Abstract
Purpose of Review
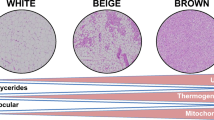
To summarize the state-of-the-art regarding the exercise-regulated endocrine signals that might modulate brown adipose tissue (BAT) activity and/or white adipose tissue (WAT) browning, or through which BAT communicates with other tissues, in humans.
Recent Findings
Exercise induces WAT browning in rodents by means of a variety of physiological mechanism. However, whether exercise induces WAT browning in humans is still unknown. Nonetheless, a number of protein hormones and metabolites, whose signaling can influence thermogenic adipocyte’s metabolism, are secreted during and/or after exercise in humans from a variety of tissues and organs, such as the skeletal muscle, the adipose tissue, the liver, the adrenal glands, or the cardiac muscle.
Summary
Overall, it seems plausible to hypothesize that, in humans, exercise secretes an endocrine cocktail that is likely to induce WAT browning, as it does in rodents. However, even if exercise elicits a pro-browning endocrine response, this might result in a negligible effect if blood flow is restricted in thermogenic adipocyte–rich areas during exercise, which is still to be determined. Future studies are needed to fully characterize the exercise-induced secretion (i.e., to determine the effect of the different exercise frequency, intensity, type, time, and volume) of endocrine signaling molecules that might modulate BAT activity and/or WAT browning or through which BAT communicates with other tissues, during exercise. The exercise effect on BAT metabolism and/or WAT browning could be one of the still unknown mechanisms by which exercise exerts beneficial health effects, and it might be pharmacologically mimicked.

Similar content being viewed by others
References
Cannon B, Nedergaard J. Brown adipose tissue: function and physiological significance. Physiol Rev. 2004;84(1):277–359.
Chang SH, Song NJ, Choi JH, Yun UJ, Park KW. Mechanisms underlying UCP1 dependent and independent adipocyte thermogenesis. Obes Rev. 2019;20(2):241–51.
Petrovic N, Walden TB, Shabalina IG, Timmons JA, Cannon B, Nedergaard J. Chronic peroxisome proliferator-activated receptor gamma (PPARgamma) activation of epididymally derived white adipocyte cultures reveals a population of thermogenically competent, UCP1-containing adipocytes molecularly distinct from classic brown adipocyt. J Biol Chem. 2010;285(10):7153–64.
Betz MJ, Enerbäck S. Targeting thermogenesis in brown fat and muscle to treat obesity and metabolic disease. Nat Rev Endocrinol. 2018;14(2):77–87.
Villarroya F, Cereijo R, Villarroya J, Giralt M. Brown adipose tissue as a secretory organ. Nat Rev Endocrinol. 2017;13(1):26–35.
Lehnig AC, Stanford KI. Exercise-induced adaptations to white and brown adipose tissue. J Exp Biol. 2018;221(Pt Suppl 1).
Riis-Vestergaard MJ, Richelsen B, Bruun JM, Li W, Hansen JB, Pedersen SB. Beta-1 and not beta-3-adrenergic receptors may be the primary regulator of human brown adipocyte metabolism. J Clin Endocrinol Metab. 2019;0954162(478):1–4.
Zouhal H, Jacob C, Delamarche P, Gratas-Delamarche A. Catecholamines and the effects of exercise, training and gender. Sports Med. 2008;38(5):401–23.
Volpe M. Natriuretic peptides and cardio-renal disease. Int J Cardiol. 2014;176(3):630–9.
Lafontan M, Moro C, Berlan M, Crampes F, Sengenes C, Galitzky J. Control of lipolysis by natriuretic peptides and cyclic GMP. Trends Endocrinol Metab. 2008;19(4):130–7.
Engeli S, Birkenfeld AL, Badin PM, Bourlier V, Louche K, Viguerie N, et al. Natriuretic peptides enhance the oxidative capacity of human skeletal muscle. J Clin Invest. 2012;122(12):4675–9.
Bordicchia M, Liu D, Amri EZ, Ailhaud G, Dessì-Fulgheri P, Zhang C, et al. Cardiac natriuretic peptides act via p38 MAPK to induce the brown fat thermogenic program in mouse and human adipocytes. J Clin Invest. 2012;122(3):1022–36.
Liu D, Ceddia RP, Collins S. Cardiac natriuretic peptides promote adipose “browning” through mTOR complex-1. Mol Metab. 2018;9:192–8.
Haufe S, Kaminski J, Utz W, Haas V, Mähler A, Daniels MA, et al. Differential response of the natriuretic peptide system toweight loss and exercise in overweight or obese patients. J Hypertens. 2015;33(7):1458–64.
Moro C, Polak J, Hejnova J, Klimcakova E, Crampes F, Stich V, et al. Atrial natriuretic peptide stimulates lipid mobilization during repeated bouts of endurance exercise. Am J Physiol Endocrinol Metab. 2006;290(5):E864–9.
Peres D, Mourot L, Ménétrier A, Bouhaddi M, Degano B, Regnard J, et al. Intermittent versus constant aerobic exercise in middle-aged males: acute effects on arterial stiffness and factors influencing the changes. Eur J Appl Physiol. 2018;118(8):1625–33.
Huang W-S, Lee M-S, Perng H-W, Yang S-P, Kuo S-W, Chang H-D. Circulating brain natriuretic peptide values in healthy men before and after exercise. Metabolism. 2002;51(11):1423–6.
Ohba H, Takada H, Musha H, Nagashima J, Mori N, Awaya T, et al. Effects of prolonged strenuous exercise on plasma levels of atrial natriuretic peptide and brain natriuretic peptide in healthy men. Am Heart J. 2001;141(5):751–8.
Aengevaeren VL, Hopman MTE, Thijssen DHJ, van Kimmenade RR, de Boer M-J, Eijsvogels TMH. Endurance exercise-induced changes in BNP concentrations in cardiovascular patients versus healthy controls. Int J Cardiol. 2017;227:430–5.
Pathak V, Aris R, Jensen BC, Huang W, Ford HJ. Effect of 6-min walk test on pro-BNP levels in patients with pulmonary arterial hypertension. Lung. 2018;196(3):315–9.
de Oliveira M, Mathias LS, Rodrigues BM, Mariani BG, Graceli JB, De Sibio MT, et al. The roles of triiodothyronine and irisin in improving the lipid profile and directing the browning of human adipose subcutaneous cells. Mol Cell Endocrinol. 2020;506:110744.
Qiu S, Bosnyák E, Treff G, Steinacker JM, Nieß AM, Krüger K, et al. Acute exercise-induced irisin release in healthy adults: associations with training status and exercise mode. Eur J Sport Sci. 2018;18(9):1226–33.
Dünnwald T, Melmer A, Gatterer H, Salzmann K, Ebenbichler C, Burtscher M, et al. Supervised short-term high-intensity training on plasma irisin concentrations in type 2 diabetic patients. Int J Sports Med. 2019;40(3):158–64.
Albrecht E, Norheim F, Thiede B, Holen T, Ohashi T, Schering L, et al. Irisin - a myth rather than an exercise-inducible myokine. Sci Rep. 2015;5:8889.
Hofmann T, Elbelt U, Stengel A. Irisin as a muscle-derived hormone stimulating thermogenesis - a critical update. Peptides. 2014;54:89–100.
Izumiya Y, Bina HA, Ouchi N, Akasaki Y, Kharitonenkov A, Walsh K. FGF21 is an Akt-regulated myokine. FEBS Lett. 2008;582(27):3805–10.
Muise ES, Azzolina B, Kuo DW, El-Sherbeini M, Tan Y, Yuan X, et al. Adipose fibroblast growth factor 21 is up-regulated by peroxisome proliferator-activated receptor and altered metabolic states. Mol Pharmacol. 2008;74(2):403–12.
Hondares E, Gallego-Escuredo JM, Flachs P, Frontini A, Cereijo R, Goday A, et al. Fibroblast growth factor-21 is expressed in neonatal and pheochromocytoma-induced adult human brown adipose tissue. Metabolism. 2014;63(3):312–7.
Fisher FM, Kleiner S, Douris N, Fox EC, Mepani RJ, Verdeguer F, et al. FGF21 regulates PGC-1α and browning of white adipose tissues in adaptive thermogenesis. Genes Dev. 2012;26(3):271–81.
Soundarrajan M, Deng J, Kwasny M, Rubert NC, Nelson PC, El-Seoud DA, et al. Activated brown adipose tissue and its relationship to adiposity and metabolic markers: an exploratory study. Adipocyte. 2020;9(1):87–95.
Slusher AL, Whitehurst M, Zoeller RF, Mock JT, Maharaj M, Huang CJ. Attenuated fibroblast growth factor 21 response to acute aerobic exercise in obese individuals. Nutr Metab Cardiovasc Dis. 2015;25(9):839–45.
Sargeant JA, Aithal GP, Takamura T, Misu H, Takayama H, Douglas JA, et al. The influence of adiposity and acute exercise on circulating hepatokines in normal-weight and overweight/obese men. Appl Physiol Nutr Metab. 2018;43(5):482–90.
Willis SA, Sargeant JA, Thackray AE, Yates T, Stensel DJ, Aithal GP, et al. Effect of exercise intensity on circulating hepatokine concentrations in healthy men. Appl Physiol Nutr Metab. 2019;44(10):1065–72.
Ma Y, Gao M, Sun H, Liu D. Interleukin-6 gene transfer reverses body weight gain and fatty liver in obese mice. Biochim Biophys Acta - Mol Basis Dis. 2015;1852(5):1001–11.
Mauer J, Chaurasia B, Goldau J, Vogt MC, Ruud J, Nguyen KD, et al. Signaling by IL-6 promotes alternative activation of macrophages to limit endotoxemia and obesity-associated resistance to insulin. Nat Immunol. 2014;15(5):423–30.
Stanford KI, Middelbeek RJW, Townsend KL, An D, Nygaard EB, Hitchcox KM, et al. Brown adipose tissue regulates glucose homeostasis and insulin sensitivity. J Clin Invest. 2013;123(1):215–23.
Pedersen BK, Fischer CP. Physiological roles of muscle-derived interleukin-6 in response to exercise. Curr Opin Clin Nutr Metab Care. 2007;10(3):265–71.
Reihmane D, Dela F. Interleukin-6: possible biological roles during exercise. Eur J Sport Sci. 2014;14(3):242–50.
Rao RRR, Long JZZ, White JPP, Svensson KJJ, Lou J, Lokurkar I, et al. Meteorin-like is a hormone that regulates immune-adipose interactions to increase beige fat thermogenesis. Cell. 2014;157(6):1279–91.
Li Z-Y, Zheng S-L, Wang P, Xu T-Y, Guan Y-F, Zhang Y-J, et al. Subfatin is a novel adipokine and unlike Meteorin in adipose and brain expression. CNS Neurosci Ther. 2014;20(4):344–54.
Saghebjoo M, Einaloo A, Mogharnasi M, Ahmadabadi F. The response of meteorin-like hormone and interleukin-4 in overweight women during exercise in temperate, warm and cold water. Horm Mol Biol Clin Investig. 2018;36(3):20180027.
Nishizawa H, Matsuda M, Yamada Y, Kawai K, Suzuki E, Makishima M, et al. Musclin, a novel skeletal muscle-derived secretory factor. J Biol Chem. 2004;279(19):19391–5.
Subbotina E, Sierra A, Zhu Z, Gao Z, Koganti SRK, Reyes S, et al. Musclin is an activity-stimulated myokine that enhances physical endurance. Proc Natl Acad Sci U S A. 2015;112(52):16042–7.
Jeremic N, Chaturvedi P, Tyagi SC. Browning of White fat: novel insight into factors, mechanisms, and therapeutics. J Cell Physiol. 2017;232(1):61–8.
Morris A. Advances in GDF15 research. Nat Rev Endocrinol. 2020;16(3):129.
Laurens C, Parmar A, Murphy E, Carper D, Lair B, Maes P, et al. Growth and differentiation factor 15 is secreted by skeletal muscle during exercise and promotes lipolysis in humans. JCI insight. 2020;5(6):e131870.
Campderrós L, Moure R, Cairó M, Gavaldà-Navarro A, Quesada-López T, Cereijo R, et al. Brown adipocytes secrete GDF15 in response to thermogenic activation. Obesity (Silver Spring). 2019;27(10):1606–16.
Kleinert M, Clemmensen C, Sjøberg KA, Carl CS, Jeppesen JF, Wojtaszewski JFP, et al. Exercise increases circulating GDF15 in humans. Mol Metab. 2018;9:187–91.
Galliera E, Lombardi G, Marazzi MG, Grasso D, Vianello E, Pozzoni R, et al. Acute exercise in elite rugby players increases the circulating level of the cardiovascular biomarker GDF-15. Scand J Clin Lab Invest. 2014;74(6):492–9.
McPherron AC, Lawler AM, Lee S-J. Regulation of skeletal muscle mass in mice by a new TGF-p superfamily member. Nature. 1997;387(6628):83–90.
Schuelke M, Wagner KR, Stolz LE, Hübner C, Riebel T, Kömen W, et al. Myostatin mutation associated with gross muscle hypertrophy in a child. N Engl J Med. 2004;350(26):2682–8.
McPherron AC, Lee S-J. Suppression of body fat accumulation in myostatin-deficient mice. J Clin Invest. 2002;109(5):595–601.
Zhang C, McFarlane C, Lokireddy S, Masuda S, Ge X, Gluckman PD, et al. Inhibition of myostatin protects against diet-induced obesity by enhancing fatty acid oxidation and promoting a brown adipose phenotype in mice. Diabetologia. 2012;55(1):183–93.
Shan T, Liang X, Bi P, Kuang S. Myostatin knockout drives browning of white adipose tissue through activating the AMPK-PGC1α-Fndc5 pathway in muscle. FASEB J. 2013;27(5):1981–9.
Kong X, Yao T, Zhou P, Kazak L, Tenen D, Lyubetskaya A, et al. Brown adipose tissue controls skeletal muscle function via the secretion of myostatin. Cell Metab. 2018;28(4):631–43.
Kabak B, Belviranli M, Okudan N. Irisin and myostatin responses to acute high-intensity interval exercise in humans. Horm Mol Biol Clin Investig. 2018;35(3):20180008.
Kazemi F. The correlation of resistance exercise-induced myostatin with insulin resistance and plasma cytokines in healthy young men. J Endocrinol Investig. 2016;39(4):383–8.
Saremi A, Gharakhanloo R, Sharghi S, Gharaati MR, Larijani B, Omidfar K. Effects of oral creatine and resistance training on serum myostatin and GASP-1. Mol Cell Endocrinol. 2010;317(1–2):25–30.
Paoli A, Pacelli QF, Neri M, Toniolo L, Cancellara P, Canato M, et al. Protein supplementation increases postexercise plasma myostatin concentration after 8 weeks of resistance training in young physically active subjects. J Med Food. 2015;18(1):137–43.
Bagheri R, Moghadam BH, Church DD, Tinsley GM, Eskandari M, Moghadam BH, et al. The effects of concurrent training order on body composition and serum concentrations of follistatin, myostatin and GDF11 in sarcopenic elderly men. Exp Gerontol. 2020;133:110869.
Singh R, Braga M, Reddy STT, Lee SJS-J, Parveen M, Grijalva V, et al. Follistatin targets distinct pathways to promote brown adipocyte characteristics in brown and white adipose tissues. Endocrinology. 2017;158(5):1217–30.
Perakakis N, Mougios V, Fatouros I, Siopi A, Draganidis D, Peradze N, et al. Physiology of activins/follistatins: associations with metabolic and anthropometric variables and response to exercise. J Clin Endocrinol Metab. 2018;103(10):3890–9.
Li J-X, Cummins CL. Getting the skinny on follistatin and fat. Endocrinology. 2017;158(5):1109–12.
Hansen JS, Pedersen BK, Xu G, Lehmann R, Weigert C, Plomgaard P. Exercise-induced secretion of FGF21 and follistatin are blocked by pancreatic clamp and impaired in type 2 diabetes. J Clin Endocrinol Metab. 2016;101(7):2816–25.
Ouchi N, Oshima Y, Ohashi K, Higuchi A, Ikegami C, Izumiya Y, et al. Follistatin-like 1, a secreted muscle protein, promotes endothelial cell function and revascularization in ischemic tissue through a nitric-oxide synthase-dependent mechanism. J Biol Chem. 2008;283(47):32802–11.
Görgens SW, Raschke S, Holven KB, Jensen J, Eckardt K, Eckel J. Regulation of follistatin-like protein 1 expression and secretion in primary human skeletal muscle cells. Arch Physiol Biochem. 2013;119(2):75–80.
Fang D, Shi X, Lu T, Ruan H, Gao Y. The glycoprotein follistatin-like 1 promotes brown adipose thermogenesis. Metabolism. 2019;98:16–26.
Kon M, Ebi Y, Nakagaki K. Effects of acute sprint interval exercise on follistatin-like 1 and apelin secretions. Arch Physiol Biochem. 2019; :1–5.
Tapia-Arancibia L, Rage F, Givalois L, Arancibia S. Physiology of BDNF: focus on hypothalamic function. Front Neuroendocrinol. 2004;25(2):77–107.
Stanford KI, Goodyear LJ. Exercise regulation of adipose tissue. Adipocyte. 2016;5(2):153–62.
Cao L, Choi EY, Liu X, Martin A, Wang C, Xu X, et al. White to brown fat phenotypic switch induced by genetic and environmental activation of a hypothalamic-adipocyte axis. Cell Metab. 2011;14(3):324–38.
Wrann CD, White JP, Salogiannnis J, Laznik-Bogoslavski D, Wu J, Ma D, et al. Exercise induces hippocampal BDNF through a PGC-1α/FNDC5 pathway. Cell Metab. 2013;18(5):649–59.
Hung C-L, Tseng J-W, Chao H-H, Hung T-M, Wang H-S. Effect of acute exercise mode on serum brain-derived neurotrophic factor (BDNF) and task switching performance. J Clin Med. 2018;7(10):301.
Simão AP, Mendonça VA, Avelar NCP, da Fonseca SF, Santos JM, de Oliveira ACC, et al. Whole body vibration training on muscle strength and brain-derived neurotrophic factor levels in elderly woman with knee osteoarthritis: a randomized clinical trial study. Front Physiol. 2019;10:756.
Marinus N, Hansen D, Feys P, Meesen R, Timmermans A, Spildooren J. The impact of different types of exercise training on peripheral blood brain-derived neurotrophic factor concentrations in older adults: a meta-analysis. Sports Med. 2019;49(10):1529–46.
Devenney KE, Guinan EM, Kelly ÁM, Mota BC, Walsh C, Olde Rikkert M, et al. Acute high-intensity aerobic exercise affects brain-derived neurotrophic factor in mild cognitive impairment: a randomised controlled study. BMJ Open Sport Exerc Med. 2019;5(1):e000499.
Goekint M, De Pauw K, Roelands B, Njemini R, Bautmans I, Mets T, et al. Strength training does not influence serum brain-derived neurotrophic factor. Eur J Appl Physiol. 2010;110(2):285–93.
Correia PR, Pansani A, MacHado F, Andrade M, da Silva AC, Scorza FA, et al. Acute strength exercise and the involvement of small or large muscle mass on plasma brain-derived neurotrophic factor levels. Clinics. 2010;65(11):1123–6.
Woodward L, Akoumianakis I, Antoniades C. Unravelling the adiponectin paradox: novel roles of adiponectin in the regulation of cardiovascular disease. Br J Pharmacol. 2017;174(22):4007–20.
Hui X, Gu P, Zhang J, Nie T, Pan Y, Wu D, et al. Adiponectin enhances cold-induced browning of subcutaneous adipose tissue via promoting M2 macrophage proliferation. Cell Metab. 2015;22(2):279–90.
Sun L, Yan J, Goh HJ, Govindharajulu P, Verma S, Michael N, et al. Fibroblast growth factor-21, leptin, and adiponectin responses to acute cold-induced brown adipose tissue activation. J Clin Endocrinol Metab. 2020;105(3).
Kraemer RR, Aboudehen KS, Carruth AK, Durand RJ, Acevedo EO, Hebert EP, et al. Adiponectin responses to continuous and progressively intense intermittent exercise. Med Sci Sports Exerc. 2003;35(8):1320–5.
Ferguson MA, White LJ, McCoy S, Kim HW, Petty T, Wilsey J. Plasma adiponectin response to acute exercise in healthy subjects. Eur J Appl Physiol. 2004;91(2–3):324–9.
Punyadeera C, Zorenc AHG, Koopman R, McAinch AJ, Smit E, Manders R, et al. The effects of exercise and adipose tissue lipolysis on plasma adiponectin concentration and adiponectin receptor expression in human skeletal muscle. Eur J Endocrinol. 2005;152(3):427–36.
Jamurtas AZ, Theocharis V, Koukoulis G, Stakias N, Fatouros IG, Kouretas D, et al. The effects of acute exercise on serum adiponectin and resistin levels and their relation to insulin sensitivity in overweight males. Eur J Appl Physiol. 2006;97(1):122–6.
Jürimäe J, Hofmann P, Jürimäe T, Mäestu J, Purge P, Wonisch M, et al. Plasma adiponectin response to sculling exercise at individual anaerobic threshold in college level male rowers. Int J Sports Med. 2006;27(4):272–7.
Jürimäe J, Purge P, Jürimäe T. Adiponectin is altered after maximal exercise in highly trained male rowers. Eur J Appl Physiol. 2005;93(4):502–5.
Jürimäe J, Purge P, Jürimäe T. Adiponectin and stress hormone responses to maximal sculling after volume-extended training season in elite rowers. Metabolism. 2006;55(1):13–9.
Racil G, Ben Ounis O, Hammouda O, Kallel A, Zouhal H, Chamari K, et al. Effects of high vs. moderate exercise intensity during interval training on lipids and adiponectin levels in obese young females. Eur J Appl Physiol. 2013;113(10):2531–40.
Maffei M, Halaas J, Ravussin E, Pratley RE, Lee GH, Zhang Y, et al. Leptin levels in human and rodent: measurement of plasma leptin and ob RNA in obese and weight-reduced subjects. Nat Med. 1995;1(11):1155–61.
Kuryszko J, Sławuta P, Sapikowski G. Secretory function of adipose tissue. Pol J Vet Sci. 2016;19(2):441–6.
Enriori PJ, Sinnayah P, Simonds SE, Garcia Rudaz C, Cowley MA. Leptin action in the dorsomedial hypothalamus increases sympathetic tone to brown adipose tissue in spite of systemic leptin resistance. J Neurosci. 2011;31(34):12189–97.
Kotzbeck P, Giordano A, Mondini E, Murano I, Severi I, Venema W, et al. Brown adipose tissue whitening leads to brown adipocyte death and adipose tissue inflammation. J Lipid Res. 2018;59(5):784–94.
Rodríguez A, Becerril S, Méndez-Giménez L, Ramírez B, Sáinz N, Catalán V, et al. Leptin administration activates irisin-induced myogenesis via nitric oxide-dependent mechanisms, but reduces its effect on subcutaneous fat browning in mice. Int J Obes. 2015;39(3):397–407.
Desgorces FD, Chennaoui M, Gomez-Merino D, Drogou C, Bonneau D, Guezennec CY. Leptin, catecholamines and free fatty acids related to reduced recovery delays after training. Eur J Appl Physiol. 2004;93(1–2):153–8.
Olive JL, Miller GD. Differential effects of maximal- and moderate-intensity runs on plasma leptin in healthy trained subjects. Nutrition. 2001;17(5):365–9.
Zaccaria M, Ermolao A, Roi GS, Englaro P, Tegon G, Varnier M. Leptin reduction after endurance races differing in duration and energy expenditure. Eur J Appl Physiol. 2002;87(2):108–11.
Legakis IN, Mantzouridis T, Saramantis A, Lakka-Papadodima E. Rapid decrease of leptin in middle-aged sedentary individuals after 20 minutes of vigorous exercise with early recovery after the termination of the test. J Endocrinol Investig. 2004;27(2):117–20.
Park KM, Park SC, Kang S. Effects of resistance exercise on adipokine factors and body composition in pre- and postmenopausal women. J Exerc Rehabil. 2019;15(5):676–82.
Salvadori A, Fanari P, Brunani A, Marzullo P, Codecasa F, Tovaglieri I, et al. Leptin level lowers in proportion to the amount of aerobic work after four weeks of training in obesity. Horm Metab Res. 2015;47(3):225–31.
Klagsbrun M, D’Amore PA. Vascular endothelial growth factor and its receptors. Cytokine Growth Factor Rev. 1996;7(3):259–70.
Sun K, Kusminski CM, Luby-Phelps K, Spurgin SB, An YA, Wang QA, et al. Brown adipose tissue derived VEGF-A modulates cold tolerance and energy expenditure. Mol Metab. 2014;3(4):474–83.
Kraus RM, Stallings HW, Yeager RC, Gavin TP. Circulating plasma VEGF response to exercise in sedentary and endurance-trained men. J Appl Physiol. 2004;96(4):1445–50.
Jürimäe J, Vaiksaar S, Purge P. Circulating inflammatory cytokine responses to endurance exercise in female rowers. Int J Sports Med. 2018;39(14):1041–8.
Ribeiro F, Ribeiro IP, Gonçalves AC, Alves AJ, Melo E, Fernandes R, et al. Effects of resistance exercise on endothelial progenitor cell mobilization in women. Sci Rep. 2017;7(1):17880.
Landers-Ramos RQ, Jenkins NT, Spangenburg EE, Hagberg JM, Prior SJ. Circulating angiogenic and inflammatory cytokine responses to acute aerobic exercise in trained and sedentary young men. Eur J Appl Physiol. 2014;114(7):1377–84.
Jürimäe J, Tillmann V, Purge P, Jürimäe T. Acute inflammatory response to prolonged sculling in competitive male rowers. J Sports Med Phys Fitness. 2016;56(11):1368–75.
Larkin KA, MacNeil RG, Dirain M, Sandesara B, Manini TM, Buford TW. Blood flow restriction enhances post-resistance exercise angiogenic gene expression. Med Sci Sports Exerc. 2012;44(11):2077–83.
Dijk W, Kersten S. Regulation of lipid metabolism by angiopoietin-like proteins. Curr Opin Lipidol. 2016;27(3):249–56.
Yu J, Zheng J, Liu XF, Feng ZL, Zhang XP, Cao LL, et al. Exercise improved lipid metabolism and insulin sensitivity in rats fed a high-fat diet by regulating glucose transporter 4 (GLUT4) and musclin expression. Brazilian J Med Biol Res. 2016;49(5):e5129.
Catoire M, Alex S, Paraskevopulos N, Mattijssen F, Evers-van Gogh I, Schaart G, et al. Fatty acid-inducible ANGPTL4 governs lipid metabolic response to exercise. Proc Natl Acad Sci U S A. 2014;111(11):E1043–52.
Ingerslev B, Hansen JS, Hoffmann C, Clemmesen JO, Secher NH, Scheler M, et al. Angiopoietin-like protein 4 is an exercise-induced hepatokine in humans, regulated by glucagon and cAMP. Mol Metab. 2017;6(10):1286–95.
Kersten S, Lichtenstein L, Steenbergen E, Mudde K, Hendriks HFJ, Hesselink MK, et al. Caloric restriction and exercise increase plasma ANGPTL4 levels in humans via elevated free fatty acids. Arterioscler Thromb Vasc Biol. 2009;29(6):969–74.
Górecka M, Krzemiński K, Buraczewska M, Kozacz A, Dąbrowski J, Ziemba AW. Effect of mountain ultra-marathon running on plasma angiopoietin-like protein 4 and lipid profile in healthy trained men. Eur J Appl Physiol. 2020;120(1):117–25.
Shimomura Y, Honda T, Shiraki M, Murakami T, Sato J, Kobayashi H, et al. Branched-chain amino acid catabolism in exercise and liver disease. J Nutr. 2018;136:250S–3S.
Roberts LD, Boström P, O’Sullivan JF, Schinzel RT, Lewis GD, Dejam A, et al. β-Aminoisobutyric acid induces browning of white fat and hepatic β-oxidation and is inversely correlated with cardiometabolic risk factors. Cell Metab. 2014;19(1):96–108.
Stautemas J, Van Kuilenburg ABP, Stroomer L, Vaz F, Blancquaert L, Lefevere FBD, et al. Acute aerobic exercise leads to increased plasma levels of R- and S-β-aminoisobutyric acid in humans. Front Physiol. 2019; 10 (SEP) :1240.
Morales FE, Forsse JS, Andre TL, McKinley-Barnard SK, Hwang PS, Anthony IG, et al. BAIBA does not regulate UCP-3 expression in human skeletal muscle as a response to aerobic exercise. J Am Coll Nutr. 2017;36(3):200–9.
Short KR, Chadwick JQ, Teague AM, Tullier MA, Wolbert L, Coleman C, et al. Effect of obesity and exercise training on plasma amino acids and amino metabolites in American Indian adolescents. J Clin Endocrinol Metab. 2019;104(8):3249–61.
Kristensen M, Albertsen J, Rentsch M, Juel C. Lactate and force production in skeletal muscle. J Physiol. 2005;562(2):521–6.
De Matteis R, Lucertini F, Guescini M, Polidori E, Zeppa S, Stocchi V, et al. Exercise as a new physiological stimulus for brown adipose tissue activity. Nutr Metab Cardiovasc Dis. 2013;23(6):582–90.
Carrière A, Jeanson Y, Berger-Müller S, André M, Chenouard V, Arnaud E, et al. Browning of white adipose cells by intermediate metabolites: an adaptive mechanism to alleviate redox pressure. Diabetes. 2014;63(10):3253–65.
Jeanson Y, Ribas F, Galinier A, Arnaud E, Ducos M, André M, et al. Lactate induces FGF21 expression in adipocytes through a p38-MAPK pathway. Biochem J. 2016;473(6):685–92.
Schranner D, Kastenmüller G, Schönfelder M, Römisch-Margl W, Wackerhage H. Metabolite concentration changes in humans after a bout of exercise: a systematic review of exercise metabolomics studies. Sport Med - open. 2020;6(1):11.
Evans M, Cogan KE, Egan B. Metabolism of ketone bodies during exercise and training: physiological basis for exogenous supplementation. J Physiol. 2017;595(9):2857–71.
Wang W, Ishibashi J, Trefely S, Shao M, Cowan AJ, Sakers A, et al. A PRDM16-driven metabolic signal from adipocytes regulates precursor cell fate. Cell Metab. 2019; 30 (1) :174–189.e5.
Srivastava S, Baxa U, Niu G, Chen X, Veech RL. A ketogenic diet increases brown adipose tissue mitochondrial proteins and UCP1 levels in mice. IUBMB Life. 2013;65(1):58–66.
de Oliveira CR, Andreotti S, Komino ACM, de Fatima SF, Sertié RAL, Christoffolete MA, et al. Physiological concentrations of β-hydroxybutyrate do not promote adipocyte browning. Life Sci. 2019;232:116683.
Margolis LM, O’Fallon KS. Utility of ketone supplementation to enhance physical performance: a systematic review. Adv Nutr. 2019;11(2):412–9.
Lynes MD, Leiria LO, Lundh M, Bartelt A, Shamsi F, Huang TL, et al. The cold-induced lipokine 12,13-diHOME promotes fatty acid transport into brown adipose tissue. Nat Med. 2017;23(5):631–7.
Stanford KI, Lynes MD, Takahashi H, Baer LA, Arts PJ, May FJ, et al. 12,13-diHOME: an exercise-induced lipokine that increases skeletal muscle fatty acid uptake. Cell Metab. 2018;27(5):1111–1120.e3.
Nieman DC, Shanely RA, Luo B, Meaney MP, Dew DA, Pappan KL. Metabolomics approach to assessing plasma 13- and 9-hydroxy-octadecadienoic acid and linoleic acid metabolite responses to 75-km cycling. Am J Physiol - Regul Integr Comp Physiol. 2014;307(1):68–74.
Acosta FM, Martinez-Tellez B, Sanchez-Delgado G, Migueles JH, Contreras-Gomez MA, Martinez-Avila WD, et al. Association of objectively measured physical activity with brown adipose tissue volume and activity in young adults. J Clin Endocrinol Metab. 2018;104(2):223–33.
Martinez-Tellez B, Sanchez-Delgado G, Amaro-Gahete FJ, Acosta FM, Ruiz JR. Relationships between cardiorespiratory fitness/muscular strength and 18F-fluorodeoxyglucose uptake in brown adipose tissue after exposure to cold in young, sedentary adults. Sci Rep. 2019;9(1):11314.
Dinas PC, Nikaki A, Jamurtas AZ, Prassopoulos V, Efthymiadou R, Koutedakis Y, et al. Association between habitual physical activity and brown adipose tissue activity in individuals undergoing PET-CT scantle. Clin Endocrinol. 2015;82(1):147–54.
Dinas PC, Valente A, Granzotto M, Rossato M, Vettor R, Zacharopoulou A, et al. Browning formation markers of subcutaneous adipose tissue in relation to resting energy expenditure, physical activity and diet in humans. Horm Mol Biol Clin Investig. 2017; 31 (1).
Vosselman MJ, Hoeks J, Brans B, Pallubinsky H, Nascimento EBM, Van Der Lans AAJJ, et al. Low brown adipose tissue activity in endurance-trained compared with lean sedentary men. Int J Obes. 2015;39(12):1696–702.
Singhal V, Maffazioli GD, Ackerman KE, Lee H, Elia EF, Woolley R, et al. Effect of chronic athletic activity on brown fat in young women. PLoS One. 2016;11(5):e0156353.
Trexler ET, McCallister D, Smith-Ryan AE, Branca RT. Incidental finding of low brown adipose tissue activity in endurance-trained individuals: methodological considerations for positron emission tomography. J Nat Sci. 2017;3(3):e335.
Motiani P, Virtanen KA, Motiani KK, Eskelinen JJ, Middelbeek RJ, Goodyear LJ, et al. Decreased insulin-stimulated brown adipose tissue glucose uptake after short-term exercise training in healthy middle-aged men. Diabetes Obes Metab. 2017;19(10):1379–88.
Norheim F, Langleite TM, Hjorth M, Holen T, Kielland A, Stadheim HK, et al. The effects of acute and chronic exercise on PGC-1α, irisin and browning of subcutaneous adipose tissue in humans. FEBS J. 2014;281(3):739–49.
Tsiloulis T, Carey AL, Bayliss J, Canny B, Meex RCR, Watt MJ. No evidence of white adipocyte browning after endurance exercise training in obese men. Int J Obes. 2018;42(4):721–7.
Martinez-Tellez B, Xu H, Sanchez-Delgado G, Acosta FM, Rensen PCN, Llamas-Elvira JM, et al. Association of wrist and ambient temperature with cold-induced brown adipose tissue and skeletal muscle [18F]FDG uptake in young adults. Am J Physiol Regul Integr Comp Physiol. 2018;315(6):R1281–8.
Carpentier AC, Blondin DP, Virtanen KA, Richard D, Haman F, Turcotte ÉE. Brown adipose tissue energy metabolism in humans. Front Endocrinol (Lausanne). 2018; 9 :447.
Blondin DP, Labbé SM, Noll C, Kunach M, Phoenix S, Guérin B, et al. Selective impairment of glucose but not fatty acid or oxidative metabolism in brown adipose tissue of subjects with type 2 diabetes. Diabetes. 2015;64(7):2388–97.
Cypess AM, White AP, Vernochet C, Schulz TJ, Xue R, Sass CA, et al. Anatomical localization, gene expression profiling and functional characterization of adult human neck brown fat. Nat Med. 2013;19(5):635–9.
Mittendorfer B, Fields DA, Klein S. Excess body fat in men decreases plasma fatty acid availability and oxidation during endurance exercise. Am J Physiol - Endocrinol Metab. 2004;286(3):E354–62.
Fenzl M, Schnizer W, Aebli N, Schlegel C, Villiger B, Disch A, et al. Release of ANP and fat oxidation in overweight persons during aerobic exercise in water. Int J Sport Med. 2013;34(9):795–9.
Bloomer RJ, Canale RE, Shastri S, Suvarnapathki S. Effect of oral intake of capsaicinoid beadlets on catecholamine secretion and blood markers of lipolysis in healthy adults: a randomized, placebo controlled, double-blind, cross-over study. Lipids Health Dis. 2010;9:72.
Onus K, Cannon J, Liberts L, Marino FE. Acute effects of a dopamine/norepinephrine reuptake inhibitor on neuromuscular performance following self-paced exercise in cool and hot environments. J Therm Biol. 2016;60:60–9.
Skriver K, Roig M, Lundbye-Jensen J, Pingel J, Helge JW, Kiens B, et al. Acute exercise improves motor memory: exploring potential biomarkers. Neurobiol Learn Mem. 2014;116:46–58.
Goto C, Nishioka K, Umemura T, Jitsuiki D, Sakagutchi A, Kawamura M, et al. Acute moderate-intensity exercise induces vasodilation through an increase in nitric oxide bioavailiability in humans. Am J Hypertens. 2007;20(8):825–30.
Ceresini G, Marchini L, Fabbo A, Freddi M, Pasolini G, Reali N, et al. Evaluation of circulating galanin levels after exercise-induced pituitary hormone secretion in man. Metabolism. 1997;46(3):282–6.
Kliszczewicz BM, Esco MR, Quindry JC, Blessing DL, Oliver GD, Taylor KJ, et al. Autonomic responses to an acute bout of high-intensity body weight resistance exercise vs. treadmill running. J strength Cond Res. 2016;30(4):1050–8.
Kraemer WJ, Gordon SE, Fragala MS, Bush JA, Szivak TK, Flanagan SD, et al. The effects of exercise training programs on plasma concentrations of proenkephalin peptide F and catecholamines. Peptides. 2015;64:74–81.
Turner D, Gray BJ, Luzio S, Dunseath G, Bain SC, Hanley S, et al. Similar magnitude of post-exercise hyperglycemia despite manipulating resistance exercise intensity in type 1 diabetes individuals. Scand J Med Sci Sports. 2016;26(4):404–12.
Shimizu R, Hotta K, Yamamoto S, Matsumoto T, Kamiya K, Kato M, et al. Low-intensity resistance training with blood flow restriction improves vascular endothelial function and peripheral blood circulation in healthy elderly people. Eur J Appl Physiol. 2016;116(4):749–57.
Rubin DA, Castner DM, Pham H, Ng J, Adams E, Judelson DA. Hormonal and metabolic responses to a resistance exercise protocol in lean children, obese children and lean adults. Pediatr Exerc Sci. 2014;26(4):444–54.
Turner D, Luzio S, Gray BJ, Dunseath G, Rees ED, Kilduff LP, et al. Impact of single and multiple sets of resistance exercise in type 1 diabetes. Scand J Med Sci Sports. 2015;25(1):e99–109.
Koppo K, Larrouy D, Marques MA, Berlan M, Bajzova M, Polak J, et al. Lipid mobilization in subcutaneous adipose tissue during exercise in lean and obese humans. Roles of insulin and natriuretic peptides. Am J Physiol - Endocrinol Metab. 2010;299(2):E258–65.
MacDonald JR, MacDougall JD, Interisano SA, Smith KM, McCartney N, Moroz JS, et al. Hypotension following mild bouts of resistance exercise and submaximal dynamic exercise. Eur J Appl Physiol Occup Physiol. 1999;79(2):148–54.
Poveda JJ, Berrazueta JR, Ochoteco A, Montalbán C, García-Unzueta MT, Fernández C, et al. Age-related responses of vasoactive factors during acute exercise. Horm Metab Res. 1998;30(11):668–72.
Poveda JJ, Riestra A, Salas E, Cagigas ML, López-Somoza C, Amado JA, et al. Contribution of nitric oxide to exercise-induced changes in healthy volunteers: effects of acute exercise and long-term physical training. Eur J Clin Investig. 1997;27(11):967–71.
He Z, Tian Y, Valenzuela PL, Huang C, Zhao J, Hong P, et al. Myokine/adipokine response to “aerobic” exercise: is it just a matter of exercise load? Front Physiol. 2019;10(691).
Ozbay S, Ulupınar S, Şebin E, Altınkaynak K. Acute and chronic effects of aerobic exercise on serum irisin, adropin, and cholesterol levels in the winter season: indoor training versus outdoor training. Chin J Physiol. 2020;63(1):21–6.
Daskalopoulou SS, Cooke AB, Gomez YH, Mutter AF, Filippaios A, Mesfum ET, et al. Plasma irisin levels progressively increase in response to increasing exercise workloads in young, healthy, active subjects. Eur J Endocrinol. 2014;171(3):343–52.
Rojas Vega S, Kleinert J, Sulprizio M, Hollmann W, Bloch W, Strüder HK. Responses of serum neurotrophic factors to exercise in pregnant and postpartum women. Psychoneuroendocrinology. 2011;36(2):220–7.
Wiecek M, Szymura J, Maciejczyk M, Kantorowicz M, Szygula Z. Acute anaerobic exercise affects the secretion of asprosin, irisin, and other cytokines - a comparison between sexes. Front Physiol. 2018;9:1782.
Philippou A, Maridaki M, Tenta R, Koutsilieris M. Hormonal responses following eccentric exercise in humans. Hormones. 2017;16(4):402–13.
Blizzard Leblanc DR, Rioux B V., Pelech C, Moffatt TL, Kimber DE, Duhamel TA, et al. Exercise-induced irisin release as a determinant of the metabolic response to exercise training in obese youth: the exit trial. Physiol Rep. 2017; 5 (23).
Tsuchiya Y, Ando D, Takamatsu K, Goto K. Resistance exercise induces a greater irisin response than endurance exercise. Metabolism. 2015;64(9):1042–50.
Morville T, Sahl RE, Trammell SA, Svenningsen JS, Gillum MP, Helge JW, et al. Divergent effects of resistance and endurance exercise on plasma bile acids, FGF19, and FGF21 in humans. JCI insight. 2018;3(15):122737.
JanssenDuijghuijsen LM, Keijer J, Mensink M, Lenaerts K, Ridder L, Nierkens S, et al. Adaptation of exercise-induced stress in well-trained healthy young men. Exp Physiol. 2017;102(1):86–99.
Taniguchi H, Tanisawa K, Sun X, Higuchi M. Acute endurance exercise lowers serum fibroblast growth factor 21 levels in Japanese men. Clin Endocrinol. 2016;85(6):861–7.
Kim KH, Kim SH, Min Y-K, Yang H-M, Lee J-B, Lee M-S. Acute exercise induces FGF21 expression in mice and in healthy humans. PLoS One. 2013;8(5):e63517.
Parmar B, Lewis JE, Samms RJ, Ebling FJPP, Cheng CC, Adams AC, et al. Eccentric exercise increases circulating fibroblast activation protein α but not bioactive fibroblast growth factor 21 in healthy humans. Exp Physiol. 2018;103(6):876–83.
Marques CG, Santos VC, Levada-Pires AC, Jacintho TM, Gorjão R, Pithon-Curi TC, et al. Effects of DHA-rich fish oil supplementation on the lipid profile, markers of muscle damage, and neutrophil function in wheelchair basketball athletes before and after acute exercise. Appl Physiol Nutr Metab. 2015;40(6):596–604.
Lau KK, Obeid J, Breithaupt P, Belostotsky V, Arora S, Nguyen T, et al. Effects of acute exercise on markers of inflammation in pediatric chronic kidney disease: a pilot study. Pediatr Nephrol. 2015;30(4):615–21.
Viana JL, Kosmadakis GC, Watson EL, Bevington A, Feehally J, Bishop NC, et al. Evidence for anti-inflammatory effects of exercise in CKD. J Am Soc Nephrol. 2014;25(9):2121–30.
Islam H, Townsend LK, McKie GL, Medeiros PJ, Gurd BJ, Hazell TJ. Potential involvement of lactate and interleukin-6 in the appetite-regulatory hormonal response to an acute exercise bout. J Appl Physiol. 2017;123(3):614–23.
Sabaratnam R, Pedersen AJTT, Kristensen JM, Handberg A, Wojtaszewski JFPP, Højlund K. Intact regulation of muscle expression and circulating levels of myokines in response to exercise in patients with type 2 diabetes. Physiol Rep. 2018;6(12):e13723.
Mendham AE, Donges CE, Liberts EA, Duffield R. Effects of mode and intensity on the acute exercise-induced IL-6 and CRP responses in a sedentary, overweight population. Eur J Appl Physiol. 2011;111(6):1035–45.
Harris RA, Padilla J, Hanlon KP, Rink LD, Wallace JP. The flow-mediated dilation response to acute exercise in overweight active and inactive men. Obesity (Silver Spring). 2008;16(3):578–84.
Tajra V, Tibana RA, Vieira DCL, de Farias DL, Teixeira TG, Funghetto SS, et al. Identification of high responders for interleukin-6 and creatine kinase following acute eccentric resistance exercise in elderly obese women. J Sci Med Sport. 2014;17(6):662–6.
Jackman JS, Bell PG, Gill S, van Someren K, Davison GW, Cockburn E. Assessing the usefulness of acute physiological responses following resistance exercise: sensitivity, magnitude of change, and time course of measures. Appl Physiol Nutr Metab. 2019;44(3):309–19.
Hasenoehrl T, Wessner B, Tschan H, Vidotto C, Crevenna R, Csapo R. Eccentric resistance training intensity may affect the severity of exercise induced muscle damage. J Sports Med Phys Fitness. 2017;57(9):1195–204.
Turner D, Luzio S, Kilduff LP, Gray BJ, Dunseath G, Bain SC, et al. Reductions in resistance exercise-induced hyperglycaemic episodes are associated with circulating interleukin-6 in type 1 diabetes. Diabet Med. 2014;31(8):1009–13.
Han DS, Hsiao MY, Wang TG, Chen SY, Yang WS. Association of serum myokines and aerobic exercise training in patients with spinal cord injury: An observational study. BMC Neurol. 2016;16(1):142.
Gustafsson G, Lira CM, Johansson J, Wisén A, Wohlfart B, Ekman R, et al. The acute response of plasma brain-derived neurotrophic factor as a result of exercise in major depressive disorder. Psychiatry Res. 2009;169(3):244–8.
Bos I, Jacobs L, Nawrot TS, de Geus B, Torfs R, Int Panis L, et al. No exercise-induced increase in serum BDNF after cycling near a major traffic road. Neurosci Lett. 2011;500(2):129–32.
Seifert T, Brassard P, Wissenberg M, Rasmussen P, Nordby P, Stallknecht B, et al. Endurance training enhances BDNF release from the human brain. Am J Physiol Regul Integr Comp Physiol. 2010;298(2):R372–7.
Rasmussen P, Brassard P, Adser H, Pedersen MV, Leick L, Hart E, et al. Evidence for a release of brain-derived neurotrophic factor from the brain during exercise. Exp Physiol. 2009;94(10):1062–9.
Gold SM, Schulz KH, Hartmann S, Mladek M, Lang UE, Hellweg R, et al. Basal serum levels and reactivity of nerve growth factor and brain-derived neurotrophic factor to standardized acute exercise in multiple sclerosis and controls. J Neuroimmunol. 2003;138(1–2):99–105.
Winter B, Breitenstein C, Mooren FC, Voelker K, Fobker M, Lechtermann A, et al. High impact running improves learning. Neurobiol Learn Mem. 2007;87(4):597–609.
Goekint M, Heyman E, Roelands B, Njemini R, Bautmans I, Mets T, et al. No influence of noradrenaline manipulation on acute exercise-induced increase of brain-derived neurotrophic factor. Med Sci Sports Exerc. 2008;40(11):1990–6.
Tang SW, Chu E, Hui T, Helmeste D, Law C. Influence of exercise on serum brain-derived neurotrophic factor concentrations in healthy human subjects. Neurosci Lett. 2008;431(1):62–5.
Tsai CL, Pan CY, Chen FC, Wang CH, Chou FY. Effects of acute aerobic exercise on a task-switching protocol and brain-derived neurotrophic factor concentrations in young adults with different levels of cardiorespiratory fitness. Exp Physiol. 2016;101(7):836–50.
Griffin ÉW, Mullally S, Foley C, Warmington SA, O’Mara SM, Kelly ÁM. Aerobic exercise improves hippocampal function and increases BDNF in the serum of young adult males. Physiol Behav. 2011;104(5):934–41.
Laske C, Banschbach S, Stransky E, Bosch S, Straten G, MacHann J, et al. Exercise-induced normalization of decreased BDNF serum concentration in elderly women with remitted major depression. Int J Neuropsychopharmacol. 2010;13(5):595–602.
Ströhle A, Stoy M, Graetz B, Scheel M, Wittmann A, Gallinat J, et al. Acute exercise ameliorates reduced brain-derived neurotrophic factor in patients with panic disorder. Psychoneuroendocrinology. 2010;35(3):364–8.
Rojas Vega S, Strüder HK, Vera Wahrmann B, Schmidt A, Bloch W, Hollmann W. Acute BDNF and cortisol response to low intensity exercise and following ramp incremental exercise to exhaustion in humans. Brain Res. 2006;1121(1):59–65.
Ferris LT, Williams JS, Shen CL. The effect of acute exercise on serum brain-derived neurotrophic factor levels and cognitive function. Med Sci Sports Exerc. 2007;39(4):728–34.
Duclos M, Corcuff JB, Ruffie A, Roger P, Manier G. Rapid leptin decrease in immediate post-exercise recovery. Clin Endocrinol. 1999;50(3):337–42.
Sari R, Balci MK, Balci N, Karayalcin U. Acute effect of exercise on plasma leptin level and insulin resistance in obese women with stable caloric intake. Endocr Res. 2006;32(1–2):9–17.
Jürimäe J, Jürimäe T. Leptin responses to short term exercise in college level male rowers. Br J Sports Med. 2005;39(1):6–9.
Zafeiridis A, Smilios I, Considine RV, Tokmakidis SP. Serum leptin responses after acute resistance exercise protocols. J Appl Physiol. 2003;94(2):591–7.
Sureda A, Mestre-Alfaro A, Banquells M, Riera J, Drobnic F, Camps J, et al. Exercise in a hot environment influences plasma anti-inflammatory and antioxidant status in well-trained athletes. J Therm Biol. 2015;47:91–8.
Baria MR, Miller MM, Borchers J, Desmond S, Onate J, Magnussen R, et al. High intensity interval exercise increases platelet and transforming growth factor- β yield in platelet-rich plasma. PM R. 2020; (August) :2–31.
Ribeiro F, Ribeiro IP, Gonçalves AC, Alves AJ, Melo E, Fernandes R, et al. Effects of resistance exercise on endothelial progenitor cell mobilization in women. Sci Rep. 2017;7(1):1–9.
Gavin TP, Drew JL, Kubik CJ, Pofahl WE, Hickner RC. Acute resistance exercise increases skeletal muscle angiogenic growth factor expression. Acta Physiol. 2007;191(2):139–46.
Norheim F, Hjorth M, Langleite TM, Lee S, Holen T, Bindesbøll C, et al. Regulation of angiopoietin-like protein 4 production during and after exercise. Physiol Rep. 2014;2(8):1–12.
Fery F, Balasse EO. Response of ketone body metabolism to exercise during transition from postabsorptive to fasted state1. Fery F, Balasse EO. Response of ketone body metabolism to exercise during transition from postabsorptive to fasted state. Am J Physiol - Endocrinol Metab. 1986;250(5):E495–501.
Johnson RH, Walton JL. The effect of exercise upon acetoacetate metabolism in athletes and non-athletes. Q J Exp Physiol Cogn Med Sci. 1972;57(1):73–9.
Matoulek M, Svobodova S, Vetrovska R, Stranska Z, Svacina S. Post-exercise changes of beta hydroxybutyrate as a predictor of weight changes. Physiol Res. 2014;63(Suppl 2):S321–5.
Parker MT. Post-exercise reported. :452–5.
Zhang W, Bi S. Hypothalamic regulation of brown adipose tissue thermogenesis and energy homeostasis. Front Endocrinol (Lausanne). 2015;6(1):83.
Rennie MJ, Jennett S, Johnson RH. The metabolic effects of strenuous exercise: a comparison between untrained subjects and racing cyclists. Q J Exp Physiol Cogn Med Sci. 1974;59(3):201–12.
Devlin J, Paton B, Poole L, Sun W, Ferguson C, Wilson J, et al. Blood lactate clearance after maximal exercise depends on active recovery intensity. J Sports Med Phys Fitness. 2014;54(3):271–8.
Acknowledgments
This study was performed as part of a PhD thesis conducted within the Official Doctoral Programme in Biomedicine of the University of Granada, Spain.
Funding
This study was supported by the Spanish Ministry of Economy and Competitiveness via Retos de la Sociedad (DEP2016-79512-R) and European Regional Development Funds (ERDF), the Spanish Ministry of Education (FPU13/04365, FPU16/02828 FPU16/03653), the Redes Temáticas de Investigación Cooperativa RETIC (Red SAMID RD16/0022), the University of Granada Plan Propio de Investigación 2016–Excellence actions: Unit of Excellence on Exercise and Health (UCEES), the University of Granada Plan Propio de Investigación 2018 (Programa Contratos Puente and Perfeccionamiento de Doctores), the Junta de Andalucía, Consejería de Conocimiento, Investigación y Universidades (ERDF; ref. SOMM17/6107/UGR), and the Fundación Alfonso Martín Escudero.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Jonatan R Ruiz and Guillermo Sanchez-Delgado share seniorship.
This article is part of the Topical Collection on Obesity
Rights and permissions
About this article
Cite this article
Mendez-Gutierrez, A., Osuna-Prieto, F.J., Aguilera, C.M. et al. Endocrine Mechanisms Connecting Exercise to Brown Adipose Tissue Metabolism: a Human Perspective. Curr Diab Rep 20, 40 (2020). https://doi.org/10.1007/s11892-020-01319-7
Published:
DOI: https://doi.org/10.1007/s11892-020-01319-7