Abstract
Background
Hypocapnia induces cerebral vasoconstriction leading to a decrease in cerebral blood flow, which might precipitate cerebral ischemia. Hypocapnia can be intentional to treat intracranial hypertension or unintentional due to a spontaneous hyperventilation (SHV). SHV is frequent after subarachnoid hemorrhage. However, it is understudied in patients with severe traumatic brain injury (TBI). The objective of this study was to describe the incidence and consequences on outcome of SHV after severe TBI.
Methods
We conducted a retrospective, observational study including all intubated TBI patients admitted in the trauma center and still comatose 24 h after the withdrawal of sedation. SHV was defined by the presence of at least one arterial blood gas (ABG) with both PaCO2 < 35 mmHg and pH > 7.45. Patient characteristics and outcome were extracted from a prospective registry of all intubated TBI admitted in the intensive care unit. ABG results were retrieved from patient files. A multivariable logistic regression model was developed to determine factors independently associated with unfavorable outcome (defined as a Glasgow Outcome Scale between 1 and 3) at 6-month follow-up.
Results
During 7 years, 110 patients fully respecting inclusion criteria were included. The overall incidence of SHV was 69.1% (95% CI [59.9–77]). Patients with SHV were more severely injured (median head AIS score (5 [4–5] vs. 4 [4–5]; p = 0.016)) and exhibited an elevated morbidity during their stay. The proportion of patients with an unfavorable functional neurologic outcome was significantly higher in patients with SHV: 40 (52.6%) versus 6 (17.6%), p = 0.0006. After adjusting for confounders, SHV remains an independent factor associated with unfavorable outcome at the 6-month follow-up (OR 4.1; 95% CI [1.2–14.4]).
Conclusions
SHV is common in patients with a persistent coma after a severe TBI (overall rate: 69%) and was independently associated with unfavorable outcome at 6-month follow-up.
Similar content being viewed by others
Background
Carbon dioxide is a powerful modulator of the cerebral vasculature [1, 2]. Hypocapnia induces cerebral vasoconstriction leading to a decrease in cerebral blood flow (CBF) and a consequent decrease in intracranial pressure (ICP) [1, 3, 4]. Thus, in the past, intentional hyperventilation has been proposed as a treatment for intracranial hypertension (ICH) in patients with traumatic brain injury (TBI) [5, 6]. However, numerous recent studies demonstrated an association between hypocapnia and worse functional neurologic outcome [7,8,9,10]. In fact, hyperventilation induced reductions in CBF compromise oxidative metabolism, increase cerebral oxygen extraction, and then may precipitate or worsen cerebral ischemia [4, 9, 11,12,13]. It is for these reasons that current French and International guidelines advocate the avoidance of prolonged prophylactic hyperventilation, particularly during the first 24 h when CBF is more frequently already impaired [14,15,16,17]. Hyperventilation can be used as a temporizing measure for elevated ICP, ideally under the supervision of cerebral oxygenation monitoring (brain tissue oxygen tension [PbtO2] or jugular bulb venous oxygen saturation [SjO2]) [14].
Central or neurogenic spontaneous hyperventilation (SHV) is frequent after a brain injury [18,19,20,21]. SHV can also occur in patients with severe TBI still comatose after the withdrawal of sedation. SHV leads to hypocapnia despite minimal or absent ventilator support and may have potential deleterious consequences. However, very little is known about its incidence or effects on functional neurologic outcomes.
The aim of this study was to determine the frequency of SHV in severe TBI patients still comatose after the withdrawal of sedation and its association with worse outcomes. We hypothesized that SHV is associated with poor neurological functional outcome at 6 months after the trauma.
Patients and Methods
Study Design and Patient Selection
This 7-year retrospective, observational, single-center study was conducted at the Sainte Anne Military Hospital of Toulon (France). Patients with severe TBIs were eligible when they were intubated and admitted to the intensive care unit (ICU) between January 2007 and December 2013. Inclusion criteria were: age ≥ 18 years; severe TBI with a Glasgow Coma Scale (GCS) score ≤ 8 after initial resuscitation; still comatose 24 h after the withdrawal of sedation. Patients were excluded when they died before the withdrawal of sedation, had quick extubation (within 6 h) after the withdrawal of sedation, or no arterial blood gas (ABG) results available in the wake-up period.
All patients were sedated, intubated, and mechanically ventilated in accordance with international guidelines [17]. The institutional therapeutic management approach is presented in Fig. 1 and remained constant throughout the study period.
The Institutional Review Board approved the study and waived the requirement for informed consent from patients and their relatives, given the observational nature of the study.
Definition and Diagnosis of Spontaneous Hyperventilation (SHV)
ABG results were retrieved from patient files for all included subjects during a 7-day period after the withdrawal of sedation. Included subjects had to have at least one ABG that was obtained while ventilated in a pressure support ventilation (PSV) mode or not mechanically ventilated (through a T-tube or extubation). ABGs were collected before or following a delay of at least 30 min after nursing care or other painful procedure.
SHV was defined by the presence of at least one ABG with both PaCO2 < 35 mmHg and pH > 7.45. Severe SHV was defined by the presence of both PaCO2 < 30 mmHg and pH > 7.50. Patients with SHV not meeting the requirement for severe SHV were considered to have moderate SHV [21].
Data Collected
We accessed a registry of data prospectively collected on all patients intubated for TBIs and admitted to the ICU. The registry reported data on patient characteristics, mechanism of injury, pre-hospital assessment, whole-body computed tomography scan results, evolution in the ICU, in-hospital mortality, and neurologic functional outcome at 6 months according to the Glasgow Outcome Scale (GOS). The GOS score is a 5-point scale, where 1 = death, 2 = persistent vegetative state, 3 = severe disability, 4 = moderate disability, and 5 = good recovery [22]. A senior intensivist or a senior physical medicine and rehabilitation physician assessed the GOS by clinic visits (preferentially) or a phone call to patient or relatives with standardized, structured interviews [23].
Endpoints
The primary endpoint of the study was the GOS at 6 months post-TBI, which was prospectively collected in our registry. GOS was dichotomized to unfavorable neurological functional outcome (GOS between 1 and 3) and favorable outcome (GOS 4 and 5). Secondary endpoints were in-hospital length of stay and in-hospital mortality.
Statistical Analysis
All statistical analyses were performed with XLSTAT, version 2015.3.01 (Addinsoft, Paris, France). Continuous data are reported as the mean ± SD. Data that were not normally distributed are expressed as the median and interquartile range [25th–75th percentiles]. Nominal variables are reported as number and proportions (%).
To compare differences in baseline characteristics and evolution between the groups of patients with and without SHV, the χ2 test or Fisher’s exact test was used for categorical variables, and the Mann–Whitney test or Student t test was used for continuous variables, as appropriate.
To examine association between SHV and unfavorable functional neurologic outcome (GOS 1–3), we used a simple logistic regression. All parameters with p value < 0.1 in the simple logistic regression analysis were included in multivariable logistic regression model to identify independent factors associated with an unfavorable neurologic outcome at 6 months. The Hosmer–Lemeshow goodness-of-fit test and the area under the receiver operating characteristic (ROC) curve were used to evaluate the overall final model fit and the model discrimination, respectively. To detect multicollinearity, we calculated the Variance Inflation Factors of each variable included in the model. Final model results were expressed as the odds ratio (OR) and 95% confidence intervals (95% CI). For all tests, a two-side p < 0.05 was considered statistically significant.
Results
Study Population
During the study period, 228 patients with severe TBIs were admitted to the ICU. One-hundred and eighteen patients were excluded, due to death while sedated (n = 45), rapid awakening after withdrawal of sedation (n = 36), no ABG available (n = 34), no evaluation of the 6-month GOS (n = 3) (Fig. 2). Among the 110 patients included in the study, the most common mechanism of injury was a motorcycle crash (31%). There were 85 male (77%) and 25 female (23%) patients. These patients had a median age of 38 [22–60] years, a median injury severity score of 23 [16–29], a median abbreviated injury scale (AIS) score for head injury of 5 [4–5], and a median minimal GCS score of 6 [4–8].
Spontaneous Hyperventilation
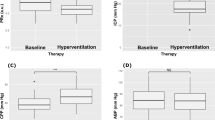
We collected a total of 473 ABGs: 381 (67.2%) during PSV mode and 155 (32.8%) without mechanical ventilation. The median level of support was 12 cmH2O (10–14), and the median tidal volume was 7.3 ml/kg (6.2–9.1) (Additional Table).
SHV was diagnosed in 76 patients with severe TBIs still comatose after the withdrawal of sedation (overall incidence, 69.1%; 95% CI [59.9–77]). The SHV started within the 3 days after the withdrawal of sedation for 72 patients (95%) (2 patients developed SHV at day 4 and 2 patients at day 7). SHV started at a median of 11 (7–16) days after the TBI. Twenty-five of 76 patients with SHV (32.9%) were classified as having a severe SHV. The remaining 51 (67.1%) were considered to have moderate SHV.
At the onset of SHV, 35 patients (46.1%) had an ongoing infection (31 early- or late-onset ventilator-associated pneumonia [88.6%] and 4 nosocomial meningitis [11.4%]). Eighteen of them (49.6%) were already treated with antibiotics for more than 48 h before the start of SHV.
General characteristics of patients with SHV are compared to those without SHV in Table 1. In comparisons of patients without SHV, those with SHV had a more severe TBI, in terms of median initial GCS score (6 [4–8] vs. 8 [6–10]; p = 0.006), rate of pupillary abnormality (46.1% vs. 14.7%; p = 0.002), and median head AIS score (5 [4–5] vs. 4 [4–5]; p = 0.016). There were no significant differences in age, gender, injury severity score, and thoracic AIS score.
SVH patients were significantly more likely to experience at least one episode of ICH before the withdrawal of sedation (52.6% vs. 23.5%, p = 0.005), and thus, they more frequently received therapeutic hypothermia (50% vs. 23.5%, p = 0.009), barbiturate infusion (18.4% vs. 8.8%, p = 0.015), and/or decompressive craniectomy (31.6% vs. 2.9%, p = 0.001).
Functional Neurologic Outcome at 6 months
The GOS score distribution was more favorable among patients without SHV (p = 0.0007) (Fig. 3). Based on our dichotomization, the proportion of patients with an unfavorable functional neurologic outcome was significantly higher in patients with SHV: 40 (52.6%) versus 6 (17.6%), p = 0.0006.
Functional neurologic outcomes at 6 months after traumatic brain injury according to the presence of spontaneous hyperventilation. Shown is the distribution of scores on the Glasgow Outcome Scale at 6 months. Scores range from 1 to 5, with 1 indicating death, 2 persistent vegetative state, 3 severe disability, 4 moderate disability, and 5 good recovery. There was a significant difference between groups in the overall distribution of scores (p = 0.0007). SHV spontaneous hyperventilation
In simple logistic regression analysis, we found that patients with SHV had five times the odds of unfavorable outcome (OR 5.2; 95% CI [1.9–14]). Other factors significantly associated with unfavorable outcome were age above 65 years (OR 4.7; 95% CI [1.6–13.3]), minimal GCS score < 6 (OR 3; 95% CI [1.4–6.7]), pupillary abnormalities (OR 5.6; 95% CI [2.4–13]), Marshall category ≥ 3 (OR 4; 95% CI [1.8–8.9]), and hypernatremia (> 155 mEq/L) (OR 2.7; 95% CI [1.2–6.3] (Table 2).
After adjustment in the multivariable logistic regression model, SHV remained significantly associated with unfavorable outcome (OR 4.1; 95% CI [1.2–14.4]). Other variables included in the model are shown in Table 3. The area under the ROC curve was 0.84. The Hosmer–Lemeshow test demonstrated a good model fit (χ2 = 9.8, df = 8, p = 0.28).
Others Endpoints
Patients that developed SHV exhibited elevated morbidity during their stay (Table 1). Notably, compared to patients without SHV, those with SHV had significantly longer sedation durations (9 [4–14] days vs. 3.5 [2–6.5] days, p = 0.0002), significantly longer mechanical ventilation durations (14.5 [10–21] days vs. 5.5 [4–10] days, p < 0.0001), and significantly longer hospital lengths of stay (33 [25–49] days vs. 14 [10–32] days, p = 0.0001). In-hospital mortality was not different: 7 (9.2%) vs. 3 (8.8%), p = 1.00.
Discussion
This retrospective analysis of a prospective observational cohort of 110 patients with severe TBIs still comatose after interruption of sedation showed a high occurrence of SHV (approximately of 69%) including almost 33% of severe SHV. This occurrence is consistent with similar findings in other types of brain injury [20, 21]. Notably, in subarachnoid hemorrhage (SAH), the frequency of SHV varies from 55 to 92% [20, 21]. The pathophysiology of this condition after TBI is not completely established, but multiples hypotheses can be discussed. First, TBI may induce SHV by disrupting the cortical inhibition on the brainstem respiratory centers, liberating them and thereby triggering hyperventilation [24]. Second, SHV may be a part of the paroxysmal sympathetic hyperactivity (PSH), which is also associated elevated heart rate, elevated blood pressure, hyperthermia, and sweating [25]. PSH is common in neurointensive care units, with a reported prevalence ranging from 8 to 33% [25]. Finally, SHV could be simply due to other factors indirectly related to the TBI and its care, such as pain, discomfort from endotracheal tube, fever due to infection or analgesic and sedative drugs withdrawal syndrome.
The second and probably main finding of the present work is the independent association between SHV and unfavorable functional neurologic outcome at 6 months. Indeed, severe TBI patients developing SHV had four times the odds of unfavorable outcome. However, whether the SHV just reflected severity of cerebral damage or contributed to its aggravation is still unclear. It is well established that hypocapnia, especially if it occurs in the first days following the TBI, is associated with unfavorable outcome by causing or aggravating brain ischemia [4, 9]. Indeed, hypocapnia results in a cerebrospinal fluid alkalosis triggering multiples neurologic effects [4, 26]. Firstly, cerebrospinal fluid alkalosis reduces CBF and, to a lesser extent, cerebral blood volume via cerebral arterial vasoconstriction, leading to a decrease in oxygen delivery [4, 9, 12]. In patients with TBI, CBF decreases by approximately 3% per mm Hg change in PaCO2 [27]. Coles et al. [12] demonstrated that an induced moderate hypocapnia (from 36 to 29 mm Hg) significantly reduces global CBF (from 31 to 23 mL/100 g/min) and results in a significant increase in the volume of critically hypoperfused tissue. However, some studies have demonstrated that prolonged hyperventilation is associated with a tachyphylaxis of the effect of hypocapnia and, therefore, prolonged cerebral arterial vasoconstriction may be unlikely [28]. Secondly, hypocapnia increases cerebral oxygen demand through an increased neuronal excitability or induction of seizures [13, 29]. In 2007, Coles and colleagues using positron emission tomography and somatosensory evoked potentials showed that hypocapnia is associated with an increase in cerebral oxygen metabolism (CMRO2) [13]. Both of these mechanisms (i.e., decreased oxygen delivery by reduction of CBF and increased CMRO2) deteriorate the flow–metabolism balance and may contribute to a switch to anaerobic metabolism or, even worse, precipitate a brain ischemia, especially in regions with preexisting impairment of CBF [4, 12, 13]. Finally, cerebrospinal fluid alkalosis may induce neurotoxicity, notably by the production of excitatory amino acids, like N-methyl-d-aspartate, that are locally cytotoxic [30, 31].
Although patients with SHV have more severe disease in the present work (in terms of initial GCS score, rate of pupillary abnormalities, need for advanced therapeutics as decompressive craniotomy or barbiturate infusion), two elements may argue in favor of a direct negative impact of SHV on outcome. Firstly, after adjustment on age and markers of TBI severity in the multivariable analysis, SHV remains associated with unfavorable functional neurologic outcome at 6 months. Secondly, Carrera et al. [32] demonstrated that SHV may negatively affect brain tissue oxygenation monitored with brain tissue oxygen tension (PbtO2) in patients with severe brain injury (SAH, intracranial hemorrhage, or TBI). Compared with normocapnia, the percentage of hourly data with PbtO2 < 15 mm Hg was significantly higher for patients with hypocapnia (15.7% in patients with normal EtCO2 to 33.9% in patients with EtCO2 < 25 mm Hg). Moreover, EtCO2 and PbtO2 were strongly correlated in patients with TBI. It was already proved that a PbtO2 < 15 mm Hg is associated with an increased risk of brain ischemia leading to secondary cerebral insults and, therefore, poor functional neurologic outcome [33, 34]. Thus, the work of Carrera et al. supports our opinion that SHV may induce cerebral hypoxic events that may alter the prognosis.
Even if the present work demonstrated an independent association between SHV and poor functional neurologic outcome, further studies are necessary to determine whether a treatment of SHV is effective or leads to improved outcome. Overall, the level of evidence is too low to recommend any intervention to treat SHV. Moreover, therapeutic options in this kind of patients to minimize hyperventilation are limited, either mechanical by adding dead space to the ventilator circuit in order to reduce hypocapnia, or pharmacological with sedatives, opioids or more specific molecules acting on the PSH like α2 agonists (clonidine for example) [25]. However, both of these options have side effects like an increase in the work of breathing or an interference with clinical monitoring [25, 35].
Study Limitations
Our study had several limitations. First, it was a single-center study; therefore, the results are not generalizable to all patient populations. Second, since this is an observational study, it was not possible to account for all confounders leading to an association between SHV and unfavorable functional neurologic outcome. Nonetheless, the final logistical regression model included most of the well-established parameters classically associated with poor outcome (age, GCS score, radiological severity with Marshall category etc.). Additionally, given the historic nature of the data, it is possible that temporal changes in clinical practice may have impacted the results. For example, over the course of the time frame of the study, practitioners became more aware of the potential adverse effects of SHV, leading to increased usage of medications targeting PSH (propranolol, clonidine), since PSH was thought to cause some cases of SHV. Thus, the incidence of SHV and its consequences could have been artificially decreased. Finally, we excluded patients quickly extubated after the withdrawal of sedation. This leads to a very high occurrence of SHV (69.1%; 95% CI [59.9–77]). However, we hope that this study may help clinicians to determine which patients will have a poor outcome, and this question seems more relevant in patients still comatose after the initial phase of TBI.
Conclusions
The present work showed that patients with severe TBI had a high incidence of SHV. We found that SHV starts quickly after the withdrawal of sedation for the majority of patients. In addition, our results suggested that SHV was associated with an unfavorable functional neurologic outcome.
Abbreviations
- TBI:
-
Traumatic brain injury
- GCS:
-
Glasgow Coma Scale
- CPP:
-
Cerebral perfusion pressure
- PbtO2 :
-
Brain tissue oxygen tension
- ICU:
-
Intensive care unit
- ICP:
-
Intracranial pressure
- FiO2 :
-
Oxygen inspired fraction
- GOS:
-
Glasgow Outcome Scale
- ROC:
-
Receiver operating characteristic
- 95% CI:
-
95% confidence intervals
References
Madden JA. The effect of carbon dioxide on cerebral arteries. Pharmacol Ther. 1993;59(2):229–50.
Ito H, Ibaraki M, Kanno I, Fukuda H, Miura S. Changes in the arterial fraction of human cerebral blood volume during hypercapnia and hypocapnia measured by positron emission tomography. J Cereb Blood Flow Metab. 2005;25(7):852–7.
Raichle ME, Plum F. Hyperventilation and cerebral blood flow. Stroke. 1972;3(5):566–75.
Curley G, Kavanagh BP, Laffey JG. Hypocapnia and the injured brain: more harm than benefit. Crit Care Med. 2010;38(5):1348–59.
Ghajar J, Hariri RJ, Narayan RK, Iacono LA, Firlik K, Patterson RH. Survey of critical care management of comatose, head-injured patients in the United States. Crit Care Med. 1995;23(3):560–7.
Neumann JO, Chambers IR, Citerio G, Enblad P, Gregson BA, Howells T, et al. The use of hyperventilation therapy after traumatic brain injury in Europe: an analysis of the BrainIT database. Intensive Care Med. 2008;34(9):1676–82.
Muizelaar JP, Marmarou A, Ward JD, Kontos HA, Choi SC, Becker DP, et al. Adverse effects of prolonged hyperventilation in patients with severe head injury: a randomized clinical trial. J Neurosurg. 1991;75(5):731–9.
Dumont TM, Visioni AJ, Rughani AI, Tranmer BI, Crookes B. Inappropriate prehospital ventilation in severe traumatic brain injury increases in-hospital mortality. J Neurotrauma. 2010;27(7):1233–41.
Godoy DA, Seifi A, Garza D, Lubillo-Montenegro S, Murillo-Cabezas F. Hyperventilation therapy for control of posttraumatic intracranial hypertension. Front Neurol. 2017;8:250.
Roberts BW, Karagiannis P, Coletta M, Kilgannon JH, Chansky ME, Trzeciak S. Effects of PaCO2 derangements on clinical outcomes after cerebral injury: a systematic review. Resuscitation. 2015;27:1–48.
Stringer WA, Hasso AN, Thompson JR, Hinshaw DB, Jordan KG. Hyperventilation-induced cerebral ischemia in patients with acute brain lesions: demonstration by xenon-enhanced CT. AJNR Am J Neuroradiol. 1993;14(2):475–84.
Coles JP, Minhas PS, Fryer TD, Smielewski P, Aigbirihio F, Donovan T, et al. Effect of hyperventilation on cerebral blood flow in traumatic head injury: clinical relevance and monitoring correlates. Crit Care Med. 2002;30(9):1950–9.
Coles JP, Fryer TD, Coleman MR, Smielewski P, Gupta AK, Minhas PS, et al. Hyperventilation following head injury: effect on ischemic burden and cerebral oxidative metabolism. Crit Care Med. 2007;35(2):568–78.
Carney N, Totten AM, O’Reilly C, Ullman JS, Hawryluk GWJ, Bell MJ, et al. Guidelines for the management of severe traumatic brain injury, fourth edition. Neurosurgery. 2017;80:6–15.
Geeraerts T, Velly L, Abdennour L, Asehnoune K, Audibert G, Bouzat P, et al. Management of severe traumatic brain injury (first 24 hours). Anaesth Crit Care Pain Med. 2018;37(2):171–86.
Marehbian J, Muehlschlegel S, Edlow BL, Hinson HE, Hwang DY. Medical management of the severe traumatic brain injury patient. Neurocrit Care. 2017;30:1–17.
Brain Trauma Foundation, American Association of Neurological Surgeons, Congress of Neurological Surgeons. Guidelines for the management of severe traumatic brain injury. J Neurotrauma. 2007;24:S1–106.
Gaviani P, Gonzalez RG, Zhu J-J, Batchelor TT, Henson JW. Central neurogenic hyperventilation and lactate production in brainstem glioma. Neurology. 2005;64(1):166–7.
Møller K, Høgh P, Larsen FS, Strauss GI, Skinhøj P, Sperling BK, et al. Regional cerebral blood flow during hyperventilation in patients with acute bacterial meningitis. Clin Physiol. 2000;20(5):399–410.
Solaiman O, Singh JM. Hypocapnia in aneurysmal subarachnoid hemorrhage: incidence and association with poor clinical outcomes. J Neurosurg Anesthesiol. 2013;25(3):254–61.
Williamson CA, Sheehan KM, Tipirneni R, Roark CD, Pandey AS, Thompson BG, et al. The association between spontaneous hyperventilation, delayed cerebral ischemia, and poor neurological outcome in patients with subarachnoid hemorrhage. Neurocrit Care. 2015;23(3):330–8.
Jennett B, Bond M. Assessment of outcome after severe brain damage. Lancet. 1975;1(7905):480–4.
Fayol P, Carrière H, Habonimana D, Preux P-M, Dumond J-J. French version of structured interviews for the Glasgow Outcome Scale: guidelines and first studies of validation. Ann Readapt Med Phys. 2004;47(4):142–56.
Leitch AG, McLennan JE, Balkenhol S, Loudon RG, McLaurin RL. Mechanisms of hyperventilation in head injury: case report and review. Neurosurgery. 1979;5(6):701–7.
Meyfroidt G, Baguley IJ, Menon DK. Paroxysmal sympathetic hyperactivity: the storm after acute brain injury. Lancet Neurol. 2017;16(9):721–9.
Kontos HA, Raper AJ, Patterson JL. Analysis of vasoactivity of local pH, PCO2 and bicarbonate on pial vessels. Stroke. 1977;8(3):358–60.
Alberti E, Hoyer S, Hamer J, Stoeckel H, Packschiess P, Weinhardt F. The effect of carbon dioxide on cerebral blood flow and cerebral metabolism in dogs. Br J Anaesth. 1975;47(9):941–7.
Muizelaar JP, van der Poel HG, Li ZC, Kontos HA, Levasseur JE. Pial arteriolar vessel diameter and CO2 reactivity during prolonged hyperventilation in the rabbit. J Neurosurg. 1988;69(6):923–7.
Huttunen J, Tolvanen H, Heinonen E, Voipio J, Wikström H, Ilmoniemi RJ, et al. Effects of voluntary hyperventilation on cortical sensory responses. Electroencephalographic and magnetoencephalographic studies. Exp Brain Res. 1999;125(3):248–54.
Graham EM, Apostolou M, Mishra OP, Delivoria-Papadopoulos M. Modification of the N-methyl-d-aspartate (NMDA) receptor in the brain of newborn piglets following hyperventilation induced ischemia. Neurosci Lett. 1996;218(1):29–32.
Mykita S, Golly F, Dreyfus H, Freysz L, Massarelli R. Effect of CDP-choline on hypocapnic neurons in culture. J Neurochem. 1986;47(1):223–31.
Carrera E, Schmidt JM, Fernandez L, Kurtz P, Merkow M, Stuart M, et al. Spontaneous hyperventilation and brain tissue hypoxia in patients with severe brain injury. J Neurol Neurosurg Psychiatry. 2010;81(7):793–7.
Valadka AB, Gopinath SP, Contant CF, Uzura M, Robertson CS. Relationship of brain tissue PO2 to outcome after severe head injury. Crit Care Med. 1998;26(9):1576–81.
van Santbrink H, Maas AI, Avezaat CJ. Continuous monitoring of partial pressure of brain tissue oxygen in patients with severe head injury. Neurosurgery. 1996;38(1):21–31.
Haberthür C, Fabry B, Stocker R, Ritz R, Guttmann J. Additional inspiratory work of breathing imposed by tracheostomy tubes and non-ideal ventilator properties in critically ill patients. Intensive Care Med. 1999;25(5):514–9.
Funding
None.
Author information
Authors and Affiliations
Contributions
PE, JR, and CJ contributed to the study concept and design. PE, JR, MC, ED, AM, PJC, and AS contributed to the acquisition of data. PE, PG, AD, and BP contributed to the analysis and interpretation of data. PE, PG, JB, and EM contributed to the drafting of manuscript and critical revision of the manuscript for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to report.
Ethical Approval and Consent to Participate
Institutional Review Board of the Sainte Anne Military Hospital, Toulon (France), approved the study and waived the requirement for informed consent from the patients or patient’s kin given the observational nature of the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
12028_2018_639_MOESM1_ESM.docx
Additional Table. Comparison between Arterial Blood Gas with Spontaneous Hyperventilation criteria and those without. (DOCX 12 kb)
Rights and permissions
About this article
Cite this article
Esnault, P., Roubin, J., Cardinale, M. et al. Spontaneous Hyperventilation in Severe Traumatic Brain Injury: Incidence and Association with Poor Neurological Outcome. Neurocrit Care 30, 405–413 (2019). https://doi.org/10.1007/s12028-018-0639-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-018-0639-0