Abstract
Background and Purpose
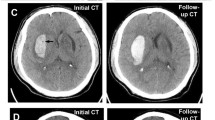
The computed tomography angiography (CTA) spot sign is widely used to assess the risk of hematoma expansion following acute intracerebral hemorrhage (ICH). However, not all patients can receive intravenous contrast nor are all hospital systems equipped with this technology. We aimed to independently validate the Hematoma Expansion Prediction (HEP) Score, an 18-point non-contrast prediction scale, in an external cohort and compare its diagnostic capability to the CTA spot sign.
Methods
We performed a retrospective analysis of the predicting hematoma growth and outcome in intracerebral hemorrhage using contrast bolus CT (PREDICT) Cohort Study. Primary outcome was significant hematoma expansion (≥ 6 mL or ≥ 33%). We generated a receiver operating characteristic (ROC) curve comparing the HEP score to significant expansion. We calculated sensitivity, specificity, positive and negative predictive values (PPV/NPV) for each score point. We determined independent predictors of significant hematoma expansion via logistic regression.
Results
A total of 292 patients were included in primary analysis. Hematoma growth of ≥ 6 mL or ≥ 33% occurred in 94 patients (32%). The HEP score was associated with significant expansion (adjusted odds ratio [aOR] 1.14, 95% confidence interval [CI] 1.01–1.30). ROC curves comparing HEP score to significant expansion had an area under the curve of 0.64 (95% CI 0.57–0.71). Youden’s method showed an optimum score of 4. HEP Scores ≥ 4 (n = 100, sensitivity 49%, specificity 73%, PPV 46%, NPV 75%, aOR 1.99, 95% CI 1.09–3.64) accurately predicted significant expansion. PPV increased with higher HEP scores, but at the cost of lower sensitivity. The diagnostic characteristics of the spot sign (n = 82, Sensitivity 49%, Specificity 81%, PPV 55%, NPV 76%, aOR 2.95, 95% CI 1.61–5.42) were similar to HEP scores ≥ 4.
Conclusion
The HEP score is predictive of significant expansion (≥ 6 mL or ≥ 33%) and is comparable to the spot sign in diagnostic accuracy. Non-contrast prediction tools may have a potential role in the recruitment of patients in future intracerebral hemorrhage trials.

Similar content being viewed by others
References
Qureshi AI, Mendelow AD, Hanley DF. Intracerebral haemorrhage. Lancet (London, England). 2009;373(9675):1632–44.
Gonzales NR. Ongoing clinical trials in intracerebral hemorrhage. Stroke. 2013;44(6 Suppl 1):S70–3.
VanDerWerf J, Kurowski D, Siegler J, Ganguly T, Cucchiara B. Combination of intra-hematomal hypodensity on CT and BRAIN scoring improves prediction of hemorrhage expansion in ICH. Neurocrit Care. 2018;29:40–6.
Morotti A, Dowlatshahi D, Boulouis G, et al. Predicting intracerebral hemorrhage expansion with noncontrast computed tomography: the BAT Score. Stroke. 2018;49(5):1163–9.
Huynh TJ, Aviv RI, Dowlatshahi D, et al. Validation of the 9-point and 24-Point Hematoma Expansion Prediction Scores and derivation of the PREDICT A/B Scores. Stroke. 2015;46(11):3105–10.
Delgado Almandoz JE, Yoo AJ, Stone MJ, et al. The spot sign score in primary intracerebral hemorrhage identifies patients at highest risk of in-hospital mortality and poor outcome among survivors. Stroke. 2010;41(1):54–60.
Wang X, Arima H, Al-Shahi Salman R, et al. Clinical prediction algorithm (BRAIN) to determine risk of hematoma growth in acute intracerebral hemorrhage. Stroke. 2015;46(2):376–81.
Yao X, Xu Y, Siwila-Sackman E, Wu B, Selim M. The HEP Score: a nomogram-derived Hematoma Expansion Prediction Scale. Neurocrit Care. 2015;23(2):179–87.
Meretoja A, Churilov L, Campbell BCV, et al. The spot sign and tranexamic acid on preventing ICH growth–AUStralasia Trial (STOP-AUST): protocol of a phase II randomized, placebo-controlled, double-blind, multicenter trial. Int J Stroke. 2014;9(4):519–24.
Demchuk AM, Dowlatshahi D, Rodriguez-Luna D, et al. Prediction of haematoma growth and outcome in patients with intracerebral haemorrhage using the CT-angiography spot sign (PREDICT): a prospective observational study. Lancet Neurol. 2012;11(4):307–14.
Dowlatshahi D, Demchuk AM, Flaherty ML, et al. Defining hematoma expansion in intracerebral hemorrhage: relationship with patient outcomes. Neurology. 2011;76(14):1238–44.
Royston P, Ambler G, Sauerbrei W. The use of fractional polynomials to model continuous risk variables in epidemiology. Int J Epidemiol. 1999;28(5):964–74.
Al-Shahi Salman R, Frantzias J, Lee RJ, et al. Absolute risk and predictors of the growth of acute spontaneous intracerebral haemorrhage: a systematic review and meta-analysis of individual patient data. Lancet Neurol. 2018;17(10):885–94.
DeLong ER, DeLong DM, Clarke-Pearson DL. Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 1988;44(3):837–45.
Dowlatshahi D, Smith EE, Flaherty ML, et al. Small intracerebral haemorrhages are associated with less haematoma expansion and better outcomes. Int J Stroke. 2011;6(3):201–6.
Dowlatshahi D, Yogendrakumar V, Aviv RIRI, et al. Small intracerebral hemorrhages have a low spot sign prevalence and are less likely to expand. Int J Stroke. 2016;11(2):191–7.
Schlegel D, Kolb SJ, Luciano JM, et al. Utility of the NIH Stroke Scale as a predictor of hospital disposition. Stroke. 2003;34(1):134–7.
Balami JS, Buchan AM. Complications of intracerebral haemorrhage. Lancet Neurol. 2012;11(1):101–18.
Kazui S, Naritomi H, Yamamoto H, Sawada T, Yamaguchi T. Enlargement of spontaneous intracerebral hemorrhage. Incidence and time course. Stroke. 1996;27(10):1783–7.
Brott T, Broderick J, Kothari R, et al. Early hemorrhage growth in patients with intracerebral hemorrhage. Stroke. 1997;28(1):1–5.
Kuramatsu JB, Gerner ST, Schellinger PD, et al. Anticoagulant reversal, blood pressure levels, and anticoagulant resumption in patients with anticoagulation-related intracerebral hemorrhage. JAMA. 2015;313(8):824–36.
Cordonnier C, Leys D, Dumont F, et al. What are the causes of pre-existing dementia in patients with intracerebral haemorrhages? Brain. 2010;133(11):3281–9.
Rodrigues MA, Samarasekera N, Lerpiniere C, et al. The Edinburgh CT and genetic diagnostic criteria for lobar intracerebral haemorrhage associated with cerebral amyloid angiopathy: model development and diagnostic test accuracy study. Lancet Neurol. 2018;17(3):232–40.
Boulouis G, Morotti A, Charidimou A, Dowlatshahi D, Goldstein JN. Noncontrast computed tomography markers of intracerebral hemorrhage expansion. Stroke. 2017;48(4):1120–5.
Broderick JP, Brott TG, Duldner JE, Tomsick T, Huster G. Volume of intracerebral hemorrhage. A powerful and easy-to-use predictor of 30-day mortality. Stroke. 1993;24(7):987–93.
Funding
There was no support for this work.
Author information
Authors and Affiliations
Consortia
Contributions
This manuscript complies with the instructions provided by Neurocritical Care. All authors meet the requirements for authorship. Their roles and contributions to this manuscript are listed below: VY and DD were involved in protocol/project development, data analysis, and manuscript writing/editing. TR contributed to data analysis and manuscript writing/editing. AMD, RIA, DR-L, CAM, YSB, ID, AK, J-MB, CL, GG, PS, JR, CSK, RB were involved in data collection or management. MDH contributed to data collection or management and manuscript writing/editing. DF contributed to manuscript writing/editing. MS was involved in protocol/project development and manuscript writing/editing.
Corresponding author
Ethics declarations
Conflicts of Interest
Andrew M. Demchuk reports grants from NovoNordisk Canada, during the conduct of the study; Jean-Martin Boulanger reports other from Pfizer, other from Novartis, outside the submitted work; Cheemun Lum has deceased; Michael D. Hill reports personal fees from Merck, non-financial support from Hoffmann-La Roche Canada Ltd, grants from Covidien (Medtronic), grants from Boehringer-Ingleheim, grants from Stryker Inc., grants from Medtronic LLC, grants from NoNO Inc., outside the submitted work; In addition, Hill has a patent Systems and Methods for Assisting in Decision-Making and Triaging for Acute Stroke Patients pending to US Patent office Number: 62/086,077 and owns stock in Calgary Scientific Incorporated, a company that focuses on medical imaging software, is a director of the Canadian Federation of Neurological Sciences, a not-for-profit group and has received grant support from Alberta Innovates Health Solutions, CIHR, Heart & Stroke Foundation of Canada, National Institutes of Neurological Disorders and Stroke; Magdy Selim reports grants from NIH/NINDS, during the conduct of the study and the remaining authors have nothing to disclose.
Ethical approval/Informed consent
Local research ethics board approval was obtained at all enrolling sites, and written informed consent was obtained from all participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yogendrakumar, V., Ramsay, T., Fergusson, D.A. et al. Independent Validation of the Hematoma Expansion Prediction Score: A Non-contrast Score Equivalent in Accuracy to the Spot Sign. Neurocrit Care 31, 1–8 (2019). https://doi.org/10.1007/s12028-019-00740-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-019-00740-5