Abstract
Purpose of Review
Impairments in mitochondrial function in patients with insulin resistance and type 2 diabetes have been disputed for decades. This review aims to briefly summarize the current knowledge on mitochondrial dysfunction in metabolic tissues and to particularly focus on addressing a new perspective of mitochondrial dysfunction, the altered capacity of mitochondria to communicate with other organelles within insulin-resistant tissues.
Recent Findings
Organelle interactions are temporally and spatially formed connections essential for normal cell function. Recent studies have shown that mitochondria interact with various cellular organelles, such as the endoplasmic reticulum, lysosomes and lipid droplets, forming inter-organelle junctions.
Summary
We will discuss the current knowledge on alterations in these mitochondria-organelle interactions in insulin resistance and diabetes, with a focus on changes in mitochondria-lipid droplet communication as a major player in ectopic lipid accumulation, lipotoxicity and insulin resistance.


Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: •• Of major importance
Zimmet P, Alberti KG, Magliano DJ, Bennett PH. Diabetes mellitus statistics on prevalence and mortality: facts and fallacies. Nat Rev Endocrinol. 2016;12(10):616–22. https://doi.org/10.1038/nrendo.2016.105.
Montgomery MK, Turner N. Mitochondrial dysfunction and insulin resistance: an update. Endocr Connect. 2015;4(1):R1–R15. https://doi.org/10.1530/EC-14-0092.
Suliman HB, Piantadosi CA. Mitochondrial quality control as a therapeutic target. Pharmacol Rev. 2016;68(1):20–48. https://doi.org/10.1124/pr.115.011502.
Montgomery MK, De Nardo W, Watt MJ. Impact of lipotoxicity on tissue “cross talk” and metabolic regulation. Physiology (Bethesda). 2019;34(2):134–49. https://doi.org/10.1152/physiol.00037.2018.
Ly LD, Xu S, Choi SK, Ha CM, Thoudam T, Cha SK, et al. Oxidative stress and calcium dysregulation by palmitate in type 2 diabetes. Exp Mol Med. 2017;49(2):e291. https://doi.org/10.1038/emm.2016.157.
Giralt M, Villarroya F. Mitochondrial uncoupling and the regulation of glucose homeostasis. Curr Diabetes Rev. 2017;13(4):386–94. https://doi.org/10.2174/1573399812666160217122707.
Horvath SE, Daum G. Lipids of mitochondria. Prog Lipid Res. 2013;52(4):590–614. https://doi.org/10.1016/j.plipres.2013.07.002.
•• Paradies G, Paradies V, Ruggiero FM, Petrosillo G. Role of cardiolipin in mitochondrial function and dynamics in health and disease: molecular and pharmacological aspects. Cells. 2019;8(7). https://doi.org/10.3390/cells8070728. This review discusses the role of cardiolipin in mitochondrial function and dynamics.
Ma ZA, Zhao Z, Turk J. Mitochondrial dysfunction and beta-cell failure in type 2 diabetes mellitus. Exp Diabetes Res. 2012;2012:703538. https://doi.org/10.1155/2012/703538.
Han X, Yang J, Cheng H, Yang K, Abendschein DR, Gross RW. Shotgun lipidomics identifies cardiolipin depletion in diabetic myocardium linking altered substrate utilization with mitochondrial dysfunction. Biochemistry. 2005;44(50):16684–94. https://doi.org/10.1021/bi051908a.
Han X, Yang J, Yang K, Zhao Z, Abendschein DR, Gross RW. Alterations in myocardial cardiolipin content and composition occur at the very earliest stages of diabetes: a shotgun lipidomics study. Biochemistry. 2007;46(21):6417–28. https://doi.org/10.1021/bi7004015.
Daum G, Vance JE. Import of lipids into mitochondria. Prog Lipid Res. 1997;36(2):103–30. https://doi.org/10.1016/S0163-7827(97)00006-4.
Sivitz WI, Yorek MA. Mitochondrial dysfunction in diabetes: from molecular mechanisms to functional significance and therapeutic opportunities. Antioxid Redox Signal. 2010;12(4):537–77. https://doi.org/10.1089/ars.2009.2531.
Youle RJ, van der Bliek AM. Mitochondrial fission, fusion, and stress. Science (New York, NY). 2012;337(6098):1062–5. https://doi.org/10.1126/science.1219855.
Frezza C, Cipolat S, Martins de Brito O, Micaroni M, Beznoussenko GV, Rudka T, et al. OPA1 controls apoptotic cristae remodeling independently from mitochondrial fusion. Cell. 2006;126(1):177–89. https://doi.org/10.1016/j.cell.2006.06.025.
Molina AJ, Wikstrom JD, Stiles L, Las G, Mohamed H, Elorza A, et al. Mitochondrial networking protects beta-cells from nutrient-induced apoptosis. Diabetes. 2009;58(10):2303–15. https://doi.org/10.2337/db07-1781.
Zorzano A, Liesa M, Palacin M. Mitochondrial dynamics as a bridge between mitochondrial dysfunction and insulin resistance. Arch Physiol Biochem. 2009;115(1):1–12. https://doi.org/10.1080/13813450802676335.
Montaigne D, Marechal X, Coisne A, Debry N, Modine T, Fayad G, et al. Myocardial contractile dysfunction is associated with impaired mitochondrial function and dynamics in type 2 diabetic but not in obese patients. Circulation. 2014;130(7):554–64. https://doi.org/10.1161/circulationaha.113.008476.
Fealy CE, Mulya A, Lai N, Kirwan JP. Exercise training decreases activation of the mitochondrial fission protein dynamin-related protein-1 in insulin-resistant human skeletal muscle. J Appl Physiol (1985). 2014;117(3):239–45. https://doi.org/10.1152/japplphysiol.01064.2013.
Yoon Y, Galloway CA, Jhun BS, Yu T. Mitochondrial dynamics in diabetes. Antioxid Redox Signal. 2011;14(3):439–57. https://doi.org/10.1089/ars.2010.3286.
Yang L, Long Q, Liu J, Tang H, Li Y, Bao F, et al. Mitochondrial fusion provides an ‘initial metabolic complementation’ controlled by mtDNA. Cell Mol Life Sci. 2015;72(13):2585–98. https://doi.org/10.1007/s00018-015-1863-9.
Lavorato M, Iyer VR, Dewight W, Cupo RR, Debattisti V, Gomez L, et al. Increased mitochondrial nanotunneling activity, induced by calcium imbalance, affects intermitochondrial matrix exchanges. Proc Natl Acad Sci U S A. 2017;114(5):E849–e58. https://doi.org/10.1073/pnas.1617788113.
•• Vincent AE, White K, Davey T, Philips J, Ogden RT, Lawless C, et al. Quantitative 3D mapping of the human skeletal muscle mitochondrial network. Cell Rep. 2019;26(4):996–1009.e4. https://doi.org/10.1016/j.celrep.2019.01.010. This study maps the mitochondrial network in human muscle at electron microscopy resolution and defines the ultrastructure of mitochondrial nanotunnels.
•• Gatta AT, Levine TP. Piecing together the patchwork of contact sites. Trends Cell Biol. 2017;27(3):214–29. https://doi.org/10.1016/j.tcb.2016.08.010. This is an important review on inter-organelle communication and organelle contact sites.
•• Simmen T, Tagaya M. Organelle communication at membrane contact sites (MCS): from curiosity to center stage in cell biology and biomedical research. Adv Exp Med Biol. 2017;997:1–12. https://doi.org/10.1007/978-981-10-4567-7_1. This review is a detailed summary of membrane contact sites and the importance of these contact sites in organelle function.
•• Scorrano L, De Matteis MA, Emr S, Giordano F, Hajnóczky G, Kornmann B, et al. Coming together to define membrane contact sites. Nat Commun. 2019;10(1):1287. https://doi.org/10.1038/s41467-019-09253-3. This scientific opinion paper provides guidelines for the experimental definition and analysis of contact sites.
Lackner LL, Ping H, Graef M, Murley A, Nunnari J. Endoplasmic reticulum-associated mitochondria-cortex tether functions in the distribution and inheritance of mitochondria. Proc Natl Acad Sci U S A. 2013;110(6):E458–67. https://doi.org/10.1073/pnas.1215232110.
•• Eisenberg-Bord M, Shai N, Schuldiner M, Bohnert M. A tether is a tether is a tether: tethering at membrane contact sites. Dev Cell. 2016;39(4):395–409. https://doi.org/10.1016/j.devcel.2016.10.022. This review provides guidelines that define the prerequisites for categorizing a protein as a tether.
Liu Y, Zhu X. Endoplasmic reticulum-mitochondria tethering in neurodegenerative diseases. Transl Neurodegener. 2017;6:21. https://doi.org/10.1186/s40035-017-0092-6.
Kornmann B, Currie E, Collins SR, Schuldiner M, Nunnari J, Weissman JS, et al. An ER-mitochondria tethering complex revealed by a synthetic biology screen. Science (New York, NY). 2009;325(5939):477–81. https://doi.org/10.1126/science.1175088.
Helle SC, Kanfer G, Kolar K, Lang A, Michel AH, Kornmann B. Organization and function of membrane contact sites. Biochim Biophys Acta. 2013;1833(11):2526–41. https://doi.org/10.1016/j.bbamcr.2013.01.028.
Theurey P, Tubbs E, Vial G, Jacquemetton J, Bendridi N, Chauvin MA, et al. Mitochondria-associated endoplasmic reticulum membranes allow adaptation of mitochondrial metabolism to glucose availability in the liver. J Mol Cell Biol. 2016;8(2):129–43. https://doi.org/10.1093/jmcb/mjw004.
Hayashi T, Fujimoto M. Detergent-resistant microdomains determine the localization of sigma-1 receptors to the endoplasmic reticulum-mitochondria junction. Mol Pharmacol. 2010;77(4):517–28. https://doi.org/10.1124/mol.109.062539.
Vance JE. Phospholipid synthesis in a membrane fraction associated with mitochondria. J Biol Chem. 1990;265(13):7248–56.
Szabadkai G, Bianchi K, Varnai P, De Stefani D, Wieckowski MR, Cavagna D, et al. Chaperone-mediated coupling of endoplasmic reticulum and mitochondrial Ca2+ channels. J Cell Biol. 2006;175(6):901–11. https://doi.org/10.1083/jcb.200608073.
Booth DM, Enyedi B, Geiszt M, Varnai P, Hajnoczky G. Redox nanodomains are induced by and control calcium signaling at the ER-mitochondrial interface. Mol Cell. 2016;63(2):240–8. https://doi.org/10.1016/j.molcel.2016.05.040.
•• Takeda K, Nagashima S, Shiiba I, Uda A, Tokuyama T, Ito N, et al. MITOL prevents ER stress-induced apoptosis by IRE1alpha ubiquitylation at ER-mitochondria contact sites. EMBO J. 2019;38(15):e100999. https://doi.org/10.15252/embj.2018100999. This study defines MITOL as a novel player in mitochondria-ER contact.
Hamasaki M, Furuta N, Matsuda A, Nezu A, Yamamoto A, Fujita N, et al. Autophagosomes form at ER-mitochondria contact sites. Nature. 2013;495(7441):389–93. https://doi.org/10.1038/nature11910.
Horner SM, Liu HM, Park HS, Briley J, Gale M Jr. Mitochondrial-associated endoplasmic reticulum membranes (MAM) form innate immune synapses and are targeted by hepatitis C virus. Proc Natl Acad Sci U S A. 2011;108(35):14590–5. https://doi.org/10.1073/pnas.1110133108.
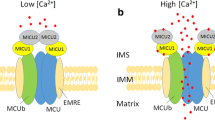
Tarasov AI, Griffiths EJ, Rutter GA. Regulation of ATP production by mitochondrial Ca(2+). Cell Calcium. 2012;52(1):28–35. https://doi.org/10.1016/j.ceca.2012.03.003.
Betz C, Stracka D, Prescianotto-Baschong C, Frieden M, Demaurex N, Hall MN. Feature article: mTOR complex 2-Akt signaling at mitochondria-associated endoplasmic reticulum membranes (MAM) regulates mitochondrial physiology. Proc Natl Acad Sci U S A. 2013;110(31):12526–34. https://doi.org/10.1073/pnas.1302455110.
De Vos KJ, Morotz GM, Stoica R, Tudor EL, Lau KF, Ackerley S, et al. VAPB interacts with the mitochondrial protein PTPIP51 to regulate calcium homeostasis. Hum Mol Genet. 2012;21(6):1299–311. https://doi.org/10.1093/hmg/ddr559.
Iwasawa R, Mahul-Mellier AL, Datler C, Pazarentzos E, Grimm S. Fis1 and Bap31 bridge the mitochondria-ER interface to establish a platform for apoptosis induction. EMBO J. 2011;30(3):556–68. https://doi.org/10.1038/emboj.2010.346.
de Brito OM, Scorrano L. Mitofusin 2 tethers endoplasmic reticulum to mitochondria. Nature. 2008;456(7222):605–10. https://doi.org/10.1038/nature07534.
Teng Y, Ren X, Li H, Shull A, Kim J, Cowell JK. Mitochondrial ATAD3A combines with GRP78 to regulate the WASF3 metastasis-promoting protein. Oncogene. 2016;35(3):333–43. https://doi.org/10.1038/onc.2015.86.
•• Rieusset J. Role of endoplasmic reticulum-mitochondria communication in type 2 diabetes. Adv Exp Med Biol. 2017;997:171–86. https://doi.org/10.1007/978-981-10-4567-7_13. This review discusses the role of mitochondria-associated membranes (MAM) in glucose homeostasis.
Thoudam T, Ha C-M, Leem J, Chanda D, Park J-S, Kim H-J, et al. PDK4 augments ER–mitochondria contact to dampen skeletal muscle insulin signaling during obesity. Diabetes. 2019;68(3):571–86. https://doi.org/10.2337/db18-0363.
Arruda AP, Pers BM, Parlakgul G, Guney E, Inouye K, Hotamisligil GS. Chronic enrichment of hepatic endoplasmic reticulum-mitochondria contact leads to mitochondrial dysfunction in obesity. Nat Med. 2014;20(12):1427–35. https://doi.org/10.1038/nm.3735.
Tubbs E, Theurey P, Vial G, Bendridi N, Bravard A, Chauvin M-A, et al. Mitochondria-associated endoplasmic reticulum membrane (MAM) integrity is required for insulin signaling and is implicated in hepatic insulin resistance. Diabetes. 2014;63(10):3279–94. https://doi.org/10.2337/db13-1751.
•• Tubbs E, Chanon S, Robert M, Bendridi N, Bidaux G, Chauvin M-A, et al. Disruption of mitochondria-associated endoplasmic reticulum membrane (MAM) integrity contributes to muscle insulin resistance in mice and humans. Diabetes. 2018;67(4):636–50. https://doi.org/10.2337/db17-0316. This study highlights the importance of mitochondria-associated membranes (MAM) integrity in muscle insulin resistance.
Shinjo S, Jiang S, Nameta M, Suzuki T, Kanai M, Nomura Y, et al. Disruption of the mitochondria-associated ER membrane (MAM) plays a central role in palmitic acid-induced insulin resistance. Exp Cell Res. 2017;359(1):86–93. https://doi.org/10.1016/j.yexcr.2017.08.006.
Thivolet C, Vial G, Cassel R, Rieusset J, Madec AM. Reduction of endoplasmic reticulum- mitochondria interactions in beta cells from patients with type 2 diabetes. PLoS One. 2017;12(7):e0182027. https://doi.org/10.1371/journal.pone.0182027.
Herms A, Bosch M, Reddy BJN, Schieber NL, Fajardo A, Rupérez C, et al. AMPK activation promotes lipid droplet dispersion on detyrosinated microtubules to increase mitochondrial fatty acid oxidation. Nat Commun. 2015;6(1):7176. https://doi.org/10.1038/ncomms8176.
Tarnopolsky MA, Rennie CD, Robertshaw HA, Fedak-Tarnopolsky SN, Devries MC, Hamadeh MJ. Influence of endurance exercise training and sex on intramyocellular lipid and mitochondrial ultrastructure, substrate use, and mitochondrial enzyme activity. Am J Phys Regul Integr Comp Phys. 2007;292(3):R1271–8. https://doi.org/10.1152/ajpregu.00472.2006.
Shubeita GT, Tran SL, Xu J, Vershinin M, Cermelli S, Cotton SL, et al. Consequences of motor copy number on the intracellular transport of kinesin-1-driven lipid droplets. Cell. 2008;135(6):1098–107. https://doi.org/10.1016/j.cell.2008.10.021.
Rambold AS, Cohen S, Lippincott-Schwartz J. Fatty acid trafficking in starved cells: regulation by lipid droplet lipolysis, autophagy, and mitochondrial fusion dynamics. Dev Cell. 2015;32(6):678–92. https://doi.org/10.1016/j.devcel.2015.01.029.
Bischof J, Salzmann M, Streubel MK, Hasek J, Geltinger F, Duschl J, et al. Clearing the outer mitochondrial membrane from harmful proteins via lipid droplets. Cell Death Dis. 2017;3(1):17016. https://doi.org/10.1038/cddiscovery.2017.16.
Nguyen TB, Louie SM, Daniele JR, Tran Q, Dillin A, Zoncu R, et al. DGAT1-dependent lipid droplet biogenesis protects mitochondrial function during starvation-induced autophagy. Dev Cell. 2017;42(1):9–21.e5. https://doi.org/10.1016/j.devcel.2017.06.003.
•• Schuldiner M, Bohnert M. A different kind of love - lipid droplet contact sites. Biochim Biophys Acta Mol Cell Biol Lipids. 2017;1862(10 Pt B):1188–96. https://doi.org/10.1016/j.bbalip.2017.06.005. This review highlights recent findings on the functions of lipid droplet contact sites.
Kory N, Farese RV Jr, Walther TC. Targeting fat: mechanisms of protein localization to lipid droplets. Trends Cell Biol. 2016;26(7):535–46. https://doi.org/10.1016/j.tcb.2016.02.007.
Kimmel AR, Sztalryd C. The perilipins: major cytosolic lipid droplet-associated proteins and their roles in cellular lipid storage, mobilization, and systemic homeostasis. Annu Rev Nutr. 2016;36:471–509. https://doi.org/10.1146/annurev-nutr-071813-105410.
Wang H, Sreenivasan U, Hu H, Saladino A, Polster BM, Lund LM, et al. Perilipin 5, a lipid droplet-associated protein, provides physical and metabolic linkage to mitochondria. J Lipid Res. 2011;52(12):2159–68. https://doi.org/10.1194/jlr.M017939.
Wang H, Sreenivasan U, Gong DW, O’Connell KA, Dabkowski ER, Hecker PA, et al. Cardiomyocyte-specific perilipin 5 overexpression leads to myocardial steatosis and modest cardiac dysfunction. J Lipid Res. 2013;54(4):953–65. https://doi.org/10.1194/jlr.M032466.
Pollak NM, Schweiger M, Jaeger D, Kolb D, Kumari M, Schreiber R, et al. Cardiac-specific overexpression of perilipin 5 provokes severe cardiac steatosis via the formation of a lipolytic barrier. J Lipid Res. 2013;54(4):1092–102. https://doi.org/10.1194/jlr.M034710.
Gemmink A, Daemen S, Kuijpers HJH, Schaart G, Duimel H, Lopez-Iglesias C, et al. Super-resolution microscopy localizes perilipin 5 at lipid droplet-mitochondria interaction sites and at lipid droplets juxtaposing to perilipin 2. Biochim Biophys Acta Mol Cell Biol Lipids. 2018;1863(11):1423–32. https://doi.org/10.1016/j.bbalip.2018.08.016.
Bosma M, Minnaard R, Sparks LM, Schaart G, Losen M, de Baets MH, et al. The lipid droplet coat protein perilipin 5 also localizes to muscle mitochondria. Histochem Cell Biol. 2012;137(2):205–16. https://doi.org/10.1007/s00418-011-0888-x.
Mason RR, Mokhtar R, Matzaris M, Selathurai A, Kowalski GM, Mokbel N, et al. PLIN5 deletion remodels intracellular lipid composition and causes insulin resistance in muscle. Mol Metab. 2014;3(6):652–63. https://doi.org/10.1016/j.molmet.2014.06.002.
Varghese M, Kimler VA, Ghazi FR, Rathore GK, Perkins GA, Ellisman MH, et al. Adipocyte lipolysis affects perilipin 5 and cristae organization at the cardiac lipid droplet-mitochondrial interface. Sci Rep. 2019;9(1):4734. https://doi.org/10.1038/s41598-019-41329-4.
Keenan SN, Meex RC, Lo JCY, Ryan A, Nie S, Montgomery MK, et al. Perilipin 5 deletion in hepatocytes remodels lipid metabolism and causes hepatic insulin resistance in mice. Diabetes. 2019;68(3):543–55. https://doi.org/10.2337/db18-0670.
Mason RR, Watt MJ. Unraveling the roles of PLIN5: linking cell biology to physiology. Trends Endocrinol Metab. 2015;26(3):144–52. https://doi.org/10.1016/j.tem.2015.01.005.
Wang C, Zhao Y, Gao X, Li L, Yuan Y, Liu F, et al. Perilipin 5 improves hepatic lipotoxicity by inhibiting lipolysis. Hepatology. 2015;61(3):870–82. https://doi.org/10.1002/hep.27409.
Gemmink A, Daemen S, Brouwers B, Huntjens PR, Schaart G, Moonen-Kornips E, et al. Dissociation of intramyocellular lipid storage and insulin resistance in trained athletes and type 2 diabetes patients; involvement of perilipin 5? J Physiol. 2018;596(5):857–68. https://doi.org/10.1113/jp275182.
Gemmink A, Bakker LE, Guigas B, Kornips E, Schaart G, Meinders AE, et al. Lipid droplet dynamics and insulin sensitivity upon a 5-day high-fat diet in Caucasians and South Asians. Sci Rep. 2017;7:42393. https://doi.org/10.1038/srep42393.
Coen PM, Hames KC, Leachman EM, Delany JP, Ritov VB, Menshikova EV, et al. Reduced skeletal muscle oxidative capacity and elevated ceramide but not diacylglycerol content in severe obesity. Obesity. 2013;21(11):2362–71. https://doi.org/10.1002/oby.20381.
Gjelstad IMF, Haugen F, Gulseth HL, Norheim F, Jans A, Bakke SS, et al. Expression of perilipins in human skeletal muscle in vitro and in vivo in relation to diet, exercise and energy balance. Arch Physiol Biochem. 2012;118(1):22–30. https://doi.org/10.3109/13813455.2011.630009.
Peters SJ, Samjoo IA, Devries MC, Stevic I, Robertshaw HA, Tarnopolsky MA. Perilipin family (PLIN) proteins in human skeletal muscle: the effect of sex, obesity, and endurance training. Appl Physiol Nutr Metab. 2012;37(4):724–35. https://doi.org/10.1139/H2012-059.
Boutant M, Kulkarni SS, Joffraud M, Ratajczak J, Valera-Alberni M, Combe R, et al. Mfn2 is critical for brown adipose tissue thermogenic function. EMBO J. 2017;36(11):1543–58. https://doi.org/10.15252/embj.201694914.
Young PA, Senkal CE, Suchanek AL, Grevengoed TJ, Lin DD, Zhao L, et al. Long-chain acyl-CoA synthetase 1 interacts with key proteins that activate and direct fatty acids into niche hepatic pathways. J Biol Chem. 2018;293(43):16724–40. https://doi.org/10.1074/jbc.RA118.004049.
Pidoux G, Witczak O, Jarnaess E, Myrvold L, Urlaub H, Stokka AJ, et al. Optic atrophy 1 is an A-kinase anchoring protein on lipid droplets that mediates adrenergic control of lipolysis. EMBO J. 2011;30(21):4371–86. https://doi.org/10.1038/emboj.2011.365.
Yeshaw WM, van der Zwaag M, Pinto F, Lahaye LL, Faber AI, Gomez-Sanchez R, et al. Human VPS13A is associated with multiple organelles and influences mitochondrial morphology and lipid droplet motility. Elife. 2019;8. https://doi.org/10.7554/eLife.43561.
Freyre CAC, Rauher PC, Ejsing CS, Klemm RW. MIGA2 links mitochondria, the ER, and lipid droplets and promotes de novo lipogenesis in adipocytes. Mol Cell. 2019;76(5):811–25.e14. https://doi.org/10.1016/j.molcel.2019.09.011.
Tai ES, Ordovas JM. The role of perilipin in human obesity and insulin resistance. Curr Opin Lipidol. 2007;18(2):152–6. https://doi.org/10.1097/MOL.0b013e328086aeab.
•• Benador IY, Veliova M, Liesa M, Shirihai OS. Mitochondria bound to lipid droplets: where mitochondrial dynamics regulate lipid storage and utilization. Cell Metab. 2018;29(4):827–35. https://doi.org/10.1016/j.cmet.2019.02.011. This review discusses the regulation of mitochondrial tethering to lipid droplets.
•• Valm AM, Cohen S, Legant WR, Melunis J, Hershberg U, Wait E, et al. Applying systems-level spectral imaging and analysis to reveal the organelle interactome. Nature. 2017;546(7656):162–7. https://doi.org/10.1038/nature22369. This is a high-impact study showing a systems-level analysis of the full organelle interactome among six different organelles.
Dolman NJ, Gerasimenko JV, Gerasimenko OV, Voronina SG, Petersen OH, Tepikin AV. Stable Golgi-mitochondria complexes and formation of Golgi Ca(2+) gradients in pancreatic acinar cells. J Biol Chem. 2005;280(16):15794–9. https://doi.org/10.1074/jbc.M412694200.
Wong YC, Kim S, Peng W, Krainc D. Regulation and function of mitochondria–lysosome membrane contact sites in cellular homeostasis. Trends Cell Biol. 2019;29(6):500–13. https://doi.org/10.1016/j.tcb.2019.02.004.
Wong YC, Ysselstein D, Krainc D. Mitochondria-lysosome contacts regulate mitochondrial fission via RAB7 GTP hydrolysis. Nature. 2018;554(7692):382–6. https://doi.org/10.1038/nature25486.
Fransen M, Lismont C, Walton P. The peroxisome-mitochondria connection: how and why? Int J Mol Sci. 2017;18(6). https://doi.org/10.3390/ijms18061126.
Fan J, Li X, Issop L, Culty M, Papadopoulos V. ACBD2/ECI2-mediated peroxisome-mitochondria interactions in Leydig cell steroid biosynthesis. Mol Endocrinol. 2016;30(7):763–82. https://doi.org/10.1210/me.2016-1008.
Komatsu G, Nonomura T, Sasaki M, Ishida Y, Arai S, Miyazaki T. AIM-deficient mouse fed a high-trans fat, high-cholesterol diet: a new animal model for nonalcoholic fatty liver disease. Exp Anim. 2018. https://doi.org/10.1538/expanim.18-0108.
Schrader M, Costello J, Godinho LF, Islinger M. Peroxisome-mitochondria interplay and disease. J Inherit Metab Dis. 2015;38(4):681–702. https://doi.org/10.1007/s10545-015-9819-7.
Acknowledgements
Figures were adapted from SMART Servier Medical Art in accordance with the Creative Commons Attribution 3.0 Unported License.
Funding
MJW and MKM are supported by Research Fellowships from the NHMRC (APP1077703, APP1143224).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Other Forms of Diabetes and Its Complications
Electronic Supplementary Material
ESM 1
(DOCX 23.2 kb).
Rights and permissions
About this article
Cite this article
Keenan, S.N., Watt, M.J. & Montgomery, M.K. Inter-organelle Communication in the Pathogenesis of Mitochondrial Dysfunction and Insulin Resistance. Curr Diab Rep 20, 20 (2020). https://doi.org/10.1007/s11892-020-01300-4
Published:
DOI: https://doi.org/10.1007/s11892-020-01300-4