].
Conclusions
Contrary to previously published research using self-reports, objectively assessed MVPA and sedentary time were not associated with depression symptoms. Objectively assessed MVPA was associated with SWL and anxiety outcomes in colon cancer survivors.
Implications for Cancer Survivors
Colon cancer survivors should continue to engage in regular and sustained MVPA for the accrual of psychological health benefits.
Similar content being viewed by others
Introduction
A colorectal cancer diagnosis and related treatments are associated with increased psychological distress. Several studies of colorectal cancer survivors suggest a high prevalence of both depression [1, 2] and anxiety [3, 4]. In this group, it is estimated that the overall prevalence of psychological distress ranges between 44 and 32 % [5].
Physical activity is a safe and effective intervention to facilitate favorable psychosocial health outcomes across various cancer survivor groups [6]. However, all cross-sectional studies to date have exclusively utilized self-report measures of physical activity. Self-report estimates of these behaviors are prone to measurement error that often leads to incorrect inferences about physical activity behaviors (and associated outcomes) and may bias study results [7]. Objective activity monitoring, using accelerometers and inclinometers, provides the means for precise estimates of physical activity. To date, no studies have examined objectively assessed physical activity and psychological health among colon cancer survivors.
New evidence has suggested that sedentary behavior is a health risk, even for physically active individuals [8]. This risk likely extends to cancer survivors as well [9]. Not to be confused with physical inactivity (i.e., not meeting physical activity guidelines), sedentary behaviors are performed in a seated or reclining posture and require very low energy expenditure (≤1.5 metabolic equivalents) [10, 11]. In a recently published commentary, we noted that cancer survivors spend over two thirds of their waking hours in sedentary behaviors [9]. While no studies have considered associations between sedentary behavior and psychological health in the cancer context, objectively assessed sedentary behavior has been linked to depression in the general population [12].
The primary objective of this study was to determine associations of objectively assessed moderate-to-vigorous intensity physical activity (MVPA) with psychological health outcomes including depression symptoms, anxiety symptoms, and overall satisfaction with life, among colon cancer survivors. The secondary objectives were to determine (a) associations of objectively assessed sedentary time with psychological health and (b) whether meeting physical activity guidelines (i.e., engaging in at least 150 min of MVPA per week, accumulated in bouts of at least 10 min) were associated with depression symptoms, anxiety symptoms, and satisfaction with life, and (c) whether prolonged bouts of sedentary time (i.e., total sedentary time accumulated in at least 30-min bouts) were associated with depression symptoms, anxiety symptoms, and satisfaction with life. We hypothesized objectively assessed MVPA and sedentary time would be significantly associated with fewer depression symptoms, anxiety symptoms, and higher satisfaction with life.
Method
Participants
The methods of this cross-sectional study have been described in detail elsewhere [13]. Briefly, colon cancer survivors were recruited through the Alberta Cancer Registry (Alberta, Canada) and the Western Australia (WA) Cancer Registry. The study was approved by local ethics boards at Alberta Health Services, Athabasca University, and the Department of Health WA and The University of WA.
The Alberta Cancer Registry and the WA Cancer Registry identified colon cancer survivors with histologically confirmed diagnosis of a first, primary colon cancer. Eligibility criteria included speaking English and being between the ages of 18 and 80. Eligible survivors had to (a) not be currently undergoing any adjuvant therapy, (b) be able to understand and provide written informed consent, and (c) be willing and able to wear an accelerometer for 7 days. The recruitment protocol for the two study sites was identical.
Registry procedures
Survivors were mailed a study invitation package containing (1) a letter from the registry describing the role of the registry in this study and the general purpose of the registry and (2) an invitation letter from the research team explaining the nature of the research study and what would be required of the participant. Survivors received a follow-up reminder postcard 2 weeks after the initial mailout. Participants were then sent a package containing a survey, one Actigraph® GT3X+ accelerometer (Actigraph, LLC, Pensacola, FL), a detailed instructional pamphlet describing how to use the accelerometer, an accelerometer diary (for the participant to record when accelerometer was taken off and put on), and a postage-paid priority post return envelope.
Measures
The Alberta Cancer Registry provided participants’ date of diagnosis, age at diagnosis, stage, and types of treatments received. In WA, date of diagnosis and stage were provided by the WA Cancer Registry while treatment information was gathered from the participant via self-report. Demographic and medical information including sex, age, employment, marital status, income, education, ethnicity, height and weight, and comorbidities were collected via self-report.
MVPA and sedentary time were derived from an Actigraph GT3X+ accelerometer. This instrument records acceleration using a triaxial accelerometer. Participants were provided with the accelerometer and instructed to wear it on their right hip attached by an elastic belt during all waking hours for seven consecutive days. Participants were asked to record, in a daily log, the time they put on and took off the monitor each day. Participants returned their accelerometer, survey, and logbook to the study coordinators by express post. A pragmatic cutoff of <100 counts/min was used to categorize sedentary time [14]. Commonly accepted activity count cutoffs were used to differentiate MVPA (counts/min ≥1952) from light-intensity activity (100–1951 counts/min) [14]. Data were recorded in 60-s epochs. Non-wear time was defined as intervals of at least 60 consecutive minutes of zero counts, with allowance for up to 2 min of observations of less than 50 counts/min within the non-wear interval [15]. To be considered valid, days of data collection required at least 600 min (10 h) of wear time and no excessive counts (>20,000 counts/min).
Depression was assessed using the Patient Health Questionnaire-9 (PHQ-9) [16, 17]. The PHQ-9 scores each of the nine DSM-IV criteria, and item responses range from “0” (not at all) to “3” (nearly every day). Participants were asked, “Over the last 2 weeks, how often have you been bothered by any of the following problems?” for each of the nine DSM-IV criteria, which included such items as “feeling tired or having little energy” and “feeling down, depressed, or hopeless.” Symptoms were considered present if reported for at least “more than half the days” or at least “several days” in the case of “thoughts that you would be better off dead or of hurting yourself in some way.” In this study, the PHQ-9 was used as a screener to monitor depression symptom severity. To obtain the symptom severity index, item responses were] summed for a total score. Total scores can be categorized as minimal depression (1–4), mild depression (5–9), moderate depression (10–14), moderately severe depression (15–19), and severe depression (20–27). A difference of 5 points on the PHQ-9 is considered a minimum important difference [18].
Anxiety
State anxiety was assessed using Spielberger’s State Anxiety Inventory (SAI) [19]. The SAI contains 10 items that measures how participants feel at a particular time (e.g., “I feel calm,” “I am relaxed,” “I feel worried”). The SAI state scale is scored on four levels of anxiety intensity ranging from 1 (not at all) to 4 (very much so). Scores on the SAI range from 10 to 40 with lower anxiety scores indicating fewer feelings of anxiety experiences by the participant.
Satisfaction with life
Satisfaction with life (SWL) was assessed using Diener’s Satisfaction With Life Scale [20]. The SWLS is a short five-item instrument designed to measure global cognitive judgments of satisfaction with one’s life (e.g., “The conditions of my life are excellent,” “In most ways my life is close to my ideal”). Participants were asked to indicate their degree of agreement or disagreement on a scale ranging from 1 (strongly disagree) to 7 (strongly agree). Scores on the SWL scale range from 5 to 35 with higher scores indicating greater life satisfaction.
Statistical analyses
Descriptive statistics were used to examine the demographic, health, and medical characteristics of the sample. Multivariate analysis of variance (MANOVA) procedures were used to test for differences in depression and anxiety symptoms and SWL across quartiles of overall MVPA minutes. Participants were also classified as either meeting physical activity guidelines (i.e., both overall MVPA and MVPA accumulated in at least 10-min bouts) or not (i.e., <150 min a week). For sedentary time, MANOVA was used to test for differences in depression and anxiety symptoms and SWL across quartiles of (a) overall sedentary time and (b) sedentary time accumulated in at least 30-min bouts. Pairwise comparison procedures were conducted on all significant ANOVA statistics. Covariates were included if they had (a) any evidence of association (p < 0.20) with the dependent variable and (b) demonstrated clinical relevance based on previous research. All models covaried on sex, body mass index (BMI), disease stage, chemotherapy, age, months since diagnosis, total sedentary minutes (for MVPA models), and total MVPA minutes (for sedentary time models). Sidak corrections were applied to all comparisons, and an alpha (α) of 0.05 was used as a threshold for determining statistical significance.
Results
Participant characteristics
A total of 197 survivors responded to the registry mailouts representing a response rate across the two study sites of 22 %. Overall, 180 participants provided complete accelerometer and psychological health data. These participants did not significantly differ from the 17 participants who had missing accelerometer or psychological health data on any demographic, clinical, or behavioral characteristics. There were small significant differences between WA and Alberta participants. Participants from Alberta were approximately 3 years younger (p = 0.025), had fewer comorbidities (p = 0.006), and were on average 4 months further past diagnosis (p < 0.001) compared to WA participants.
Complete information related to demographic, medical, and behavioral data is located in Table 1. The mean age of the sample was 64.3 years (SD = 10.3) and 55 % were male. On average, this sample reported mild depression symptoms (PHQscore = 3.5, SD = 4.5) and anxiety symptoms (Anxietyscore = 18.2, SD = 3.1) and were largely satisfied with their lives (SWLscore = 26.2, SD = 6.5). Overall, 74.6 % of participants had no depression symptoms, 16.3 % reported minimal symptoms, 4 % reported minor depression, and 4.5 % reported major depression. When considering total overall MVPA minutes per day, 45 % were achieving public health guidelines for MVPA. However, when considering MVPA accumulated in at least 10-min bouts, 16 % were achieving guidelines.
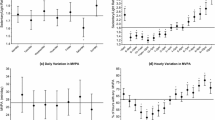
MVPA
Cut points for MVPA minutes per day were <12.9 (Q1), 12.9 to <23.8 (Q2), 23.8 to <41.3 (Q3), and ≥41.3 (Q4). The overall MANOVA was significant when comparing psychological health outcomes across quartiles [Wilks’ λ = 0.886, F(9382.2) = 2.156, p = 0.024]. Univariate ANOVA analyses revealed significant differences in SWL (F = 3.0, p = 0.032); linear independent pairwise comparisons suggested a significant difference between Q2 and Q4 (M diff = 4.1, p = 0.034). While significant linear trends were observed for all psychological health outcomes, there were no significant associations of total MVPA with depression and anxiety symptoms (Table 2).
When comparing participants meeting versus not meeting public health MVPA guidelines (using total overall MVPA minutes) on psychosocial health outcomes, the overall MANOVA was significant [Wilks’ λ = 0.945, F(3159) = 3.1, p = 0.028]. Univariate ANOVA indicated significant differences in anxiety symptoms (F = 5.012, p = 0.027) and SWL (F = 7.239, p = 0.008); linear independent pairwise comparisons suggested participants meeting MVPA guidelines reported significantly fewer anxiety symptoms (M diff = −1.23, p = 0.027) and higher perceptions of SWL (M diff = 3.0, p = 0.008) (Table 3).
MVPA in 10-min bouts
Cut points for MVPA minutes per day accrued in minimum 10-min bouts were <0.34 (Q1), 0.34 to <4.5 (Q2), 4.5 to <12.7 (Q3), and ≥12.7 (Q4). There were no differences in psychological health outcomes across quartiles [Wilks’ λ = 0.968, F(9382.2) = 0.569, p = 0.822]. Further, there were no differences in psychological health outcomes between participants meeting versus not meeting MVPA guidelines (i.e., MVPA minutes accrued in at least 10-min bouts) [Wilks’ λ = 0.993, F(3159) = 0.390, p = 0.760].
Sedentary time
Cut points for overall sedentary time (hours) per day were <7.9 (Q1), 7.9 to <8.8 (Q2), 8.8 to <9.8 (Q3), and ≥9.8 (Q4). For overall sedentary time, no significant differences emerged for any of the psychological health outcomes across sitting time quartiles [Wilks’ λ = 0.961, F(9382.3) = 0.614, p = 0.785]. Cut points for sedentary time accrued in at least 30-min bouts (hours) were <1.31 (Q1), 1.31 to <2.18 (Q2), 2.18 to <3.41 (Q3), and ≥3.41 (Q4). When entered as the independent variable, no significant differences emerged for any of the psychological health outcomes [Wilks’ λ = 0.975, F(9382.3) = 0.448, p = 0.909] (Table 2).
Discussion
The primary objective of this study was to determine the associations of objectively assessed physical activity and sedentary time with psychological health outcomes including depression symptoms, anxiety symptoms, and overall satisfaction with life (SWL) in colon cancer survivors. MVPA and sedentary time were not associated with depression symptoms. However, we did find that higher levels of MVPA were associated with greater SWL and lower anxiety. Our study is the first to examine the associations of objectively assessed MVPA and sedentary behavior with psychological health outcomes among a sample of colon cancer survivors.
Our data suggested objectively assessed MVPA time was not associated with depression symptom severity. No associations emerged when both comparing quartiles of MVPA and participants meeting and not meeting MVPA guidelines (i.e., 150 min of MVPA per week accumulated in at least 10-min bouts). Recently published systematic reviews and meta-analyses of randomized controlled trials concluded physical activity has small-to-moderate positive effects on depressive and anxiety symptoms as well as SWL among cancer survivors [6, 21, 22]. Cross-sectional studies have demonstrated significant associations between physical activity and depression among a variety of tumor groups [23–25]. However, these aforementioned studies utilized self-report measures of physical activity; therefore, differences in conclusions may be a result of the method used to assess MVPA. Our study corroborates colorectal cancer survivor literature suggesting physical activity may not be associated with depression symptoms in this population. For example, Lynch and colleagues [26] prospectively surveyed 1966 colorectal cancer survivors and found self-reported physical activity was not associated with psychological distress (including depression, anxiety, and somatization). Future research should further examine how the physical activity assessment method influences associations with depression and anxiety symptoms, and SWL, and whether associations between MVPA and depression symptoms vary with respect to tumor site.
Public health guidelines for MVPA suggest activity should be accumulated in at least 10-min bouts. However, we reported no significant associations with any psychological health outcomes when comparing participants meeting and not meeting MVPA guidelines (using minutes accumulated in 10-min bouts). However, when considering total MVPA minutes per day, significant associations were found for anxiety and SWL. This finding corroborates our previously published data examining health-related quality of life (HRQoL) outcomes in that significant differences were not observed when considering MVPA accumulated in 10-min bouts (although some clinically important differences did emerge) [13]. Specifically, associations with HRQoL and fatigue were attenuated when only considering MVPA accumulated in at least 10-min bouts. From a public health perspective, colon cancer survivors should make efforts to simply move more frequently at a moderate intensity. To date, there are no other published studies that have examined objectively assessed MVPA minutes in colon cancer survivors.
Our data suggested neither overall sedentary time nor sedentary time accumulated in at least 30-min bouts were associated with psychological health outcomes. To our knowledge, this is the first study to examine associations between objectively assessed sedentary time and psychological health outcomes in any tumor group. The lack of association between these outcomes is not consistent with previously published studies in the general population. For example, Vallance and colleagues recently reported lower odds of depression were associated with decreasing sedentary time (i.e., objectively assessed) among a population-based sample of US adults [12]. Future research should continue to examine these psychological health outcomes and their associations with sedentary time given cancer survivors spent a large proportion of their day in sedentary pursuits [27, 28].
There are several limitations to the research that need mention. The cross-sectional study design limits our ability to draw conclusions relating to causation. The accelerometers used in this study only provide an indicator of overall MVPA and sedentary time. Although a precise assessment, this method does not provide any information related to the context of the MVPA (walking, cycling, indoor/outdoor) and sedentary behavior (e.g., television viewing, driving, computer use). It has been postulated that some sedentary behaviors (e.g., television viewing) may remove individuals from social interactions and further increase their risk for depression [29]. However, other sedentary behaviors may promote social interaction (e.g., conversing over a cup of coffee, participating in Internet forums/online chat) or well-being (e.g., sitting and doing a puzzle) and thus be beneficial for psychological health [30]. While we examined sedentary time in prolonged, 30-min bouts, future studies should elect to explore longer bouts of accumulated sedentary time (e.g., 60 min, 2 h). This study did not assess sleep time, which is emerging as a potentially important behavior for both physiological and psychological health. Future studies should evaluate sleep time for a more comprehensive analysis of behaviors occurring throughout the day and night. Furthermore, as posture is not directly measured with the Actigraph accelerometer, we are unable to determine whether individuals are sitting or standing. It is understood that a proportion of accelerometer-derived sedentary time may be comprised for time spent standing still (e.g., while queuing or waiting for a bus).
Study participants had relatively few depression and anxiety symptoms and high perceptions of their SWL, which limited our ability to detect whether increased MVPA and/or decreased sedentary time was associated with these psychological health outcomes. It is possible that survivors with moderate or severe depression, high anxiety, and low SWL may have refrained from participating in this study. The lack of statistical significance may have also been an artifact of the small sample size. Post hoc sample size calculations suggested we needed 63 participants per quartile to detect a significant difference on the PHQ-9 scores. Strengths of this study include the objective measurement of physical activity and sedentary time and the use of well-established psychological assessment tools. Our study presents objectively assessed MVPA and sedentary time data on a relatively homogeneous sample of colon cancer survivors in contrast to the heterogeneous (and small) samples that have been published to date [31–34].
In this study, objectively assessed MVPA and sedentary time were not associated with depression symptoms. Objectively assessed MVPA was associated with SWL and anxiety outcomes in colon cancer survivors. Future physical activity and sedentary behavior research with cancer survivors should continue to utilize objective and more precise estimates of these health behaviors given the well-established limitations of self-reported estimates [7].
References
Krebber AM, Buffart LM, Kleijn G, et al. Prevalence of depression in cancer patients: a meta-analysis of diagnostic interviews and self-report instruments. Psychooncology. 2014;23:121–30.
Massie MJ. Prevalence of depression in patients with cancer. J Natl Cancer Inst Monogr. 2004;57–71.
Mullens AB, McCaul KD, Erickson SC, Sandgren AK. Coping after cancer: risk perceptions, worry, and health behaviors among colorectal cancer survivors. Psychooncology. 2004;13:367–76.
Tavoli A, Mohagheghi MA, Montazeri A, et al. Anxiety and depression in patients with gastrointestinal cancer: does knowledge of cancer diagnosis matter? BMC Gastroenterol. 2007;7:28.
Dunn J, Ng SK, Holland J, et al. Trajectories of psychological distress after colorectal cancer. Psychooncology. 2013;22:1759–65.
Mishra SI, Scherer RW, Geigle PM, et al. Exercise interventions on health-related quality of life for cancer survivors. Cochrane Database Syst Rev. 2012;8:CD007566.
Ainsworth BE, Caspersen CJ, Matthews CE, et al. Recommendations to improve the accuracy of estimates of physical activity derived from self report. J Phys Act Health. 2012;9 Suppl 1:S76–84.
Owen N. Sedentary behavior: understanding and influencing adults’ prolonged sitting time. Prev Med. 2012;55:535–9.
Lynch BM, Dunstan DW, Vallance JK, Owen N. Don’t take cancer sitting down: a new survivorship research agenda. Cancer. 2013;119:1928–35.
Owen N. Ambulatory monitoring and sedentary behaviour: a population-health perspective. Physiol Meas. 2012;33:1801–10.
Sedentary Behaviour Research N: Letter to the editor: standardized use of the terms “sedentary” and “sedentary behaviours”. Applied Physiology, Nutrition, and Metabolism 2012; 37: 540–542.
Vallance JK, Winkler EA, Gardiner PA, et al. Associations of objectively-assessed physical activity and sedentary time with depression: NHANES (2005–2006). Prev Med. 2011;53:284–8.
Vallance JK, Boyle T, Courneya KS, Lynch BM. Associations of objectively-assessed physical activity and sedentary time with health-related quality of life among colon cancer survivors. Cancer, 2014.
Freedson PS, Melanson E, Sirard J. Calibration of the Computer Science and Applications Inc. accelerometer. Med Sci Sports Exerc. 1998;30:777–81.
Matthews CE, Chen KY, Freedson PS, et al. Amount of time spent in sedentary behaviors in the United States, 2003–2004. Amican J Epidemiol. 2008;167:875–81.
Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–13.
Kroenke K, Spitzer RL, Williams JB, Lowe B. The Patient Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: a systematic review. Gen Hosp Psychiatry. 2010;32:345–59.
Löwe B, Kroenke K, Herzog W, Gräfe K. Measuring depression outcome with a brief self-report instrument: sensitivity to change of the Patient Health Questionnaire (PHQ-9). J Affect Disord. 2004;81(1):61–6.
Spielberger C, Gorsuch R, Lushene R. Manual for the state-trait anxiety inventory. 1970
Diener D, Emmons RA, Larsen RJ, Griffin S. The Satisfaction With Life Scale. J Person Assess. 1985;49:71–5.
Brown JC, Huedo-Medina TB, Pescatello LS, et al. The efficacy of exercise in reducing depressive symptoms among cancer survivors: a meta-analysis. PLoS One. 2012;7:e30955.
Craft LL, Vaniterson EH, Helenowski IB, Rademaker AW, Courneya KS. Exercise effects on depressive symptoms in cancer survivors: a systematic review and meta-analysis. Cancer Epidemiol Biomark Prev. 2012;21:3–19.
Faul LA, Jim HS, Minton S, et al. Relationship of exercise to quality of life in cancer patients beginning chemotherapy. J Pain Symptom Manag. 2011;41:859–69.
Penttinen HM, Saarto T, Kellokumpu-Lehtinen P, et al. Quality of life and physical performance and activity of breast cancer patients after adjuvant treatments. Psychooncology 2010.
Rogers LQ, Markwell SJ, Courneya KS, McAuley E, Verhulst S. Physical activity type and intensity among rural breast cancer survivors: patterns and associations with fatigue and depressive symptoms. J Cancer Surviv. 2011;5:54–61.
Lynch BM, Cerin E, Owen N, Hawkes AL, Aitken JF. Television viewing time of colorectal cancer survivors is associated prospectively with quality of life. Cancer Causes Control. 2011;22:1110–20.
Lynch BM, Dunstan DW, Healy GN, et al. Objectively measured physical activity and sedentary time of breast cancer survivors, and associations with adiposity: findings from NHANES (2003–2006). Cancer Causes Control. 2010;21:283–8.
Lynch BM, Dunstan DW, Winkler E, et al. Objectively assessed physical activity, sedentary time and waist circumference among prostate cancer survivors: findings from the National Health and Nutrition Examination Survey (2003–2006). Eur J Cancer Care (Engl). 2011;20:514–9.
Kraut R, Patterson M, Lundmark V, et al. Internet paradox. A social technology that reduces social involvement and psychological well-being? Am Psychol. 1998;53:1017–31.
Teychenne M, Ball K, Salmon J. Sedentary behavior and depression among adults: a review. Int J Behav Med. 2010;17:246–54.
George SM, Alfano CM, Groves J, et al. Objectively measured sedentary time is related to quality of life among cancer survivors. PLoS One. 2014;9:e87937.
Loprinzi PD, Lee H. Rationale for promoting physical activity among cancer survivors: literature review and epidemiologic examination. Oncol Nurs Forum. 2014;41:117–25.
Loprinzi PD, Lee H, Cardinal BJ. Objectively measured physical activity among US cancer survivors: considerations by weight status. J Cancer Surviv. 2013;7:493–9.
Ruiz-Casado A, Verdugo AS, Solano MJ, et al. Objectively assessed physical activity levels in Spanish cancer survivors. Oncol Nurs Forum. 2014;41:E12–20.
Acknowledgments
Jeff Vallance and Kerry Courneya are supported by the Canada Research Chairs program. Jeff Vallance is also supported by a Population Health Investigator Award from Alberta Innovates – Health Solutions. Brigid Lynch is supported by a NHMRC Public Health Training Fellowship (#586727) and the Victorian Government’s Operational Infrastructure Support Program. We would like to acknowledge Parneet Sethi and Dr. Elisabeth Winkler for their assistance in data processing and analyses.
Conflict of interest
Drs. Jeff Vallance, Terry Boyle, Kerry Courneya, and Brigid Lynch declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Vallance, J.K., Boyle, T., Courneya, K.S. et al. Accelerometer-assessed physical activity and sedentary time among colon cancer survivors: associations with psychological health outcomes. J Cancer Surviv 9, 404–411 (2015). https://doi.org/10.1007/s11764-014-0409-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11764-014-0409-8