Abstract
This review examines the current evidence for associations between vertebral fractures (VFx), the most common type of fracture in older adults, and trunk muscles, which are intimately tied to spinal loading and function. Individuals with prevalent VFxs have more fat infiltration in the trunk muscles, lower trunk extension strength, and altered muscle activation patterns. However, no longitudinal studies have examined whether assessment of trunk muscle can contribute to prediction of fracture risk. A few studies report that exercise interventions targeting the trunk muscles can reduce the risk of VFx, improve trunk strength and endurance in patients who have had a VFx, and reduce the risk of falling, a common cause of VFx, but the quality of evidence is low. Trunk muscles likely have an important role to play in prediction, prevention, and management of VFx, but additional longitudinal studies and randomized controlled trials are needed to clarify this role.


Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005–2025. J Bone Miner Res. 2007;22(3):465–75.
Christiansen BA, Bouxsein ML. Biomechanics of vertebral fractures and the vertebral fracture cascade. Curr Osteoporos Rep. 2010;8(4):198–204.
Schousboe JT. Epidemiology of vertebral fractures. J Clin Densitom. 2016;19(1):8–22.
Johansson H, Odén A, McCloskey EV, Kanis JA. Mild morphometric vertebral fractures predict vertebral fractures but not non-vertebral fractures. Osteoporos Int. 2014;25(1):235–41.
Cooper C, Atkinson EJ, O’Fallon WM, Melton LJ. Incidence of clinically diagnosed vertebral fractures: a population-based study in Rochester, Minnesota, 1985–1989. J Bone Miner Res. 1992;7(2):221–7.
Freitas SS, Barrett-Connor E, Ensrud KE, Fink HA, Bauer DC, Cawthon PM, et al. Rate and circumstances of clinical vertebral fractures in older men. Osteoporos Int. 2008;19(5):615–23.
Mitchell WK, Williams J, Atherton P, Larvin M, Lund J, Narici M. Sarcopenia, dynapenia, and the impact of advancing age on human skeletal muscle size and strength; a quantitative review. Front Physiol. 2012;3:1–19.
Delmonico MJ, Harris TB, Visser M, Park SW, Conroy MB, Velasquez-Mieyer P, et al. Longitudinal study of muscle strength, quality, and adipose tissue infiltration. Am J Clin Nutr. 2009;90(6):1579–85.
Singh DKA, Bailey M, Lee R. Ageing modifies the fibre angle and biomechanical function of the lumbar extensor muscles. Clin Biomech. 2011;26(6):543–7.
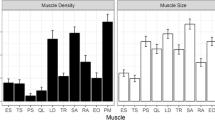
Anderson DE, D’Agostino JM, Bruno AG, Demissie S, Kiel DP, Bouxsein ML. Variations of CT-based trunk muscle attenuation by age, sex, and specific muscle. J Gerontol Ser A Biol Sci Med Sci. 2013;68(3):317–23.
Rahemi H, Nigam N, Wakeling JM. The effect of intramuscular fat on skeletal muscle mechanics: implications for the elderly and obese. J Roy Soc Int. 2015;12(109):20150365.
Quirk DA, Hubley-kozey CL. Age-related changes in trunk neuromuscular activation patterns during a controlled functional transfer task include amplitude and temporal synergies. Hum Mov Sci Elsev BV. 2014;38:262–80.
Arjmand N, Shirazi-Adl A. Model and in vivo studies on human trunk load partitioning and stability in isometric forward flexions. J Biomech. 2006;39(3):510–21.
Dreischarf M, Aboulfazl SA, Arjmand N, Rohlmann A, Schmidt H. Estimation of loads on human lumbar spine: a review of in vivo and computational model studies. J Biomech. 2015. doi:10.1016/j.jbiomech.2015.12.038.
Kalaci A, Duru M, Karazincir S, Sevinç TT, Kuvandik G, Balci A. Thoracic spine compression fracture during isoniazid-induced seizures: case report. Pediatr Emerg Care. 2008;24(12):842–4.
Youssef JA, McCullen GM, Brown CC. Seizure-induced lumbar burst fracture. Spine. 1995;20(11):1301–3.
Takahashi T, Tominaga T, Shamoto H, Shimizu H, Yoshimoto T. Seizure-induced thoracic spine compression fracture: case report. Surg Neurol. 2002;58(3):214–7.
Majkowska L, Waliłko E, Molęda P, Bohatyrewicz A. Thoracic spine fracture in the course of severe nocturnal hypoglycemia in young patients with type 1 diabetes mellitus—the role of low bone mineral density. Am J Emerg Med. 2014;32(7):816.e5–7.
Katzman W, Cawthon P, Hicks GE, Vittinghoff E, Shepherd J, Cauley JA, et al. Association of spinal muscle composition and prevalence of hyperkyphosis in healthy community-dwelling older men and women. J Gerontol Med Sci. 2012;67A(2):191–5.
Mika A, Unnithan VB, Mika P. Differences in thoracic kyphosis and in back muscle strength in women with bone loss due to osteoporosis. Spine. 2005;30(2):241–6.
Miyakoshi N, Hongo M, Maekawa S, Ishikawa Y, Shimada Y, Okada K, et al. Factors related to spinal mobility in patients with postmenopausal osteoporosis. Osteoporos Int. 2005;16(12):1871–4.
Rubenstein LZ. Falls in older people: epidemiology, risk factors and strategies for prevention. Age Ageing. 2006;35 Suppl 2:ii37–41.
Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas. 2013;75(1):51–61.
Avin KG, Bloomfield SA, Gross TS, Warden SJ. Biomechanical aspects of the muscle-bone interaction. Curr Osteoporos Rep. 2014;13(1):1–8.
Frost HM. Bone “mass” and the “mechanostat”: a proposal. Anat Rec. 1987;219(1):1–9.
Frost HM. Skeletal structural adaptations to mechanical usage (SATMU): 2. Redefining Wolff’s law: the remodeling problem. Anat Rec. 1990;226(4):414–22.
Liu CC, Theodorou DJ, Theodorou SJ, Andre MP, Sartoris DJ, Szollar SM, et al. Quantitative computed tomography in the evaluation of spinal osteoporosis following spinal cord injury. Osteoporos Int. 2000;11(10):889–96.
Dinç H, Savci G, Demirci A, Sadikoğlu MY, Tuncel E, Yavuz H. Quantitative computed tomography for measuring bone mineral density in athletes. Calcif Tissue Int. 1996;58(6):398–401.
Raguso CA, Kyle U, Kossovsky MP, Roynette C, Paoloni-Giacobino A, Hans D, et al. A 3-year longitudinal study on body composition changes in the elderly: role of physical exercise. Clin Nutr. 2006;25(4):573–80.
Anderson DE, D’Agostino JM, Bruno AG, Manoharan RK, Bouxsein ML. Regressions for estimating muscle parameters in the thoracic and lumbar trunk for use in musculoskeletal modeling. J Biomech. 2012;45(1):66–75.
Hicks GE, Simonsick EM, Harris TB, Newman AB, Weiner DK, Nevitt MA, et al. Trunk muscle composition as a predictor of reduced functional capacity in the health, aging and body composition study: the moderating role of back pain. J Gerontol A Biol Sci Med Sci. 2005;60(11):1420–4.
Hicks GE, Simonsick EM, Harris TB, Newman AB, Weiner DK, Nevitt MA, et al. Cross-sectional associations between trunk muscle composition, back pain, and physical function in the health, aging and body composition study. J Gerontol A Biol Sci Med Sci. 2005;60:882–7.
Tanner RK, Gore CJ. Physiological tests for elite athletes, 2nd ed. Champaign, IL: Human Kinetics; 2013.
Singh DKA, Bailey M, Lee R. Decline in lumbar extensor muscle strength the older adults: correlation with age, gender and spine morphology. BMC Musculoskelet Disord. 2013;14(1):215.
Sinaki M, Nwaogwugwu NC, Phillipls BE, Mokri MP. Effect of gender, age, and anthropometry on axial and appendicular muscle strength. Am J Phys Med Rehabil. 2001;80(5):330–8.
Reid KF, Fielding RA. Skeletal muscle power: a critical determinant of physical functioning in older adults. Exerc Sport Sci Rev. 2012;40(1):4–12.
Skelton DA. Explosive power and asymmetry in leg muscle function in frequent fallers and non-fallers aged over 65. Age Ageing. 2002;31(2):119–25.
Biering-Sørensen F. Physical measurements as risk indicators for low-back trouble over a one-year period. Spine. 1984;9(2):106–19.
Moffroid MT. Endurance of trunk muscles in persons with chronic low back pain: assessment, performance, training. J Rehabil Res Dev. 1997;34:440–7.
Parikh CM, Arora M. Lower trunk muscle endurance and core testing: a literature review. Int J Ther Rehabil Res. 2015;4(4):55–60.
Shipp KM, Purse JL, Gold DT, Pieper CF, Sloane R, Schenkman M, et al. Timed loaded standing: a measure of combined trunk and arm endurance suitable for people with vertebral osteoporosis. Osteoporos Int. 2000;11(11):914–22.
Kienbacher T, Paul B, Habenicht R, Starek C, Wolf M, Kollmitzer J, et al. Age and gender related neuromuscular changes in trunk flexion-extension. J Neuroeng Rehabil. 2015;12(1):1–10.
Kanis JA, Johnell O, Oden A, Johansson H, McCloskey E. FRAX™ and the assessment of fracture probability in men and women from the UK. Osteoporos Int. 2008;19(4):385–97.
Hong W, Cheng Q, Zhu X, Zhu H, Li H, Zhang X, et al. Prevalence of sarcopenia and its relationship with sites of fragility fractures in elderly Chinese men and women. PLoS One. 2015;10(9):e0138102.
Lau EM, Chan HH, Woo J, Sham A, Leung PC. Body composition and bone mineral density of Chinese women with vertebral fracture. Bone. 1996;19(6):657–62.
Takata S, Ikata T, Yonezu H. Characteristics of regional bone mineral density and soft tissue composition in patients with atraumatic vertebral fractures. J Bone Miner Metab. 2000;18(5):287–90.
Kaji H, Tobimatsu T, Naito J, Iu M-F, Yamauchi M, Sugimoto T, et al. Body composition and vertebral fracture risk in female patients treated with glucocorticoid. Osteoporos Int. 2006;17(4):627–33.
Anderson D, Allaire B, Bruno A, Demissie S, Kiel D, Bouxsein M. Low trunk muscle density is associated with prevalent vertebral fractures in older adults. J Bone Miner Res. 2013;28(Suppl 1). Available at http://www.asbmr.org/education/AbstractDetail?aid=1d255c1e-30c6-425e-81b1-29c7d681b5f9. Accessed October 8, 2015.
So KY, Kim DH, Choi DH, Kim CY, Kim JS, Choi YS. The influence of fat infiltration of back extensor muscles on osteoporotic vertebral fractures. Asian Spine J. 2013;7(4):308–13.
Kim DH, Choi DH, Park JH, Lee JH, Choi YS. What is the effect of spino-pelvic sagittal parameters and back muscles on osteoporotic vertebral fracture? Asian Spine J. 2015;9(2):162–9. This case-control study examined of the cross-sectional relationship of spino-pelvic sagittal parameters and MRI-based measures of back muscles with prevalent osteoporotic VFx. Showed that fat infiltration of back extensor muscle was associated with VFx independent of age, BMD, and spino-pelvic postural measures. This provides strong motivation for continued investigation of how trunk muscle composition relates to VFx.
Pfeifer M, Begerow B, Minne HW, Schlotthauer T, Pospeschill M, Scholz M, et al. Vitamin D status, trunk muscle strength, body sway, falls, and fractures among 237 postmenopausal women with osteoporosis. Exp Clin Endocrinol Diabetes. 2001;109(2):87–92.
Sinaki M, Wollan PC, Scott RW, Gelczer RK. Can strong back extensors prevent vertebral fractures in women with osteoporosis? Mayo Clin Proc. 1996;71(10):951–6.
Briggs AM, Greig AM, Bennell KL, Hodges PW. Paraspinal muscle control in people with osteoporotic vertebral fracture. Eur Spine J. 2007;16(8):1137–44.
Greig AM, Briggs AM, Bennell KL, Hodges PW. Trunk muscle activity is modified in osteoporotic vertebral fracture and thoracic kyphosis with potential consequences for vertebral health. PLoS One. 2014;9(10):e109515. This cross-sectional study assessed trunk muscle EMG in older adults with and without VFx. VFx subjects presented more co-contraction of agonist and antagonist trunk muscles during forward arm movements, and lower extensor activation during backward arm movements, which may represent attempts to increase stability and reduce spinal loading, respectively. This supports the need to further study how neuromuscular control may relate to VFx prediction, prevention and management.
Cawthon PM, Blackwell TL, Marshall LM, Fink HA, Kado DM, Ensrud KE, et al. Physical performance and radiographic and clinical vertebral fractures in older men. J Bone Miner Res. 2014;29(9):2101–8.
Granacher U, Gollhofer A, Hortobágyi T, Kressig RW, Muehlbauer T. The importance of trunk muscle strength for balance, functional performance, and fall prevention in seniors: a systematic review. Sport Med. 2013;43(7):627–41. This systematic review highlights the association of trunk muscle strength/trunk muscle composition with balance, physical function and falls in older adults. Although the mean Physiotherapy Evidence Database (PEDro) quality scale was low, authors recommend core strength training and/or Pilates training as “feasible exercise programs for seniors with high-adherence rates” to reduce risk of fall.
Kasukawa Y, Miyakoshi N, Hongo M, Ishikawa Y, Noguchi H, Kamo K, et al. Relationships between falls, spinal curvature, spinal mobility and back extensor strength in elderly people. J Bone Miner Metab. 2010;28(1):82–7.
Imagama S, Ito Z, Wakao N, Seki T, Hirano K, Muramoto A, et al. Influence of spinal sagittal alignment, body balance, muscle strength, and physical ability on falling of middle-aged and elderly males. Eur Spine J. 2013;22:1346–53.
Anderson DE, Quinn E, Parker E, Allaire BT, Muir JW, Rubin CT, et al. Associations of computed tomography-based trunk muscle size and density with balance and falls in older adults. J Gerontol Med Sci. 2015. doi:10.1093/gerona/glv185. This study is the first to assess the relationship of baseline CT-based trunk muscle size and density measurements with incident falls during a median 2 years follow up. While higher trunk muscle density was cross-sectionally associated with reduced postural sway in both sexes at baseline, it was not prognostic of incident falls, but larger muscle size at baseline was associated with increased postural sway for both sexes, and with a greater likelihood of falling in men. This somewhat unexpected finding highlights the complex but likely important relationship between trunk muscle and balance and falls.
Helbostad JL, Sturnieks DL, Menant J, Delbaere K, Lord SR, Pijnappels M. Consequences of lower extremity and trunk muscle fatigue on balance and functional tasks in older people: a systematic literature review. BMC Geriatr. 2010;10(1):56.
Sinaki M. Exercise for patients with osteoporosis: management of vertebral compression fractures and trunk strengthening for fall prevention. PM&R Elsevier Inc. 2012;4(11):882–8.
Cosman F, De Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, Randall S, et al. Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int. 2014;25(10):2359–81.
Kemmler W, Engelke E, Von Stengel S. Long-term exercise and bone mineral density changes in postmenopausal women-are there periods of reduced effectiveness? J Bone Miner Res. 2015. doi:10.1002/jbmr.2608.
Giangregorio LM, Papaioannou A, MacIntyre NJ, Ashe MC, Heinonen A, Shipp K, et al. Too fit to fracture: exercise recommendations for individuals with osteoporosis or osteoporotic vertebral fracture. Osteoporos Int. 2014;25(3):821–35.
Sinaki M, Itoi E, Wahner HW, Wollan P, Gelzcer R, Mullan BP, et al. Stronger back muscles reduce the incidence of vertebral fractures: a prospective 10 year follow-up of postmenopausal women. Bone. 2002;30(6):836–41.
Sinaki M, Mikkelsen BA. Postmenopausal spinal osteoporosis: flexion versus extension exercises. Arch Phys Med Rehabil. 1984;65(10):593–6.
Gillespie LD, Robertson MC, Gillespie WJ, Sherrington C, Gates S, Clemson LM, et al. Interventions for preventing falls in older people living in the community. Cochrane Datab Syst Rev. 2012;9:CD007146.
Irez GB, Ozdemir RA, Evin R, Irez SG, Korkusuz F. Integrating Pilates exercise into an exercise program for 65+ year-old women to reduce falls. J Sport Sci Med. 2011;10(1):105–11.
Lenchik L, Rogers LF, Delmas PD, Genant HK. Diagnosis of osteoporotic vertebral fractures: importance of recognition and description by radiologists. Am J Roentgenol. 2004;183(4):949–58.
Bennett DL, Post RD. The role of the radiologist when encountering osteoporosis in women. Am J Roentgenol. 2011;196(2):331–7.
Giangregorio LM, Macintyre NJ, Thabane L, Skidmore CJ, Papaioannou A. Exercise for improving outcomes after osteoporotic vertebral fracture (review). Cochrane Collab. 2013;1–50. A systematic review of the benefits and harms of exercise interventions in post-VFx individuals identified seven randomized controlled trials with 488 participants. Five of the seven directly targeted trunk muscles, and while some trials reported beneficial effects of exercise in VFx patients, variability in outcomes prevented much pooling of results. This review notes that overall quality of evidence is low, and that no studies to date have assessed incident falls, incident VFx, or other adverse events. Thus this strongly supports the need for high quality randomized controlled trials to assess the safety and efficacy of exercise for VFx prevention and management.
Gold DT, Shipp KM, Pieper CF, Duncan PW, Martinez S, Lyles KW. Group treatment improves trunk strength and psychological status in older women with vertebral fractures: results of a randomized, clinical trial. J Am Geriatr Soc. 2004;52(9):1471–8.
Bennell KL, Matthews B, Greig A, Briggs A, Kelly A, Sherburn M, et al. Effects of an exercise and manual therapy program on physical impairments, function and quality-of-life in people with osteoporotic vertebral fracture: a randomised, single-blind controlled pilot trial. BMC Musculoskelet Disord. 2010;11(1):36.
Bergland A, Thorsen H, Kåresen R. Effect of exercise on mobility, balance, and health-related quality of life in osteoporotic women with a history of vertebral fracture: a randomized, controlled trial. Osteoporos Int. 2011;22(6):1863–71.
Bergström I, Bergström K, Kronhed ACG, Karlsson S, Brinck J. Back extensor training increases muscle strength in postmenopausal women with osteoporosis, kyphosis and vertebral fractures. Adv Physiother. 2011;13(3):110–7.
Papaioannou A, Adachi JD, Winegard K, Ferko N, Parkinson W, Cook RJ, et al. Efficacy of home-based exercise for improving quality of life among elderly women with symptomatic osteoporosis-related vertebral fractures. Osteoporos Int. 2003;14(8):677–82.
Malmros B, Mortensen L, Jensen MB, Charles P. Positive effects of physiotherapy on chronic pain and performance in osteoporosis. Osteoporos Int. 1998;8(3):215–21.
Yang L, He CQ, Xie W, Lan Q. Effect of pain-free exercises on female osteoporosis patients with spinal compressive fracture. J Clin Rehabil Tissue Eng Res. 2007;11(45):9108–11.
Wong CC, McGirt MJ. Vertebral compression fractures: a review of current management and multimodal therapy. J Multidiscip Healthc. 2013;6:205–14.
Valentin GH, Pedersen LN, Maribo T. Wearing an active spinal orthosis improves back extensor strength in women with osteoporotic vertebral fractures. Prosthet Orthot Int. 2014;38(3):232–8.
Pfeifer M, Begerow B, Minne HW. Effects of a new spinal orthosis on posture, trunk strength, and quality of life in women with postmenopausal osteoporosis: a randomized trial. Am J Phys Med Rehabil. 2004;83(3):177–86.
Pfeifer M, Kohlwey L, Begerow B, Minne HW. Effects of two newly developed spinal orthoses on trunk muscle strength, posture, and quality-of-life in women with postmenopausal osteoporosis: a randomized trial. Am J Phys Med Rehabil. 2011;90(10):805–15.
Dionyssiotis Y, Trovas G, Thoma S, Lyritis G, Papaioannou N. Prospective study of spinal orthoses in women. Prosthet Orthot Int. 2015;39(6):487–95.
Barker KL, Javaid MK, Newman M, Minns Lowe C, Stallard N, Campbell H, et al. Physiotherapy rehabilitation for osteoporotic vertebral fracture (PROVE): study protocol for a randomized controlled trial. Trials. 2014;15(1):22. This paper presents the protocol for an ongoing RCT of 600 people with clinically diagnosed VFxs to study the effectiveness of exercise-based physiotherapy (including spine extensor and stabilization exercises), a manual therapy-based physiotherapy, or usual care. The primary outcomes will be Quality of Life and trunk muscle endurance (i.e. TLS) test outcomes at 1 year, and importantly incident VFx and falls will also be assessed, providing needed information on safety and whether these interventions may help in VFx prevention.
Giangregorio LM, Thabane L, Adachi JD, Ashe MC, Bleakney RR, Braun EA, et al. Build better bones with exercise: protocol for a feasibility study of a multicenter randomized controlled trial of 12 months of home exercise in women with a vertebral fracture. Phys Ther. 2014;94(9):1337–52. This paper presents the protocol for a pilot multicenter RCT recruiting 160 women aged ≥65 years with a prevalent VFx, examining the effect of an exercise intervention group compared with controls receiving equal attention but no exercise advice. The intervention involves personalized and progressive exercises (at least three times a week) targeting lower limb strength, balance, posture, upper extremity strength and endurance Trunk extensor muscle endurance (via TLS test) will be assessed at two study sites. Importantly incident VFx and falls will also be assessed, providing needed information on safety and whether the intervention may help in VFx prevention.
Acknowledgments
This work was supported by NIH grants R01 AR053986 and R00 AG042458.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
H. Mokhtarzadeh declares that he has no conflict of interest. D. E. Anderson declares that he has no conflict of interest.
Human and Animal Rights and Informed Consent
All studies by D. E. Anderson involving animal and/or human subjects were performed after approval by the appropriate institutional review boards. When required, written informed consent was obtained from all participants.
Additional information
This article is part of the Topical Collection on Imaging
Rights and permissions
About this article
Cite this article
Mokhtarzadeh, H., Anderson, D.E. The Role of Trunk Musculature in Osteoporotic Vertebral Fractures: Implications for Prediction, Prevention, and Management. Curr Osteoporos Rep 14, 67–76 (2016). https://doi.org/10.1007/s11914-016-0305-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11914-016-0305-4