Abstract
Purpose of Review
Voluntary male medical circumcision (VMMC) has been a cornerstone of HIV prevention in Eastern and Southern Africa (ESA) and is credited in part for declines in HIV incidence seen in recent years. However, these HIV incidence declines change VMMC cost-effectiveness and how it varies across populations.
Recent Findings
Mathematical models project continued cost-effectiveness of VMMC in much of ESA despite HIV incidence declines. A key data gap is how demand generation cost differs across age groups and over time as VMMC coverage increases. Additionally, VMMC models usually neglect non-HIV effects of VMMC, such as prevention of other sexually transmitted infections and medical adverse events. While small compared to HIV effects in the short term, these could become important as HIV incidence declines.
Summary
Evidence to date supports prioritizing VMMC in ESA despite falling HIV incidence. Updated modeling methodologies will become necessary if HIV incidence reaches low levels.
Similar content being viewed by others
Introduction
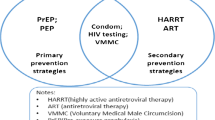
Male circumcision is one of the oldest and most commonly practiced surgical procedures worldwide. Voluntary male medical circumcision (VMMC), circumcision of boys and men by a trained medical provider with the recipient’s consent and without undue influence, has been shown to significantly reduce HIV acquisition among heterosexual men [1–3]. The past two decades have seen major investments in VMMC in Eastern and Southern Africa (ESA), home to one-third of all people living with HIV (PLHIV). VMMC is now a cornerstone of HIV prevention in 15 ESA countries with the highest HIV prevalence and low male circumcision prevalence prior to the mid-2000s: Botswana, Eswatini, Ethiopia, Kenya, Lesotho, Malawi, Mozambique, Namibia, Rwanda, South Africa, South Sudan, Uganda, Tanzania, Zambia, and Zimbabwe.
These ESA priority countries are now showing steady declines in the rates of new HIV infections, driven by a combination of VMMC and antiretroviral therapy (ART) scale-up. As a “one-and-done” procedure that gives lifelong HIV prevention, VMMC has been found in numerous economic evaluations to be one of the most cost-effective HIV interventions available in ESA [4–9]. However, as with any prevention measure, the cost-effectiveness of VMMC declines as HIV incidence in the population falls.
In this review, we summarize the evidence on VMMC’s risks and benefits, methods used to translate these benefits into impact and cost-effectiveness estimates, and the current scope and shortcomings of these methods. We review the current state of evidence as to whether VMMC will remain cost-effective and high priority for HIV budget allocation in the context of declining HIV incidence. Lastly, we discuss how declining HIV incidence may shift the scope of VMMC decision analyses in ESA, including more detailed consideration of non-HIV effects.
Risks and Benefits of VMMC
Although VMMC carries some risks, the benefits of VMMC exceed risks by 100- to 200-fold [10]. One of the largest benefits of VMMC is prevention of HIV acquisition, but other benefits include prevention of other sexually transmitted infections (STIs). This section briefly summarizes evidence regarding the risks and benefits of VMMCs.
Reduction in Individual Risk of HIV
Currently, VMMC is the only one-time biomedical intervention to reduce lifelong HIV risk. Three randomized controlled trials conducted in Kenya, Uganda, and South Africa [1–3] estimated a 60% reduction in HIV infection risk for men in the 2 years following the recommended 6-week post-surgical abstinence period. Similar protection from HIV has been observed in post-trial follow-up and in community-based observational cohorts [11•]. Among men who have sex with men (MSM), the benefits of VMMC are less well-characterized and likely smaller in magnitude, estimated at approximately a 20% reduction in HIV acquisition on average, with heterogeneity depending on factors such as types of sexual encounters [12].
Reduction in Community Risk of HIV
The HIV prevention benefits of VMMC extend beyond the recipient to the broader community. By avoiding infection, a circumcised man indirectly protects sexual partners, who in turn protect their sexual partners, and so forth. Mathematical modeling has suggested that HIV prevention benefits in ESA are approximately equally distributed between direct recipients and their communities over the first 5 years post-intervention. After 5 years, community benefits outpace individual benefits, especially when prevention recipients are male [13]. This is likely because, in generalized epidemics, women experience higher HIV prevalence and incidence than men, meaning that men are more often transmitters than recipients of new HIV infections [14].
Reduction in Urological and Sexually Transmitted Infections
Reports of male circumcision reducing the risk of STIs date back to 1855 [15], well before the HIV pandemic. Modern studies have shown mixed results regarding the effects of circumcision on men’s acquisition of STIs [16–19] and transmission to sexual partners [20–22]. In meta-analyses, evidence strongly supports reduced risk of herpes simplex virus type 2 (HSV-2), human papillomavirus (HPV), and syphilis infections in circumcised men [23], although evidence is mixed for other STIs [24]. Female sexual partners of circumcised men have lower risk of HSV-2, human papillomavirus (HPV), Trichomonas vaginalis, and bacterial vaginosis [25], while sexual partners of MSM have lower risk of HSV-2 and HPV [26]. These effects are largest in populations with high overall prevalence of STIs [24].
Interestingly, reductions in HIV and STIs have also been observed in populations practicing dorsal longitudinal foreskin cutting, in which the foreskin is not removed, but a slit causes complete exposure of the underside of the foreskin and surface of the penile shaft [27]. Both the dorsal slit and full circumcision result in changes to the stratum corneum of the exposed skin [28] and to the composition and diversity of penile microbiota [29], although the precise mechanisms by which these changes reduce STIs are still under investigation.
Risk of Adverse Events
Circumcision is a safe procedure when performed by trained personnel [30, 31] but like any surgical intervention, it carries a small risk of complications. Reported VMMC adverse events have been steadily declining in ESA [32, 33], although reporting is likely incomplete [34, 35]. There is an ongoing need to strengthen post-operative counseling and reporting [35–37] and maintain rigorous monitoring and evaluation [38].
Adverse event frequency differs by patient age [39]. Intraoperative adverse events are more common among patients older than 20 years [32]. Risk of infection is higher, but risk of bleeding is lower for ages 10–14 compared to 15 and older [34, 40–42]. A recent analysis by Lucas et al. [43•] found that boys age < 15 have a greater risk of rare but severe adverse events such as fistulas between the urethra and penile skin. These findings contributed to the 2020 decision by the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR) to raise the minimum age for VMMC to 15 years.
Risk Compensation
A common concern with HIV prevention is that recipients may increase sexual risk behavior, a phenomenon known as risk compensation. Gao et al. recently reviewed condom use and numbers of sexual partners among heterosexual men prior to 2015 and found that VMMC was not associated with increased risk-taking [44]. Several recent studies also failed to find evidence of sexual risk compensation after VMMC [45–49], while others found possible evidence of risk compensation [50–53] or risk trade-offs, such as increases in multiple sex partners combined with increases in condom usage [54]. Kwamba et al. performed a pooled analysis of VMMC randomized trials and cohort studies and found no risk compensation for at least 2 years post-VMMC [55•].
The effects of male circumcision on women’s risky behavior are less understood. Some studies suggest that women who are aware of male circumcision for HIV prevention may have a reduced perception of HIV risk, reduced condom usage, or greater number of sex partners [56, 57]. Further research is needed into the extent and possible mitigation of risk compensation among partners of circumcised men.
VMMC Modeling Approaches
Estimating the long-term population-level impact of VMMC in ESA requires a glimpse into the future, which is typically obtained through mathematical modeling. Several models are being used to inform VMMC policy in ESA, each with different advantages and disadvantages.
Scope of VMMC Models
Like any model, a VMMC model describes how a system — in this case, a human population — behaves over time. The model does not need to incorporate every nuance of the system, provided it captures the predominant features that govern important outputs [58]. VMMC models in ESA have mainly focused on how VMMC affects HIV-related morbidity and mortality, as well as its effect on healthcare spending — usually in the context of donor-funded HIV programs. Other effects of VMMC, including those discussed in the prior section, are rarely included in VMMC modeling (Table 1).
The choice to focus on HIV-related outcomes assumes the predominance of HIV-related outcomes over other health effects of VMMC. This is plausible for ESA in the short term, as HIV is currently responsible for > 90% of the burden of all STIs in ESA [69]. In model projections where HIV burden declines by an order of magnitude or STI burden rises by an order of magnitude (or some combination of the two), STIs could become equally prominent factors for VMMC decision-making. Careful monitoring of VMMC safety, risk compensation, and accruing evidence on other effects will be needed to determine whether these additional factors should be included in VMMC modeling.
Modeling Methods
For an HIV-focused VMMC model, the main goal is to translate VMMC-related changes in HIV susceptibility into projections of population-level HIV incidence, burden, and costs. The key features of these models are (1) HIV transmission, (2) progression of HIV disease, and (3) utilization of HIV services, especially cost-driving ones such as ART. These elements can be modeled in different ways, each with different advantages and disadvantages.
A representation of HIV transmission is needed to simulate the effect of VMMC. Individual-based models are able to simulate person-to-person transmission on a network (for example, the EMOD-HIV model [70]) and can also simulate group-to-group transmission based on collective attributes, such as average viral load (for example, the Synthesis HIV model [71]). Compartmental models, which represent categories of individuals, only simulate group-to-group transmission (for example, Goals [72], Optima HIV [9], and Thembisa [73]), with groups typically defined by age, sex, and key population or other proxy for risk level. Some VMMC models, such as the widely used the Decision Makers’ Program Planning Toolkit, Version 2 (DMPPT2) model [74], do not explicitly represent transmission at all, but instead “borrow” HIV incidence projections from a different model (Goals) and adjust these based on changes in male circumcision prevalence.
Representation of progression of HIV infection allows models to translate transmission reductions into changes in morbidity and mortality. Most models represent disease progression as a decline in CD4 + T-cell count, with lower CD4 counts leading to reduced quality of life due to AIDS-related complications and higher mortality rates. Age-structured models can then estimate the years of life lost due to HIV/AIDS. Models without age structure can also estimate this by approximating the average age at which an AIDS-related death is likely to occur.
Representation of HIV services is required to assess cost-effectiveness and budget impacts of VMMC, of which the most significant portion is treatment with ART. Minimally, such models must estimate the reduced need for ART due to HIV infections averted by VMMC, translating this into cost reductions over time. However, some models offer additional details such as ART drug resistance, non-adherence, treatment interruption, and delayed treatment initiation or re-initiation.
Multi-model Analyses
In general, simpler VMMC models such as Goals and DMPPT2 have been applied more widely in ESA than complex models such as those incorporating age-structured transmission, patterns of engagement along the care continuum, and/or evolution of drug resistance. This is because simpler models tend to provide greater ease-of-use, interpretability of methods, and ability to be run without specialized computing equipment or expertise. However, it is not always clear which simplifications are acceptable in the context of evaluating VMMC programs. Multi-model analyses enable a head-to-head comparison of models evaluating the same policy options, with the goal of determining whether the estimates and policy recommendations are similar or different across model structures and assumptions.
Ideally, a multi-model analysis includes models with diverse structures, assumptions, and ways of fitting epidemic data. It is critical that model comparisons not create “groupthink” by discarding potentially valid model structures and assumptions for the sake of reaching agreement. However, the models should align on the specific policies and scenarios under evaluation. Korenromp et al. recently undertook a model comparison of three models of VMMC in South Africa with diverse structures: Goals (simpler compartmental), Thembisa (more complex compartmental), and EMOD (complex agent-based/network). The analysis aligned on the number of VMMCs performed by age and geography, the cost per circumcision and per year of ART, and the time horizon and annual discount rate for the analysis, and found similar estimates for VMMC impact on HIV transmission, burden, and healthcare budgets across the diverse model structures [59••].
Cost and Cost-effectiveness of VMMC
VMMC has generally been considered one of the most cost-effective HIV prevention options available in ESA. However, questions have been raised as to whether shifts in the HIV epidemic might change VMMC cost-effectiveness or have implications for optimal ways in which VMMC resources should be distributed. Here we review evidence and current limitations in assessing the long-term cost-effectiveness of VMMC in ESA priority countries.
VMMC Costs
Numerous studies have attempted to quantify the cost of VMMC in ESA priority countries. Most studies have focused on service delivery costs, such as personnel, capital costs of buildings and equipment, and recurrent costs of rent, maintenance, and consumable goods [75]. Pineda-Antunez et al. compared ESA country averages for service delivery costs per VMMC delivered and found significant variation by country income level, with low-income country facilities spending a mean of US$42 per VMMC, while upper-middle income country facilities spent a mean of US$114 per VMMC [76•]. In most countries, the largest cost component was personnel, and higher salary levels tend to drive differences in costs.
The validity of a country-level unit cost for VMMC has been challenged because, within a country, unit costs vary greatly across facilities. Bautista-Arredondo et al. [77] found that much of the variation in VMMC cost can be predicted by a facility’s attributes, with lower-volume facilities, hospitals, and privately owned facilities incurring higher unit costs, while urban versus rural location did not independently predict unit costs. This study estimates that a 10% increase in facility volume could reduce cost per VMMC by 12–22%.
An important limitation of these studies is that they rarely include indirect costs incurred above the facility level, such as informational campaigns, program operations, and monitoring and evaluation [78]. One study estimated that in South Africa, over US$14.2 million was spent in 2014 on VMMC outreach efforts such as hiring community mobilizers and carrying out media campaigns [78]. Mangenah et al. found that in Zimbabwe, adding human-centered design (HCD) approaches to standard VMMC demand creation lowered the cost per VMMC, but further addition of HIV self-testing services increased the cost per VMMC [79••].
In addition to health system costs, VMMC incurs some out-of-pocket costs for patients. In South Africa, transportation was the largest out-of-pocket cost for VMMC clients, costing US$9.20 per client on average, or roughly 7–8% of the VMMC unit cost [80]. These costs are not included in economic analyses from the health system perspective, but are useful for analyses from the broader societal perspective.
VMMC Cost-effectiveness
VMMC has been estimated in many settings to reimburse the healthcare system through treatment costs avoided over the recipient’s lifetime, even before taking into account health benefits. Korenromp et al. used three HIV models to assess the budgetary impact of the South African VMMC program implemented in 2009–2017. In all models, VMMC costs would be reimbursed by the savings from averted treatment around 2034–2039 [59••]. These findings are consistent with earlier analyses in South Africa, which estimated that the costs of a given circumcision could be amortized over as little as 12 years (for a 25-year-old) or as much as 23 years (for a 10-year-old) [60].
VMMC cost-effectiveness estimates have tended to be consistent across models of the same setting, but widely different across ESA settings. Korenromp et al. found a cost of $1070-1220 per HIV infection averted for the South African VMMC program, a remarkable agreement across three South Africa HIV models with widely different structures [59••]. In an analysis of 14 ESA priority countries, Kripke et al. found that costs per infection averted ranged from US$1300 to $22,000 [65••]. The variability was driven more by the wide differences in HIV incidence across ESA settings [13, 81–83] (Fig. 1a) than by differences in unit costs of VMMC (Fig. 1b). The analysis suggests that providing VMMC in high-incidence countries is more important than reducing costs. A limitation of this analysis is that it approximated above-facility costs as a 15% overhead on service delivery costs in all countries, although it is likely that demand generation costs vary by country and over time as more demand is satisfied.
Association between cost per HIV infection averted by VMMC and a HIV incidence or bunit cost of VMMC. Unit costs and costs per infection averted were obtained from a study by Kripke et al. [65••] which used direct costs and modeled impact of VMMCs performed over 2010–2025 for each country except for Kenya where only the Nyanza region was included. Incidence was obtained at the national level from UNAIDS [81] and for Nyanza from three published estimates [13, 82, 83]
Budgeting for VMMC
Although VMMC is eventually cost-saving in much of ESA, health agencies cannot always afford to “lend” to VMMC programs in the short term when there are competing health resource needs. Internationally funded HIV programs typically consider an intervention to be cost-effective if it costs less than ~ US$500 per DALY averted or QALY gained, after applying an annual discount rate of at least 3% [84, 85]. Many ESA VMMC programs meet these cost-effectiveness benchmarks. For example, Kripke et al. found that Malawi’s VMMC program costs US$120 per DALY averted in urban areas and US$355 per DALY averted in rural areas [86•], both of which would be considered cost-effective within internationally funded HIV programs.
However, in the event that international donors do not cover the costs of VMMC programs, domestic funding for VMMC is much more constrained in lower-income countries. In Malawi, it is estimated that only services costing less than US$130–164 per DALY averted would be a cost-effective use of limited domestic health spending [87, 88]. In this case, only urban VMMCs would be considered cost-effective in Malawi. In contrast, higher-income economies in ESA face less stringent budget constraints. In South Africa, it is estimated that domestic health spending is cost-effective below US$3525 per DALY averted [89], making VMMC highly cost-effective [5, 90].
Another approach to estimating cost-effectiveness is an analysis that optimizes the allocation of a fixed budget across HIV services. In budget optimization analyses, VMMC has consistently been recommended for funding in South Africa [4, 5], Kenya [6], Zimbabwe [7, 8], and elsewhere in ESA [9], usually rising to the top of budget prioritization due to its cost-effectiveness. The recommended budget allocation for VMMC is usually smaller than for ART, however, due to the higher lifetime cost of ART compared to VMMC, and the immediacy of ART health benefits compared to more delayed benefits from VMMC.
Subnational Allocation of VMMC
We have seen how the impact and cost-effectiveness of VMMC can vary widely across ESA countries. It is therefore logical that VMMC cost-effectiveness varies subnationally. These differences have been evident in recent subnational estimation of VMMC impact and cost-effectiveness.
Geographic Prioritization of VMMC
The relationship between incidence and VMMC impact on a national level (Fig. 1) suggests that there would be a strong relationship between incidence and VMMC impact across subnational geographic areas. This relationship has indeed been evident in subnational VMMC modeling, but despite subnational variation, VMMC was found to be cost-saving in all regions of South Africa [91] and Uganda [92], and all 11 VMMC priority regions of Tanzania [93]. In Malawi, VMMC was found to be cost-saving in the South West and South East health zones and cost-effective but not cost-saving in the Northern and Central West zones [86•]. VMMC was not found to be cost-effective in the Central East zone where Lilongwe is located, but when the geographies were split up by urban versus rural rather than by zone, VMMC in urban areas was found to be cost-saving, providing a rationale for continuing the already-established VMMC program in Lilongwe.
Subnational geographic analyses were confounded by wide uncertainty ranges in the HIV incidence projections, leading to wide and often overlapping uncertainty ranges for VMMC cost-effectiveness by geography. Improvements in methods for estimating HIV incidence with greater geographic granularity, including tests for recent HIV infection [94] and geospatial “big data” methods [95], are poised to enable more sophisticated geographic prioritization of VMMC.
Age-Based Prioritization of VMMC
In the early years of VMMC scale-up, a vast majority of VMMC clients were adolescent boys under age 15, while the WHO/UNAIDS VMMC coverage targets had been set for ages 15–49. This raised questions about how best to prioritize VMMC by age. In response, age-based prioritization was examined in a multi-model analysis spanning nine ESA countries [96].
The ASSA2008 model of South Africa showed the greatest financial savings (US$617 per circumcision) when circumcising 20-year-olds, assuming a discount rate of 5% over a 45-year timeframe [90]. In a multi-model comparison, two models, ASM and DMPPT2, used harmonized assumptions about VMMC costs, discount rates of 3% per year, and a time horizon of 15 years. DMPPT2, applied in eight countries, found the largest number of HIV infection averted per VMMC over 15 years in the 20–24-, 25–29-, and 30–34-year age groups [74], while ASM, applied in Zambia and Zimbabwe, found the highest number of infections averted in the 15–19-, 20–24-, and 25–29-year age groups [67]. An important driver of these differences was the age distribution of HIV incidence, which was highest in men ages 20–29 in ASM and ages 25–34 in DMPPT2.
An important limitation of these cost-effectiveness analyses is the lack of data on how VMMC cost varies by client age. Demand creation tends to become more challenging at older ages. Kripke et al. [61] attempted to address this with fictitious scenarios about the relative costs of circumcising adolescent versus adult clients in Zimbabwe, finding that a 50% higher unit cost for adults compared to adolescents would make VMMC more cost-effective in adolescents than adults. Torres-Rueda et al. [97•] conducted a randomized, controlled trial comparing VMMC with and without strategies to generate demand among 20–29-year-olds. VMMC with demand creation intervention was found to be more cost-effective overall, but the intervention did not preferentially increase uptake among adults compared to adolescents, highlighting the challenge of generating demand in older age groups.
The Future of VMMC in ESA: Opportunities and Challenges
ESA countries are now striving toward the Sustainable Development Goal of HIV epidemic control by 2030 [98], an effort in which VMMC could play a substantial role. In Uganda [99], Kenya [100], and elsewhere, attainment of high VMMC coverage has been associated with declines in HIV incidence, and model-based predictions suggests that many more infections will be averted over the coming decades by VMMCs already performed [59••]. Modeling further predicts that achieving 90% VMMC coverage would avert as many HIV infections as attainment of the UNAIDS 90–90-90 HIV treatment goals [62]. However, most of ESA is far behind VMMC targets [101], despite many areas approaching or surpassing the 90–90-90 treatment targets [102]. The totality of this evidence suggests that VMMC remains an underutilized opportunity to accelerate HIV epidemic control.
It comes as little surprise that VMMC, even when highly cost-effective as an HIV intervention, is more difficult to advocate for than more direct interventions such as ART. Millions of PLHIV are almost certainly alive today thanks to ART. With VMMC, it is impossible to point to a specific HIV-negative person and know that this particular person remained negative because of VMMC. Additionally, most of the benefits of VMMC accrue over many years. Even though cost-effectiveness calculations take into account discounting over time, the long wait times further obstruct the visibility of VMMC’s benefits. Decision-makers must rely on models, rather than direct observation, in order to motivate prioritizing VMMC — which, in turn, requires credibility, visibility, and trust in VMMC modeling.
As we have discussed, there are many types of VMMC models, and multi-model analyses can be used to test the robustness of VMMC estimates to differences in model structures and assumptions. However, even multi-model analyses can fail to adequately guide VMMC decision-making when models provide conflicting results, or when all participating models use similarly flawed assumptions. For example, models provided conflicting results regarding optimal age groups for VMMC, even after harmonizing assumptions about time horizons and discount rates. Improving the accuracy and precision of age-specific HIV incidence estimation could help to resolve these differences. VMMC modeling is also susceptible to use of common flawed assumptions, especially when models rely on common and imperfect data sources for key inputs such as population sizes and VMMC coverage levels [103]. Demand generation costs, especially how they change across population groups and levels of VMMC coverage, are a particularly important data gap.
Finally, few VMMC models consider impacts of VMMC other than direct reductions in HIV acquisition. However, as HIV incidence declines, other impacts will become non-negligible, and models will need to adapt to represent VMMC impacts more comprehensively.
Conclusions
Although VMMC remains one of the most efficient HIV interventions available in ESA, its benefits are not as visible as other HIV interventions, such as ART. Mathematical models are needed to estimate the impact and cost-effectiveness of VMMC, often as a multi-model analysis to check the robustness of estimates to different model structures and assumptions. Recent multi-model analyses have confirmed the cost-effectiveness of VMMC in most ESA settings, especially those with high HIV incidence. However, some disagreement remains regarding the optimal age groups to receive VMMC, and model projections could be improved by filling key data gaps, such as demand generation costs across populations and time. Despite these limitations, modeling has provided crucial input into VMMC strategic directions [104] and continues to reinforce the importance of VMMC in ESA.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Auvert B, Taljaard D, Lagarde E, Sobngwi-Tambekou J, Sitta R, Puren A. Randomized, Controlled intervention trial of male circumcision for reduction of HIV infection risk: the ANRS 1265 trial. PLoS Med. 2005;2: e298.
Gray RH, Kigozi G, Serwadda D, et al. Male circumcision for HIV prevention in men in Rakai, Uganda: a randomised trial. The Lancet. 2007;369:657–66.
Bailey RC, Moses S, Parker CB, Agot K, Maclean I, Krieger JN, Williams CF, Campbell RT, Ndinya-Achola JO. Male circumcision for HIV prevention in young men in Kisumu, Kenya: a randomised controlled trial. The Lancet. 2007;369:643–56.
Chiu C, Johnson LF, Jamieson L, Larson BA, Meyer-Rath G. Designing an optimal HIV programme for South Africa: does the optimal package change when diminishing returns are considered? BMC Public Health. 2017. https://doi.org/10.1186/s12889-017-4023-3.
Meyer-Rath G, van Rensburg C, Larson B, Jamieson L, Rosen S. Revealed willingness-to-pay versus standard cost-effectiveness thresholds: evidence from the South African HIV Investment Case. PLoS ONE. 2017;12: e0186496.
Lukoba B, Simiyu J, Chege W, Kelly S, Minnery M, Sithole L, Shubber Z. Improving allocative efficiency of the HIV response in Kenya: a country-level analysis using the Optima HIV model. Washington, DC: World Bank; 2020.
Taramusi I, Sisimayi C, Benedikt C, Cheikh N, Fraser N, Shubber Z, et al. Improving the allocative efficiency of the HIV response across the care cascade in Zimbabwe: findings from a modelling analysis. 2019. https://doi.org/10.1596/33271.
McGillen JB, Stover J, Klein DJ, et al. The emerging health impact of voluntary medical male circumcision in Zimbabwe: an evaluation using three epidemiological models. PLoS ONE. 2018;13: e0199453.
Kelly SL, Martin-Hughes R, Stuart RM, et al. The global Optima HIV allocative efficiency model: targeting resources in efforts to end AIDS. The Lancet HIV. 2018;5:e190–8.
Morris BJ, Moreton S, Krieger JN. Critical evaluation of arguments opposing male circumcision: a systematic review. J Evid Based Med. 2019;12:263–90.
• Farley TM, Samuelson J, Grabowski MK, Ameyan W, Gray RH, Baggaley R. Impact of male circumcision on risk of HIV infection in men in a changing epidemic context – systematic review and meta-analysis. J Intern AIDS Soc. 2020. https://doi.org/10.1002/jia2.25490. Farley et al. review evidence of VMMC effectiveness, finding the intervention to be similarly effective in randomized controlled trials and in community-based cohorts where VMMC has been implemented. They further estimate that VMMC programs have averted approximately half a million HIV infections over the decade 2008–2018.
Sharma SC, Raison N, Khan S, Shabbir M, Dasgupta P, Ahmed K. Male circumcision for the prevention of human immunodeficiency virus (HIV) acquisition: a meta-analysis. BJU Int. 2018;121:515–26.
Mudimu E, Peebles K, Mukandavire Z, Nightingale E, Sharma M, Medley GF, Klein DJ, Kripke K, Bershteyn A. Individual and community-level benefits of PrEP in western Kenya and South Africa: implications for population prioritization of PrEP provision. PLoS ONE. 2020. https://doi.org/10.1371/journal.pone.0244761.
Bershteyn A, Klein DJ, Eckhoff PA. Age-dependent partnering and the HIV transmission chain: a microsimulation analysis. J R Soc Interface. 2013;10:20130613.
Hutchinson J. On the influence of circumcision in preventing syphilis. Med Times Gazette. 1855;32:542–3.
Auvert B, Sobngwi-Tambekou J, Cutler E, Nieuwoud M, Lissouba P, Puren A, Taljaard D. Effect of male circumcision on the prevalence of high-risk human papillomavirus in young men: results of a randomized controlled trial conducted in orange farm, South Africa. J Infect Dis. 2009;199:14–9.
Sobngwi-Tambekou J, Taljaard D, Nieuwoudt M, Lissouba P, Puren A, Auvert B. Male circumcision and Neisseria gonorrhoeae, Chlamydia trachomatis and Trichomonas vaginalis: observations after a randomised controlled trial for HIV prevention. J Infect Dis. 2009;85:116–20.
Tarnaud C, Lissouba P, Cutler E, Puren A, Taljaard D, Auvert B. Association of low-risk human papillomavirus infection with male circumcision in young men: results from a longitudinal study conducted in orange farm (South Africa). Infect Dis Obstet Gynecol. 2011.
Olesen TB, Munk C, Mwaiselage J, Kahesa C, Rasch V, Frederiksen K, Iftner T, Kjaer SK. Male circumcision and the risk of gonorrhoea, syphilis, HIV and human papillomavirus among men in Tanzania. Int J STD AIDS. 2019;30:1408–16.
Davis M-A, Gray RH, Grabowski MK, et al. Male circumcision decreases high-risk human papillomavirus viral load in female partners: a randomized trial in Rakai, Uganda. Int J Cancer. 2013;133:1247–53.
Millett GA, Flores SA, Gary Marks J, Reed B, Herbst JH. Circumcision status and risk of HIV and sexually transmitted infections among men who have sex with men: a meta-analysis. JAMA. 2008;300:1674–84.
Canadas MP, Darwich L, Videla S, Sirera G, Coll J, Rafael M-LA, HIV-HPV Study Group. Circumcision and penile human papillomavirus prevalence in human immunodeficiency virus-infected men: heterosexual and men who have sex with men. Clin Microbiol Infect. 2013;19:611–6.
Matoga M, Hosseinipour MC, Jewett S, Hoffman IF, Chasela C. Effects of HIV voluntary medical male circumcision programs on sexually transmitted infections. Curr Opin Infect Dis. 2020. https://doi.org/10.1097/QCO.0000000000000696.
Van Howe RS. Sexually transmitted infections and male circumcision: a systematic review and meta-analysis. Urology. 2013:42 pages.
Morris BJ, Hankins CA, Banerjee J, Lumbers ER, Mindel A, Klausner JD, Krieger JN. Does male circumcision reduce women’s risk of sexually transmitted infections, cervical cancer, and associated conditions? Public Health. 2019;7:4.
Yuan T, Fitzpatrick T, Ko N-Y, et al. Circumcision to prevent HIV and other sexually transmitted infections in men who have sex with men: a systematic review and meta-analysis of global data. Lancet Glob Health. 2019;7:e436-437.
Vallely AJ, MacLaren D, David M, et al. Dorsal longitudinal foreskin cut is associated with reduced risk of HIV, syphilis and genital herpes in men: a cross-sectional study in Papua New Guinea. J Int AIDS Soc. 2017;20:21358.
Prodger JL, Kaul R. The biology of how circumcision reduces HIV susceptibility: broader implications for the prevention field. AIDS Res Ther. 2017;14:49.
Onywera H, Williamson A-L, Ponomarenko J, Meiring TL. The penile microbiota in uncircumcised and circumcised men: relationships with HIV and human papillomavirus infections and cervicovaginal microbiota. Front Med. 2020;7:383.
Mutanekelwa I, Siziya S, Daka V, et al. Prevalence and correlates of voluntary medical male circumcision adverse events among adult males in the Copperbelt Province of Zambia: a cross-sectional study. PLoS ONE. 2021;16: e0256955.
Phili R, Abdool-Karim Q, Ngesa O. Low adverse event rates following voluntary medical male circumcision in a high HIV disease burden public sector prevention programme in South Africa. J Int AIDS Soc. 2014;17:19275.
Hellar A, Plotkin M, Lija G, et al. Adverse events in a large-scale VMMC programme in Tanzania: findings from a case series analysis. J Int AIDS Soc. 2019;22: e25369.
Victor O, Phiona M, Vernon M, et al. Adverse event trends within a large-scale, routine, voluntary medical male circumcision program in Zimbabwe, 2014–2019. J Acquir Immune Defic Syndr. 2021;88:173–80.
Brito A, Korn A, Monteiro L, Mudender F, Maiela A, Come J, Barnhart S, Feldacker C. Need for improved detection of voluntary medical male circumcision adverse events in Mozambique: a mixed-methods assessment. BMC Health Serv Res. 2019;19:855.
Feldacker C, Murenje V, Makunike-Chikwinya B, et al. Balancing competing priorities: quantity versus quality within a routine, voluntary medical male circumcision program operating at scale in Zimbabwe. PLoS ONE. 2020;15: e0240425.
Kohler PK, Namate D, Barnhart S, et al. Classification and rates of adverse events in a Malawi male circumcision program: impact of quality improvement training. BMC Health Serv Res. 2016. https://doi.org/10.1186/s12913-016-1305-x.
Ashengo TA, Grund J, Mhlanga M, et al. Feasibility and validity of telephone triage for adverse events during a voluntary medical male circumcision campaign in Swaziland. BMC Public Health. 2014;14:858.
Gilbertson A, Ongili B, Odongo FS, Hallfors DD, Rennie S, Kwaro D, Luseno WK. Voluntary medical male circumcision for HIV prevention among adolescents in Kenya: unintended consequences of pursuing service-delivery targets. PLoS ONE. 2019;14: e0224548.
Lawal TA, Oluwabunmi Olapade-Olaopa E. Circumcision and its effects in Africa. Transl Androl Urol. 2017;6:149–57.
O’Bryan G, Feldacker C, Ensminger A, et al. Adverse event profile and associated factors following surgical voluntary medical male circumcision in two regions of Namibia, 2015–2018. PLoS ONE. 2021;16: e0258611.
Feldacker C, Bochner AF, Murenje V, et al. Timing of adverse events among voluntary medical male circumcision clients: implications from routine service delivery in Zimbabwe. PLoS ONE. 2018;13: e0203292.
Bochner AF, Feldacker C, Makunike B, et al. Adverse event profile of a mature voluntary medical male circumcision programme performing PrePex and surgical procedures in Zimbabwe. J Int AIDS Soc. 2017;19:21394.
• Lucas T, Hines JZ, Samuelson J, et al. Urethrocutaneous fistulas after voluntary medical male circumcision for HIV prevention-15 African Countries, 2015–2019. BMC Urol. 2021;21:23. Lucas et al. estimate rates of urethrocutaneous fistulas, a severe adverse event in which abnormal openings between the urethra and penile skin allow urine to escape, across 15 African countries providing VMMC for HIV prevention. Though very rare (41 fistulas total), fistulas were more common in patients < 15 (0.61 fistulas per 100,000 VMMCs) versus ≥ 15 years old (0.01 fistulas per 100,000 VMMCs), with an odds ratio of approximately 51.
Gao Y, Yuan T, Zhan Y, et al. Association between medical male circumcision and HIV risk compensation among heterosexual men: a systematic review and meta-analysis. Lancet Glob Health. 2021;9:E932–41.
Shi C-F, Li M, Dushoff J. Evidence that promotion of male circumcision did not lead to sexual risk compensation in prioritized Sub-Saharan countries. PLoS One. 2017;12:e0175928.
Ortblad KF, Harling G, Chimbindi N, Tanser F, Salomon JA, Bärnighausen T. Does incident circumcision lead to risk compensation? Evidence from a population cohort in KwaZulu-Natal, South Africa. J Acquir Immune Defic Syndr. 2019;80:269–75.
Kankaka EN, Ssekasanvu J, Prodger J, Nabukalu D, Nakawooya H, Ndyanabo A, Kigozi G, Gray R. Sexual risk behaviors following circumcision among HIV-positive men in Rakai, Uganda. AIDS Care. 2018;30:990–6.
Westercamp M, Jaoko W, Mehta S, Abuor P, Siambe P, Bailey RC. Changes in male circumcision prevalence and risk compensation in the Kisumu, Kenya population, 2008–2013. J Acquir Immune Defic Syndr. 2017;74:e30–7.
Spees LP, Wirth KE, Mawandia S, Bazghina-werq S, Ledikwe JH. Sexual risk compensation following voluntary medical male circumcision: results from a prospective cohort study amongst human immunodeficiency virus-negative adult men in Botswana. South Afr J HIV Med. 2020;21:1157.
Chatsika ZJ, Kumitawa A, Samuel V, Azizi SC, Jumbe VC. Voluntary medical male circumcision and sexual practices among sexually active circumcised men in Mzuzu, Malawi: a cross-sectional study. BMC Public Health. 2020. https://doi.org/10.1186/s12889-020-8309-5.
Kibira SPS, Sandøy IF, Daniel M, Atuyambe LM, Makumbi FE. A comparison of sexual risk behaviours and HIV seroprevalence among circumcised and uncircumcised men before and after implementation of the safe male circumcision programme in Uganda. BMC Public Health. 2016. https://doi.org/10.1186/s12889-015-2668-3.
Ahinkorah BO, Hagan JEJ, Seidu A-A, Torgbenu E, Budu E, Schack T. Understanding the linkages between male circumcision and multiple sexual partnership among married Ghanaian men: analysis of data from the 2014 Ghana demographic and health survey. 2020. 26:100622.
Keetile M. An assessment of sexual risk behaviours among circumcised and uncircumcised men before and after the implementation of the safe male circumcision programme in Botswana. AIDS Care. 2020;32:1594–601.
Masango BZ, Ferrandiz-Mont D, Chiao C. Associations between early circumcision, sexual and protective practices, and HIV among a national sample of male adults in Eswatini. AIDS Behav. 2021;25:973–82.
• Kabwama SN, Ssewanyana D, Berg-Beckhoff G. The association between male circumcision and condom use behavior - a meta-analysis. Mater Sociomed. 2018;30:62–6. Kabwama et al. reviewed evience of risk compensation involving changes in male condom use after VMMC. In a pooled analysis of 5 studies, they found that the OR for condom use was 0.91 (95% CI: 0.57–1.45) at 6 months, 1.08 (95% CI: 0.87–1.34) at 12 months, and 1.11 (95% CI: 0.85, 1.45) at 24 months after VMMC. The review suggests no change in condom use after VMMC.
Kalichman S, Mathews C, Kalichman M, Eaton LA, Nkoko K. Male circumcision for HIV prevention: awareness, risk compensation, and risk perceptions among South African women. Glob Public Health. 2018;13:1682–90.
Kapumba BM, King R. Perceived HIV-protective benefits of male circumcision: risk compensatory behaviour among women in Malawi. PLoS ONE. 2019;14: e0211015.
Bershteyn A, Kim H-Y, Scott Braithwaite R. Real-time infectious disease modeling to inform emergency public health decision making. Annu Rev Public Health. 2022. https://doi.org/10.1146/annurev-publhealth-052220-093319.
•• Korenromp EL, Bershteyn A, Mudimu E, et al. The impact of the program for medical male circumcision on HIV in South Africa: analysis using three epidemiological models. Gates Open Res. 2021;5:15. Korenromp et al. present a systematic comparison of three mathematical models of VMMC in South Africa with diverse structures: Goals (simpler compartmental), Thembisa (more complex compartmental), and EMOD (complex agent-based/network). The study standardized the number of VMMCs performed by age and geography in each model, the cost per circumcision and per year of ART, and the time horizon and annual discount rate for the analysis, and found similar estimates for VMMC impact on HIV transmission, burden, and healthcare budgets across the models.
Haacker M, Fraser-Hurt N, Gorgens M. Effectiveness of and financial returns to voluntary medical male circumcision for HIV prevention in South Africa: an incremental cost-effectiveness Analysis. PLoS Med. 2016;13: e1002012.
Kripke K, Hatzold K, Mugurungi O, Ncube G, Xaba S, Gold E, Ahanda KS, Kruse-Levy N, Njeuhmeli E. Modeling impact and cost-effectiveness of increased efforts to attract voluntary medical male circumcision clients ages 20–29 in Zimbabwe. PLoS ONE. 2016;11: e0164144.
Kripke K, Reed J, Hankins C, Smiley G, Laube C, Njeuhmeli E. Impact and cost of scaling up voluntary medical male circumcision for HIV prevention in the context of the new 90–90-90 HIV treatment targets. PLoS ONE. 2016;11: e0155734.
Kripke K, Opuni M, Odoyo-June E, Onyango M, Young P, Serrem K, Ojiambo V, Schnure M, Stegman P, Njeuhmeli E. Data triangulation to estimate age-specific coverage of voluntary medical male circumcision for HIV prevention in four Kenyan counties. PLoS ONE. 2018;13: e0209385.
Njeuhmeli E, Opuni M, Schnure M, et al. Scaling up voluntary medical male circumcision for human immunodeficiency virus prevention for adolescents and young adult men: a modeling analysis of implementation and impact in selected countries. Clin Infect Dis. 2018;66:S166–72.
•• Kripke K, Njeuhmeli E, Samuelson J, et al. Assessing progress, impact, and next steps in rolling out voluntary medical male circumcision for HIV prevention in 14 priority countries in Eastern and Southern Africa through 2014. PLoS ONE. 2016;11:e0158767. Kripke et al. estimated the cost per HIV infection averted for VMMC programs in 14 ESA priority countries. Costs per infection averted varied widely: from US$1,300 to US$22,000.
Dent J, Gaspar N, Njeuhmeli E, Kripke K. Age targeting and scale-up of voluntary medical male circumcision in Mozambique. PLoS ONE. 2019;14: e0211958.
Awad SF, Sgaier SK, Lau FK, et al. Could circumcision of HIV-positive males benefit voluntary medical male circumcision programs in Africa? Mathematical modeling analysis. PLoS ONE. 2017;12: e0170641.
Njeuhmeli E, Forsythe S, Reed J, et al. Voluntary medical male circumcision: modeling the impact and cost of expanding male circumcision for HIV prevention in Eastern and Southern Africa. PLoS Med. 2011;8: e1001132.
GBD Results Tool | GHDx. http://ghdx.healthdata.org/gbd-results-tool. Accessed 22 Feb 2022.
Bershteyn A, Gerardin J, Bridenbecker D, et al. Implementation and applications of EMOD, an individual-based multi-disease modeling platform. Pathog Dis. 2018. https://doi.org/10.1093/femspd/fty059.
Phillips AN, Bansi-Matharu L, Venter F, et al. Updated assessment of risks and benefits of dolutegravir versus efavirenz in new antiretroviral treatment initiators in sub-Saharan Africa: modelling to inform treatment guidelines. Lancet HIV. 2020;7:e193–200.
Stover J, Bollinger L, Izazola JA, Loures L, DeLay P, Ghys PD, Fast Track modeling working group. What is required to end the AIDS epidemic as a public health threat by 2030? The cost and impact of the Fast-Track approach. PLoS ONE. 2016;11: e0154893.
van Schalkwyk C, Dorrington RE, Seatlhodi T, Velasquez C, Feizzadeh A, Johnson LF. Modelling of HIV prevention and treatment progress in five South African metropolitan districts. Sci Rep. 2021;11:5652.
Kripke K, Opuni M, Schnure M, Sgaier S, Castor D, Reed J, Njeuhmeli E, Stover J. Age targeting of voluntary medical male circumcision programs using the Decision Makers’ Program Planning Toolkit (DMPPT) 2.0. PLoS ONE. 2016;11:e0156909.
DeCormier PW, Bollinger LA, Alexander L, et al. Developing the Global Health Cost Consortium Unit Cost Study Repository for HIV and TB: methodology and lessons learned. Afr J AIDS Res. 2019;18:263–76.
• Pineda-Antunez C, Martinez-Silva G, Cerecero-Garcia D, et al. Meta-analysis of average costs of HIV testing and counselling and voluntary medical male circumcision across thirteen countries. Afr J AIDS Res. 2019;18:341–9. Pineda-Antunez reviewed costs of HIV testing and counseling and VMMC. They found VMMC costs to be US$59 on average (95% CI US$45 – US$74), of which 55% was personnel costs.
Bautista-Arredondo S, Pineda-Antunez C, Cerecero-Garcia D, et al. Moving away from the “unit cost”. Predicting country-specific average cost curves of VMMC services accounting for variations in service delivery platforms in Sub-Saharan Africa. PLOS ONE. 2021;16:e0249076.
Tchuenche M, Palmer E, Haté V, Thambinayagam A, Loykissoonlal D, Njeuhmeli E, Forsythe S. The cost of voluntary medical male circumcision in South Africa. PLoS ONE. 2016;11: e0160207.
•• Mangenah C, Mavhu W, Garcia DC, et al. Relative efficiency of demand creation strategies to increase voluntary medical male circumcision uptake: a study conducted as part of a randomised controlled trial in Zimbabwe. BMJ Glob Health. 2021;6: e004983. Mangenah et al. compared the costs of four VMMC demand creation strategies in Zimbabwe: standard practice, addition of HIV self-testing, addition of human-centered design (HCD), or both. HCD lowered the cost per VMMC compared to standard practice, but further addition of HIV self-testing raised the cost per VMMC.
Tchuenche M, Haté V, McPherson D, Palmer E, Thambinayagam A, Loykissoonlal D, Njeuhmeli E, Forsythe S. Estimating client out-of-pocket costs for accessing voluntary medical male circumcision in South Africa. PLoS ONE. 2016;11: e0164147.
UNAIDS Global HIV & AIDS statistics — fact sheet. https://www.unaids.org/en/resources/fact-sheet. Accessed 15 Feb 2022.
Alsallaq RA, Buttolph J, Cleland CM, Hallett T, Inwani I, Agot K, Kurth AE. The potential impact and cost of focusing HIV prevention on young women and men: a modeling analysis in western Kenya. PLoS ONE. 2017;12: e0175447.
Bershteyn A, Mutai KK, Akullian AN, Klein DJ, Jewell BL, Mwalili SM. The influence of mobility among high-risk populations on HIV transmission in Western Kenya. Infect Dis Model. 2018;3:97–106.
Revill P, Walker S, Cambiano V, Phillips A, Sculpher MJ. Reflecting the real value of health care resources in modelling and cost-effectiveness studies—the example of viral load informed differentiated care. PLoS ONE. 2018;13: e0190283.
Vyas S, Songo J, Guinness L, Dube A, Geis S, Kalua T, Todd J, Renju J, Crampin A, Wringe A. Assessing the costs and efficiency of HIV testing and treatment services in rural Malawi: implications for future “test and start” strategies. BMC Health Serv Res. 2020;20:1–11.
• Kripke K, Chimbwandira F, Mwandi Z, Matchere F, Schnure M, Reed J, Castor D, Sgaier S, Njeuhmeli E. Voluntary medical male circumcision for HIV prevention in Malawi: modeling the impact and cost of focusing the program by client age and geography. PLoS ONE. 2016;11:e0156521. Kripke et al. used the DMPPT2 model to estimate VMMC impact and cost-effectiveness in Malawi. They found VMMC to be cost-effective in most health zones and especially cost-effective in urban areas at US$120 per disability-adjusted life-year averted.
Woods B, Revill P, Sculpher M, Claxton K. Country-level cost-effectiveness thresholds: initial estimates and the need for further research. Value in Health. 2016;19:929–35.
Ochalek J, Lomas J, Claxton K. Estimating health opportunity costs in low-income and middle-income countries: a novel approach and evidence from cross-country data. BMJ Glob Health. 2018;3: e000964.
Edoka IP, Stacey NK. Estimating a cost-effectiveness threshold for health care decision-making in South Africa. Health Policy Plan. 2020;35:546–55.
Haacker M, Fraser-Hurt N, Gorgens M. Effectiveness of and financial returns to voluntary medical male circumcision for HIV prevention in South Africa: an incremental cost-effectiveness analysis. PLoS Med. 2016;13: e1002012.
Kripke K, Chen P-A, Vazzano A, et al. Cost and impact of voluntary medical male circumcision in South Africa: focusing the program on specific age groups and provinces. PLoS ONE. 2016;11: e0157071.
Kripke K, Vazzano A, Kirungi W, et al. Modeling the impact of Uganda’s safe male circumcision program: implications for age and regional targeting. PLoS ONE. 2016;11: e0158693.
Kripke K, Perales N, Lija J, et al. The economic and epidemiological impact of focusing voluntary medical male circumcision for HIV prevention on specific age groups and regions in Tanzania. PLoS ONE. 2016;11: e0153363.
Voetsch AC, Duong YT, Stupp P, et al. HIV-1 recent infection testing algorithm with antiretroviral drug detection to improve accuracy of incidence estimates. J Acquir Immune Defic Syndr. 2021;87:S73–80.
Sartorius B, VanderHeide JD, Yang M, et al. Subnational mapping of HIV incidence and mortality among individuals aged 15–49 years in Sub-Saharan Africa, 2000–18: a modelling study. Lancet HIV. 2021;8:e363–75.
Njeuhmeli E, Schnure M, Vazzano A, Gold E, Stegman P, Kripke K, Tchuenche M, Bollinger L, Forsythe S, Hankins C. Using mathematical modeling to inform health policy: a case study from voluntary medical male circumcision scale-up in eastern and southern Africa and proposed framework for success. PLoS ONE. 2019;14: e0213605.
• Torres-Rueda S, Wambura M, Weiss HA, et al. Cost and cost-effectiveness of a demand creation intervention to increase uptake of voluntary medical male circumcision in Tanzania: spending more to spend less. JAIDS J Acquir Immune Defic Syndr. 2018;78:291–9. Torres-Rueda et al. analyzed the effect of demand creation (mass media, community mobilization, and targeted service delivery) on VMMC cost and cost-effectiveness compared to standard of care in a randomized controlled trial. They found that demand creation reduced the cost per VMMC by increasing client volumes at service delivery points, making VMMC more cost-effective.
Bekker L-G, Alleyne G, Baral S, et al. Advancing global health and strengthening the HIV response in the era of the Sustainable Development Goals: the International AIDS Society—Lancet Commission. Lancet. 2018;392:312–58.
Kong X, Kigozi G, Ssekasanvu J, et al. Association of medical male circumcision and antiretroviral therapy scale-up with community HIV incidence in Rakai, Uganda. JAMA. 2016;316:182.
Borgdorff MW, Kwaro D, Obor D, et al. HIV incidence in western Kenya during scale-up of antiretroviral therapy and voluntary medical male circumcision: a population-based cohort analysis. Lancet HIV. 2018;5:e241–9.
Cork MA, Wilson KF, Perkins S, et al. Mapping male circumcision for HIV prevention efforts in Sub-Saharan Africa. BMC Med. 2020;18:189.
Ehrenkranz P, Rosen S, Boulle A, Eaton JW, Ford N, Fox MP, Grimsrud A, Rice BD, Sikazwe I, Holmes CB. The revolving door of HIV care: revising the service delivery cascade to achieve the UNAIDS 95–95-95 goals. PLoS Med. 2021;18: e1003651.
Stegman PM, Yee R, Davis J, Tchuenche M, Linder R, Zembe L, Frescura L, Kripke KE. Estimating male circumcision coverage in 15 priority countries in Sub-Saharan Africa. J Int AIDS Soc. 2021;24: e25789.
World Health Organization. Models to inform fast tracking voluntary medical male circumcision in HIV combination prevention: report from World Health Organization and UNAIDS meeting, 23–24 March 2016. Geneva: Switzerland; 2017.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Anna Bershteyn received grants to their institution from the US National Institutes of Health and the Bill and Melinda Gates Foundation. Katharine Kripke received grant to her institution from UNAIDS. Edinah Mudimu, Ingrida Platais, Samuel Mwalili, James E. Zulu, and Wiza N. Mwanza declare that they have no conflicts of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Voluntary Medical Male Circumcision: Progress and Challenges
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bershteyn, A., Mudimu, E., Platais, I. et al. Understanding the Evolving Role of Voluntary Medical Male Circumcision as a Public Health Strategy in Eastern and Southern Africa: Opportunities and Challenges. Curr HIV/AIDS Rep 19, 526–536 (2022). https://doi.org/10.1007/s11904-022-00639-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11904-022-00639-5