Abstract
Background
Cerebral edema is associated with worse outcome after acute stroke; however, the minimum clinically relevant threshold remains unknown. This study aimed to identify the minimal degree of midline shift (MLS) that predicts outcome in a cohort encompassing a broad range of patients with acute stroke.
Methods
Patient-level data from six acute stroke clinical trials were combined with endovascular thrombectomy registries from two academic referral centers, generating a combined cohort of 1977 patients. MLS was extracted from the original trial data or measured on computed tomography or magnetic resonance imaging that was obtained a median of 47.0 h (interquartile range 27.0–75.1 h) after stroke onset. Logistic regression was performed to identify predictors of poor outcome and the minimal clinically relevant MLS threshold.
Results
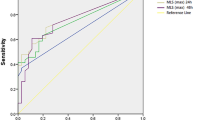
The presence of MLS was a predictor of poor outcome, independent of baseline clinical and demographic factors (adjusted odds ratio 4.46, 95% confidence interval 3.56–5.59, p < 0.001). Examining the full range of MLS values identified, a value of greater than 3 mm was the critical threshold that significantly predicted poor outcome (adjusted odds ratio 3.20 [1.31–7.82], p = 0.011).
Conclusions
These results show that the presence of MLS predicts poor outcome and, specifically, MLS value greater than 3 mm is an important threshold across a variety of clinical settings. These findings may have relevance for the design and interpretation of future trials for antiedema therapies.


Similar content being viewed by others
References
Kimberly WT, Dutra BG, Boers AMM, et al. Association of reperfusion with brain edema in patients with acute ischemic stroke: a secondary analysis of the MR CLEAN trial. JAMA Neurol. 2018;75(4):1–9.
Battey TWK, Karki M, Singhal AB, et al. Brain edema predicts outcome after nonlacunar ischemic stroke. Stroke. 2014;45(12):3643–8.
Vorasayan P, Bevers MB, Beslow LA, et al. Intravenous glibenclamide reduces lesional water uptake in large hemispheric infarction. Stroke. 2019;50(11):3021–7.
Minnerup J, Broocks G, Kalkoffen J, et al. Computed tomography–based quantification of lesion water uptake identifies patients within 4.5 hours of stroke onset: a multicenter observational study. Ann Neurol. 2016;80(6):924–34.
Dhar R, Yuan K, Kulik T, et al. CSF Volumetric analysis for quantification of cerebral edema after hemispheric infarction. Neurocrit Care. 2016;24(3):420–7.
Harston GWJ, Carone D, Sheerin F, Jenkinson M, Kennedy J. Quantifying infarct growth and secondary injury volumes: comparing multimodal image registration measures. Stroke. 2018;49(7):1647–55.
Ropper AH. Lateral displacement of the brain and level of consciousness in patients with an acute hemispheral mass. N Engl J Med. 1986;314(15):953–8.
Davis SM, Donnan GA, Parsons MW, et al. Effects of alteplase beyond 3 h after stroke in the echoplanar imaging thrombolytic evaluation trial (EPITHET): a placebo-controlled randomised trial. Lancet Neurol. 2008;7(4):299–309.
The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med. 1995;333(24):1581–7.
Kidwell CS, Jahan R, Gornbein J, et al. A trial of imaging selection and endovascular treatment for ischemic stroke. N Engl J Med. 2013;368(10):914–23.
Sheth KN, Elm JJ, Molyneaux BJ, et al. Safety and efficacy of intravenous glyburide on brain swelling after large hemispheric infarction (GAMES-RP): a randomised, double-blind, placebo-controlled phase 2 trial. Lancet Neurol. 2016;15(11):1160–9.
Kimberly WT, Bevers MB, Demchuk AM, et al. Effect of IV glyburide on adjudicated edema endpoints in the GAMES-RP Trial. Neurology. 2018;91:e2163–9.
Torbey MT, Bösel J, Rhoney DH, et al. Evidence-based guidelines for the management of large hemispheric infarction: a statement for health care professionals from the Neurocritical Care Society and the German Society for Neuro-Intensive Care and Emergency Medicine. Neurocrit Care. 2015;22(1):146–64.
Ong CJ, Gluckstein J, Laurido-Soto O, Yan Y, Dhar R, Lee JM. Enhanced detection of edema in malignant anterior circulation stroke (EDEMA) score. Stroke. 2017;48(7):1969–72.
Fung C, Murek M, Z’Graggen WJ, et al. Decompressive hemicraniectomy in patients with supratentorial intracerebral hemorrhage. Stroke. 2012;43(12):3207–11.
Thomalla G, Hartmann F, Juettler E, et al. Prediction of malignant middle cerebral artery infarction by magnetic resonance imaging within 6 hours of symptom onset: a prospective multicenter observational study. Ann Neurol. 2010;68(4):435–45.
Irvine HJ, Ostwaldt A-C, Bevers MB, et al. Reperfusion after ischemic stroke is associated with reduced brain edema. J Cereb Blood Flow Metab. 2018;38(10):1807–17.
Bevers MB, Battey TWK, Ostwaldt A-C, et al. Apparent diffusion coefficient signal intensity ratio predicts the effect of revascularization on ischemic cerebral edema. Cerebrovasc Dis. 2018;45(3–4):93–100.
Carney N, Totten AM, O’Reilly C, et al. Guidelines for the management of severe traumatic brain injury. Neurosurgery. 2017;80(1):6–15.
Scheulin KM, Jurgielewicz BJ, Spellicy SE, et al. Exploring the predictive value of lesion topology on motor function outcomes in a porcine ischemic stroke model. Sci Rep. 2021;11(1):3814.
Funding
This work was funded by NIH K23NS112474 (MBB), AAN CRTS AI18-0000000062 (MBB), NIH R01 NS099209 (WTK), and AHA 20SRG35540018 (WTK).
Author information
Authors and Affiliations
Contributions
MEM contributed for Data acquisition, data analysis, primary drafting of manuscript; AP, JK and IT contributed for Data acquisition and analysis; SBS, CK, BCVC, SMD, GAD, ML, KNS and NP contributed for Data analysis, critical revision of manuscript for intellectual content; WTK contributed for Study conception, critical revision of manuscript for intellectual content; and MBB contributed for Study conception, data acquisition, data analysis, critical revision of manuscript for intellectual content.
Corresponding author
Ethics declarations
Conflicts of interest
Dr. Bevers reports current grants from NIH K23NS112474 and AAN CRTS AI18-0000000062; in addition, Dr. Bevers reports prior grants from Andrew David Heitman Neurovascular fund, and prior grants and personal fees from Biogen, personal fees from Atlas Ventures, and personal fees from Dynamed. Dr. Kimberly reports grants from NIH R01 NS099209 and grants AHA 20SRG35540018 related to the current work; in addition, Dr. Kimberly reports grants and personal fees from Biogen, and grants and personal fees from NControl Therapeutics outside the submitted work; in addition, Dr. Kimberly has a patent to PCT/US2018/018537 pending and licensed. Dr. Sheth reports grants from Biogen, AHA, Hyperfine, NIH, Novartis and Bard. He reports consulting fees from NControl Therapeutics and Zoll, outside the submitted work. He is on a data safety monitoring board for Zoll. He has patents for wearables and nanoparticles, unrelated to the submitted work. Dr. Sheth reports stock options in Alva Health. Dr. Lev reports grants from GE Heathcare and Siemens Healthcare. He reports consulting fees from GE Healthcare and Takea/Roche-Genentech outside the submitted work. He reports patents pending in Electrical Impedance Spectroscopy and machine learning for computed tomography scan lesion detection. All other authors report no disclosures.
Ethical approval/informed consent
Applicable institutional review board approval was obtained for access to data from all underlying studies and registries used in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
W. Taylor Kimberly and Matthew B. Bevers are co-senior authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
McKeown, M.E., Prasad, A., Kobsa, J. et al. Midline Shift Greater than 3 mm Independently Predicts Outcome After Ischemic Stroke. Neurocrit Care 36, 46–51 (2022). https://doi.org/10.1007/s12028-021-01341-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-021-01341-x