Abstract
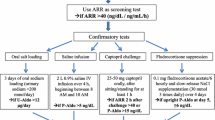
Primary aldosteronism with a prevalence of 8 % of hypertension and 20 % of pharmacologically resistant hypertension is the most common secondary cause of hypertension. Yet, the diagnosis is missed in the vast majority of patients. Current clinical practice guidelines recommend screening for primary aldosteronism in patients with sustained elevation of blood pressure (BP) ≥150/100 mmHg if possible prior to initiation of antihypertensive therapy, and in patients with resistant hypertension, spontaneous or diuretic-induced hypokalemia, adrenal incidentaloma, obstructive sleep apnea, a family history of early onset of hypertension or cerebrovascular accident <age 40, and first-degree relatives of patients with primary aldosteronism. Clinical and laboratory methods of screening, confirmatory testing, subtype classification, and medical and surgical management are systematically reviewed and illustrated with a clinical case.



Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
World Health Organization. A global brief on hypertension. Geneva: World Health Orgaanization; 2013.
Franco OH, Peeters A, Bonneux L, et al. Blood pressure in adulthood and life expectancy with cardiovascular disease in men and women: life course analysis. Hypertension. 2005;46:280–6.
Lim SS, Vos T, Flaxman AD, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–60.
Ettehad D, Emdin CA, Kiran A, et al. Blood pressure lowering for prevention of cardiovascular disease and death: a systematic review and meta-analysis. Lancet. 2016;387:957–67.
Roth GA, Nguyen G, Forouzanfar MH, et al. Estimates of global and regional premature cardiovascular mortality in 2025. Circulation. 2015;132:1270–82.
Lewington S, Clarke R, Qizilbash N, et al. Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–13.
Petruski-Ivleva N, Viera AJ, Shimbo D, et al. Longitudinal patterns of change in systolic blood pressure and incidence of cardiovascular disease. The Atherosclerosis Risk in Communities Study. Hypertension. 2016;67:1150–56.
SPRINT Research Group, Wright Jr JT, Williamson JD, et al. A randomized trial of intensive versus standard blood pressure control. N Engl J Med. 2015;373:2103–16. This landmark clinical trial randomized hypertensive patients at increased risk for cardiovascular disease to a standard vs. intensive BP lowering protocol. The study demonstrated major improvement in cardiovascular outcomes at with intensive BP lowering to <120 mmHg compared to < 140 mmHg.
Whelton PK. The elusiveness of worldwide blood pressure control. Annu Rev Public Health. 2015;36:109–30.
Calhoun DA, Jones D, Textor S, et al. Resistant hypertension: diagnosis, evaluation and treatment. A scientific statement from the American Heart Association Professional Education Committee. Hypertension. 2008;51:1403–19.
Persell SD. Prevalence of resistant hypertension in the United States, 2003–2008. Hypertension. 2011;57:1076–80.
Mulatero P, Stowasser M, Loh KC, et al. Increased diagnosis of primary aldosteronism, including surgically correctable forms, in centers from five continents. J Clin Endocrinol Metab. 2004;89:1045–50.
Calhoun DA. Hyperaldosteronism as a common cause of resistant hypertension. Annu Rev Med. 2013;64:233–7.
Funder JW, Carey RM, Mantero F, et al. The management of primary aldosteronism: case detection, diagnosis, and treatment: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2016;101:1889–916. This updated Endocrine Society Clinical Practice Guideline recommends screening for primary aldosteronism in any patient with sustained BP ≥ 150/100 mmHg. The Guideline recommends methods and conditions for screening, confirmation of the diagnosis, lateralization and treatment.
Milliez P, Girerd X, Plouin PF, et al. Evidence for increased rate of cardiovascular events in patients with primary aldosteronism. J Am Coll Cardiol. 2005;19:1243–8.
Savard S, Amar L, Plouin PF, et al. Cardiovascular complications associated with primary aldosteronism. Hypertension. 2013;62:331–6.
Bernini G, Galetta F, Franzoni F, et al. Arterial stiffness, intima-media thickness and carotid artery fibrosis in patients with primary aldosteronism. J Hypertens. 2008;26:2399–405.
Ahmed AH, Cowley D, Wolley M, et al. Seated saline suppression testing for the diagnosis of primary aldosteronism. J Clin Endocrinol Metab. 2014;99:2745–53. This study is the first to show that saline suppression testing in the seated rather than recumbent position is at least as specific as other confirmatory tests for primary aldosteronism, including the fludrocortisone suppression test.
Reardon MA, Angle JF, Abi-Jaoudeh N, et al. Intra-procedural cortisol levels in the evaluation of proper catheter placement in adrenal venous sampling. J Vasc Interv Radiol. 2011;22:1175–80.
Shada A, Stokes JB, Simpson GB, et al. Adrenalectomy for adrenal-mediated hypertension: national surgical quality improvement program analysis of an institutional experience. Am Surg. 2014;80:1152–8.
Ghorayeb NE, Mazzuco TL, Bourdeua I, et al. Basal and post ACTH aldosterone and its ratios are useful during adrenal vein sampling in primary aldosteronism. J Clin Endocrinol Metab. 2016;101:1826–35.
Wolley M, Ahmed A, Gordon R, et al. Does contralateral suppression at adrenal venous sampling predict outcome following unilateral adrenalectomy for primary aldosteronism? A retrospective study. J Hypertens. 2015;33 Suppl 1, e121.
Monticone S, Satoh F, Viola A, et al. Clinical significance of contralateral adrenal suppression during adrenal vein sampling in primary aldosteronism. J Hypertens. 2015;33 Suppl 1, e120. This study is the first to convincingly demonstrate the value of contralateral aldosterone suppression during AVS as predictive of positive surgical outcomes. The study recommends contralateral suppression, along with selectivity and lateralization indices, as routine measures with which to interpret AVS results.
Eisenhofer F, Dekkers T, Peitzsch M, et al. Mass spectroscopy-based adrenal and peripheral venous steroid profiling for subtyping primary aldosteronism. Clin Chem. 2016;62:514–24.
Umakoshi H, Naruse M, Wada N, et al. Adrenal venous sampling in patients with positive screening but negative confirmatory testing for primary aldosteronism. Hypertension. 2016;67:1014–9.
Iwakura Y, Ito S, Morimoto R, et al. Renal resistive index predicts postoperative blood pressure outcome in primary aldosteronism. Hypertension. 2016;67:654–60.
Ghazi L, Dudenbostel T, Lin CP, et al. Urinary sodium excretion predicts blood pressure response to spironolactone in patients with resistant hypertension independent of aldosterone status. J Hypertens. 2016;34:1005–10.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Robert M. Carey declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
This article is part of the Topical Collection on Hypertension
Rights and permissions
About this article
Cite this article
Carey, R.M. Diagnosing and Managing Primary Aldosteronism in Hypertensive Patients: a Case-Based Approach. Curr Cardiol Rep 18, 97 (2016). https://doi.org/10.1007/s11886-016-0774-1
Published:
DOI: https://doi.org/10.1007/s11886-016-0774-1