Abstract
The purpose of this consensus paper is to review electrophysiological abnormalities and to provide a guideline of neurophysiological assessments in cerebellar ataxias. All authors agree that standard electrophysiological methods should be systematically applied in all cases of ataxia to reveal accompanying peripheral neuropathy, the involvement of the dorsal columns, pyramidal tracts and the brainstem. Electroencephalography should also be considered, although findings are frequently non-specific. Electrophysiology helps define the neuronal systems affected by the disease in an individual patient and to understand the phenotypes of the different types of ataxia on a more general level. As yet, there is no established electrophysiological measure which is sensitive and specific of cerebellar dysfunction in ataxias. The authors agree that cerebellar brain inhibition (CBI), which is based on a paired-pulse transcranial magnetic stimulation (TMS) paradigm assessing cerebellar-cortical connectivity, is likely a useful measure of cerebellar function. Although its role in the investigation and diagnoses of different types of ataxias is unclear, it will be of interest to study its utility in this type of conditions. The authors agree that detailed clinical examination reveals core features of ataxia (i.e., dysarthria, truncal, gait and limb ataxia, oculomotor dysfunction) and is sufficient for formulating a differential diagnosis. Clinical assessment of oculomotor function, especially saccades and the vestibulo-ocular reflex (VOR) which are most easily examined both at the bedside and with quantitative testing techniques, is of particular help for differential diagnosis in many cases. Pure clinical measures, however, are not sensitive enough to reveal minute fluctuations or early treatment response as most relevant for pre-clinical stages of disease which might be amenable to study in future intervention trials. The authors agree that quantitative measures of ataxia are desirable as biomarkers. Methods are discussed that allow quantification of ataxia in laboratory as well as in clinical and real-life settings, for instance at the patients’ home. Future studies are needed to demonstrate their usefulness as biomarkers in pharmaceutical or rehabilitation trials.
Similar content being viewed by others
Introduction
A large number of heterogeneous disorders are encapsulated by the term “ataxias.” In daily praxis, it is often difficult to isolate a specific subtype of ataxia only from clinical examination. The aim of this consensus paper is to propose guidelines for neurophysiological assessments for the diagnostic work-up of ataxias. We also address the question whether neurophysiological assessments may be useful biomarkers to monitor disease course and the effects of emerging treatments.
Broadly, primary ataxias are distinguished from secondary or acquired ataxias. Primary ataxias are subdivided into sporadic and hereditary ataxias [1]. Hereditary ataxias include autosomal recessive cerebellar ataxias (ARCA), autosomal dominant cerebellar ataxias (ADCA, spinocerebellar ataxias or SCAs), episodic ataxias (EA), X-linked ataxias, and mitochondrial ataxias. Currently, there are more than 40 types of SCAs described, with SCA3 the most common form worldwide. SCA types 1, 2, 6, and 7 are the next most common types, whereas the other SCA genotypes represent a group of rare diseases, some described in single families. Friedreich’s ataxia (FRDA) is autosomal recessively inherited and is the most frequent form of hereditary ataxia in the western world. The number of recessive ataxias with known disease genes is currently fast growing [2]. Additionally, congenital ataxias can be caused by cerebellar malformations or pontocerebellar hypoplasia, most commonly related to genetic causes. Finally, there is overlap between ataxias and complex types of hereditary spastic paraplegias (HSP) [3]. Sporadic degenerative ataxias include multiple system atrophy (MSA—cerebellar type), and sporadic adult onset ataxia of unknown etiology (SAOA) [4]. Secondary or acquired ataxias are due to exogenous or endogenous generally non-genetic causes, including toxic, paraneoplastic, immune-mediated, nutritional, and infectious [1].
Common clinical features in patients with ataxias are imbalance, incoordination, and often impaired speech. Degeneration involves the cerebellar parenchyma and/or cerebellar afferent and efferent pathways as well as cortical, subcortical, and peripheral segments of the nervous system (the involvement of which can further refine diagnostic considerations). Accompanying derangement of the vestibular system, pyramidal tracts, brainstem nuclei, and basal ganglia, among others, are frequently present in ataxias. Furthermore, large- and small-fiber polyneuropathy are very common. In fact, extracerebellar involvement is the rule in ataxias, and pure cerebellar disorders are the exception. As balance requires both cerebellar and extracerebellar structures, extracerebellar involvement may be the primary driver of disordered balance and incoordination, e.g., in FRDA. Cerebellar nuclei and spinocerebellar tracts are involved in FRDA. FRDA, however, is a predominantly sensory ataxia due to early and pronounced affection of the dorsal root ganglia, dorsal columns, and sensory polyneuropathy [5]. In addition, most patients with FRDA develop significant pyramidal tract symptoms further impairing truncal stability.
The sine qua non in the diagnostic work-up of ataxias is the demonstration of cerebellar dysfunction, which may be challenging at disease onset given the insidious and slowly progressive nature of many ataxias. Next, consider whether the patient has significant extracerebellar involvement; this would sharpen phenotypic or syndromic considerations, winnowing a broad differential, and focus further genetic testing. Ataxia panels and exome analyses are increasingly used to diagnose hereditary ataxias [6]. They do have their limitations and pitfalls, and to analyze a limited number of target genes increases the sensitivity of genetic testing. In addition, there is growing demand for sensitive biomarkers to monitor the course of the disease and effects of treatment in upcoming interventional trials.
Neurophysiological assessments are often equated with electrophysiological assessments, that is, nerve conduction studies, electromyography (EMG), sensory and motor evoked potentials (SEP, MEP), and electroencephalography (EEG). These are routine procedures and are widely available in neurology departments. Electrophysiological methods are useful to detect extracerebellar involvement including polyneuropathy, dorsal columns, pyramidal tracts, brainstem involvement, and accompanying epilepsy. None of these measures, however, allow demonstration or quantification of cerebellar involvement, the core problem in most types of ataxias. The assessment of cerebellar brain inhibition (CBI) using transcranial magnetic stimulation (TMS) is the only exception. CBI, however, has not been systematically applied in ataxias, and is not part of the diagnostic routine.
The consensus paper has two parts. In the first part, we will discuss findings of electrophysiological studies in ataxias. In the second part, we will discuss the clinical assessment of the core symptoms of cerebellar disease and make reference to possible quantitative measures. For instance, imbalance in gait and stance is often the presenting but non-specific complaint of patients referred to a neurologist for an evaluation for a cerebellar ataxia syndrome. Bedside teaching of the neurological examination traditionally focuses on gross deficits such as tremor, muscle weakness, and impaired sensation. Abnormalities of eye movements may be less apparent but are often the key to localization and etiology. Another complicating feature is that normal balance requires efficient operation of many different cortical, subcortical, and infratentorial systems. These include foundational structural elements (skeletal system integrity and axial weight-bearing muscle power), primary sensory (afferent sensory proprioception and semicircular canal- and otolith-mediated vestibular responses), higher-order/multimodal cerebral integrative and associative circuits that mediate volition, motivation and agency, and finally corrective structures (basal ganglia and cerebellum) that gate activity and ensure that movements are accurate [7]. In contrast to the assessment of gait and balance impairments, the assessment of eye movement impairments can contribute more to differential diagnosis, showing distinct impairment for different types of ataxia [8]. While quantification is always the goal and many neurology departments are equipped with clinical electrooculography set-ups, simple inspection easily reveals most eye movement disorders at the bedside.
Quantitative assessment of ataxia of stance and gait, as well as limb ataxia and dysarthria, is rarely done in a clinical setting. Special equipment is needed such as motion sensors, kinetographs, and high-resolution microphones for acoustic analysis of speech. In addition, in the differential diagnosis of ataxias, the gain of quantitative assessment is often limited compared to the clinical evaluation, and, as yet, most neurology departments do not provide the necessary equipment except clinical electrooculography set-ups. This is different in the situation where treatment effects, e.g., in a drug trial need to be quantified. Treatment effects in a short time interval are likely small and will not be picked up by clinical examination.
We will start with reviews of known findings in the literature about electrophysiological studies in ataxias (see Tables 1 and 2). Regarding the core symptoms, speech, stance, gait, and eye movement assessment, we will begin with categorizing common chief complaints, then their examination correlates, and ultimately their anatomic and functional localization (see Tables 3, 4, 5, and 6). We will incorporate discussion of quantitative methodology within each section to emphasize the complementary roles of clinical and neurophysiological assessment. The role of neurophysiological assessments in the differential diagnosis of ataxias and increasingly difficult classification of its different types will be discussed. Furthermore, we aimed to evaluate the prospects as potential biomarkers for some of the cerebellar ataxias.
Nerve Conduction Studies and Electromyography
L. Schöls, Tübingen, Germany
Involvement of peripheral nerves is frequent in hereditary ataxias. Some genotypes present with predominant sensory neuropathy, whereas others develop a sensory-motor type but not pure motor neuropathies (Table 1) [9,10,11,12,13,14]. Some subtypes of ataxia like ataxia with coenzyme Q10 deficiency and ataxia with SYNE1 mutations typically do not develop peripheral neuropathy, and respective phenotyping may help in the clinical differentiation of the genetic subtypes. In Friedreich’s ataxia (FRDA), nerve conduction studies reveal severe sensory neuropathy of axonal type in almost all patients with genetically proven disease while motor nerve conduction studies are usually normal [15]. Similar findings as in FRDA are obtained in nerve conduction studies of patients with mutations in the POLG gene causing sensory ataxic neuropathy with dysarthria and ophthalmoplegia (SANDO) [16]. Also ataxia with primary vitamin E deficiency (AVED) presents with pure sensory axonal neuropathy but the reduction in sensory nerve action potentials (SNAP) tends to be less severe than in FRDA [17].
In contrast to this group of ataxias with pure sensory neuropathies that result from primarily mitochondrial defects, there is a group that is characterized by the combined affection of sensory and motor fibres and is caused by impaired DNA repair. This group includes ataxia telangiectasia (AT), ataxia with oculomotor apraxia type 1 (AOA1), and ataxia with oculomotor apraxia type 2 (AOA2) each of them going along with distally pronounced sensory-motor neuropathy [14, 18, 19]. Autosomal recessive spastic ataxia of Charlevoix Saguenay (ARSACS) also presents with sensory-motor neuropathy but in contrast to the DNA repair disorders mentioned before, it shows more dysmyelinating features [20].
In the dominantly inherited spinocerebellar ataxias (SCA), nerve conduction studies reveal peripheral nerve affection in most patients with SCA1, SCA2, and SCA7 and less frequently also SCA6 [11, 13, 21, 22]. Peripheral neuropathy presents in genotype-specific patterns. In SCA3, peripheral neuropathy affects sensory and motor nerves. SCA3 neuropathy occurs in some patients with subclinical dysfunction that is only detected by nerve conduction studies but may in other patients constitute the major manifestation of disease. In a multifactorial regression analysis, age but not CAG repeat length nor disease duration was identified as the major factor that correlates with both compound muscle action potentials in motor nerves as well as SNAP in sensory nerves [23]. Accordingly, peripheral neuropathy is the major manifestation in patients with relatively short expansions and late onset of disease [24]. In SCA2, neuropathy predominantly affects sensory nerves with a decrease in sural SNAP with longer disease duration and more severe disease [25]. In SCA1, sensory and motor nerves are affected but differ from the other genotypes by a significant slowing of nerve conduction velocities as well as F-wave latencies [11, 22, 26].
Peripheral nerve affection has been proven even in presymptomatic stages of the disease in SCA2. In SCA2, reduction of sural SNAP is evident about 5 years prior to onset of symptoms and decreases further during the prodromal state and well into the disease [25, 27]. These studies suggest nerve conduction parameters as a potential biomarker for future interventional trials in presymptomatic states of SCAs.
Electromyography (EMG) depicts neuronopathy in patients with SCA1, SCA2, SCA3, and SCA7 [13]. Motor neuron affection is confirmed clinically by the presence of fasciculations. Neuropathological examination reveals loss of motoneurons in the anterior horns in SCA1, SCA2, and SCA3 [28].
In summary, nerve conduction studies can help in the differentiation of ataxia genotypes by characterizing peripheral nerve involvement. Furthermore, electrophysiological parameters like compound muscle action potential (CMAP) and SNAP may serve as biomarkers indicating disease progression. However, before its use as outcome parameters in interventional studies, longitudinal data is required to estimate its sensitivity to change and reproducibility in a multicentric setting.
Evoked Potentials to Sensory Stimuli
L. Schöls, Tübingen, Germany
Evoked potentials frequently prove affection of the visual (VEP), auditory (BAEP), and somatosensory (SEP) system in many subtypes of hereditary ataxia and reflect the wide spread of pathology in many of these disorders. This is especially true in the polyglutamine disorders SCA1, SCA2, SCA3, and SCA7 [10,11,12]. As for many of the rare genotypes, no representative data is available, and this overview is confined to SCA1, 2, 3, 6, and 7.
Sensory evoked potentials (SEP) are challenging to assess in SCA as peripheral damage overlaps with disturbance of the central sensory tracts. Furthermore, it is technically difficult to reach relaxation of the patient due to frequent pyramidal involvement that triggers muscle responses that hinder proper recordings especially of peripheral components in fractionated SEP. This may well be the reason for the limited number of SEP studies in hereditary ataxias, although they frequently reveal abnormal findings in SCA1 as well as in SCA2 and SCA3 [11, 21, 25].
Abnormal visual evoked potentials (VEP) are a hallmark of SCA7 and reflect the retinal degeneration that goes along with ataxia in this subtype of SCA [29]. In other SCA genotypes, VEP are more variably affected [10, 12, 25].
Brainstem auditory evoked potentials (BAEP) are abnormal in the majority of patients with SCA2 and even in many presymptomatic mutation carriers [21, 25]. This finding matches well with the early and severe pontine atrophy seen on MRI in SCA2. In accordance with the widespread and severe neurodegeneration found in neuropathological studies also in SCA1 and SCA3, BAEP reveal brainstem affection also in many SCA1 and SCA3 patients [11, 21]. Whereas in SCA1, 2, and 3 frequently affect central parts of the auditory tract, in SCA6 peripheral affection of the auditory system is more frequent [11, 21].
Studies of evoked potentials in genetically confirmed cohorts of autosomal recessive ataxias are exceptionally rare. Even in the most frequent subtype, Friedreich’s ataxia (FRDA), there are only few studies in genetically proven cases. Characteristic finding in FRDA is a loss of SEPs in combination with severe axonal sensory neuropathy [15, 30]. SEP findings are similar in ataxia with primary vitamin E deficiency (AVED) which is a phenocopy of FRDA [31]. In Ataxia telangiectasia (AT), SEP revealed common and severe affection of the sensory system, progressive over the course of disease and affecting both, the peripheral and the central sensory pathways. BAEP revealed only minor affection of the brainstem in some AT patients [32]. ARSACS is characterized by slowing of conduction in almost all fiber tracts resulting in prolonged latencies in VEP as well as BAEP and also SEP [20, 33].
In summary, although sensory systems are affected in many ataxia subtypes, systematic analyses are missing in most genotypes. Comprehensive studies in representative genetically confirmed cohorts with a longitudinal assessment of evoked potentials are worthwhile to explore EP parameters as potential biomarkers to monitor disease progression in natural history studies as well as interventional trials.
Transcranial Magnetic Stimulation
M. Branscheidt, P. Celnik, Baltimore, USA
Transcranial magnetic stimulation (TMS) is a noninvasive technique that has been successfully used to investigate brain physiology in healthy individuals as well as in a wide range of pathological conditions. TMS can be used to determine different functional aspects of the motor system: integrity of the pyramidal tracts, balance of inhibition and excitation, and the connectivity between different brain regions, including the connection between motor cortex (M1) and the cerebellum. Dysfunction of the pyramidal tracts is typically characterized as reduction in amplitude size or absence of motor evoked potentials (MEPs), and/or in increases in the central motor conduction time (CMCT). Imbalances in inhibitory and excitatory circuits can be probed by double-pulse paradigms, where a conditioning TMS stimulus precedes the test TMS stimulus. Of interest to this consensus paper, cerebellar-motor connectivity can be evaluated by applying a conditioning stimulus over the cerebellum prior to a test stimulus delivered to the contralateral motor cortex. In healthy controls, this leads to a decrease of the MEP amplitude elicited from M1, a phenomenon termed cerebellar brain inhibition (CBI) and thought to be mediated by activation of the cerebellothalamocortical pathway. In this manner, several recent studies have used this measurement to read out the level of cerebellar activation in the context of different behavioral and/or cerebellar stimulation experiments [34, 35]. Because of its relative simplicity, the CBI paradigm seems ideal to understand the pathophysiology of different neurological conditions that affect the cerebellum. For instance, it has been shown that in Parkinson’s disease or dystonia, CBI is reduced [36, 37]. However, these TMS measures have not yet found a clear clinical role in the pathophysiological understanding or diagnosing of ataxias.
Motor evoked potentials, on the other hand, frequently prove affection of the corticospinal tracts in many subtypes of hereditary ataxias. MEPs might help dissociate different types of ataxia, and can detect pyramidal tract dysfunction even in the absence of clinical symptoms in some SCA subtypes [12, 38, 39].
Motor evoked potentials have been studied foremost in the most common dominant ataxias. MEPs show that the corticospinal tract is frequently affected in SCA1, SCA2, SCA3, and SCA7 [21, 30, 40]. Central as well as peripheral motor conduction time is prolonged especially in SCA1 and constitutes a distinct pattern separating SCA1 from SCA2, SCA3, and SCA6 [11, 21, 41, 42]. Prolonged central motor conduction times have also been reported in SCA6 patients from Taiwan [43]. Furthermore, motor cortex activation is altered with an elevated motor threshold in SCA1 and SCA2 and reduced intracortical facilitation in SCA2 and SCA3 [30, 44]. MEPs are abnormal even in the prodromal stage of the disease in presymptomatic carriers of SCA1, SCA2, and SCA3 mutations [38, 39, 45]. In prodromal stages of SCA1, MEP was shown to be affected before disease onset, whereas SEP abnormalities developed with the onset of first symptoms and peripheral nerve involvement occurred only in early symptomatic stages of the disease [38].
MEP data in recessive ataxias is limited. Characteristic findings in FRDA are prolonged CMCT or absent MEP [15, 30]. MEP data are not available in AVED [31]. SANDO with POLG mutations also shows severe sensory deficits and afferent ataxia but differs from FRDA electrophysiologically in that MEPs are generally normal [16]. In ataxia telangiectasia (AT), MEPs were altered in 4/5 patients, although clinical signs of cortico-spinal tract affection were missing [32]. ARSACS is characterized by prolonged latencies in MEP [20, 33].
TMS findings in ataxia, however, have not been consistent across studies. Restivio et al. [40], for example, found more frequent abnormal pyramidal tracts signs in SCA2 than previously reported. Similarly, Farrar et al. [39] observed reduced intracortical inhibition and prolonged conduction times in patients with SCA3, while Schwenkreis et al. [30] showed significant reduction of intracortical facilitation and normal CMCT. The inconsistencies across studies might be due to the relatively small sample size, differences in disease stage, and accompanying extracerebellar pathologies (e.g., Parkinsonism in SCA3). Changes in short-interval cortical inhibition are altered in different pathologies to a similar extent, indicating low specificity of the method [46]. Thus, using TMS as a tool to elucidate differential diagnosis has been difficult [46].
Albeit the above-listed limitations, TMS might have a role as a complementary rather than a primary technique when it comes to differential diagnosis. For example, Schelhaas et al. [47] identified early-onset cerebellar ataxias clinically similar to Friedreich’s ataxia but without a frataxin gene mutation. In this subgroup, neurophysiological testing using TMS revealed three distinct phenotypes which might inform future genetic testing.
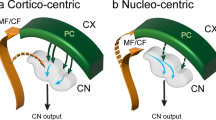
Assessing CBI introduces the possibility of differentiating conditions that cause ataxia due to involvement of afferent vs. efferent cerebellar pathways [48]. Patients with ataxia due to pathology of peripheral nerves or the posterior column or lesions of the middle cerebellar peduncle (afferent pathway) are more likely to show no changes in CBI. In contrast, patients with lesions of the cerebellum or the superior cerebellar peduncle, as well as patients with a degenerative cerebellar disease (SCA, MSA, paraneoplastic cerebellar atrophy, Wilson’s disease, efferent pathway), show decreased CBI (for an overview see [48]). Moreover, these changes seem to follow the trajectory of disease progression, with pronounced decrease of CBI over time in degenerative ataxias versus normalization of CBI with recovery from acute cerebellar ataxia [49, 50].
While these results are very promising, it has to be noted that the number of tested subjects remains very small and future research is needed to investigate factors that influence CBI in ataxia. For example, two out of ten patients with ataxia due to MSA had normal CBI measures. These two patients presented with predominant trunk and lower limb ataxia, while having only mild to absent upper limb involvement [51]. While the finding might explain that CBI follows somatotopic specificity rules [52], further characterization of this measurement in the context of patient populations is required to become useful in the clinical setting.
In sum, to date, TMS has not been established as a diagnostic tool in ataxia and remains largely in the research phase. Data regarding the reliability, sensitivity, and specificity of TMS measures comparing healthy controls and the different forms of ataxia are scarce. However, TMS can be used to probe pyramidal tract involvement even before clinical symptoms become apparent, and therefore might help predict time to ataxia onset. Of note, it might provide diagnostic evidence when imaging findings are still unremarkable.
CBI could also be useful to explore some of the pathophysiological mechanisms underlying different cerebellar diseases, to localize the anatomical origin of ataxias (efferent versus afferent pathways) and perhaps in the early differential diagnosis of Parkinson Plus Syndromes (especially MSA-C). Finally, theoretically, TMS could also be useful to monitor response to specific ataxia treatment interventions. Thus, TMS can potentially be developed into a promising screening and/or monitoring tool in ataxia; however, further studies are needed to assess its sensitivity, specificity, and predictive power in this patient population. Its application to investigate cerebellar connectivity and subclinical pyramidal tract involvement are especially intriguing in this context.
Electroencephalography
H. A. G. Teive, L. de Paola, Curitiba, Brazil
Autosomal Recessive Cerebellar Ataxias
Autosomal recessive cerebellar ataxias (ARCAs) encompass a heterogeneous group of usually early onset inherited ataxias, led by Friedreich’s ataxia (FRDA) and followed by ataxia telangiectasia (AT) [1]. Remillard et al. [53] evaluated electroencephalography (EEG) tracings of 50 patients with FRDA. They reported only mild nonspecific abnormalities in 33% of patients, with abnormal slow or irregular background rhythms (30%), intermittent paroxysmal rhythms (8%), and unilaterally absent driving responses (4%). There was no response to intermittent photic stimulation in 60% of the patients. Only 8% of the patients reported epileptic seizures [53]. Autosomal recessive spastic ataxia of Charlevoix-Saguenay (ARSACS) is rarely associated with epileptic seizures [54]. Anheim et al. [54] studied two patients from a French family with genetically proved ARSACS who, in addition to the classical phenotype, displayed asymptomatic generalized spikes and waves. Ramsay-Hunt syndrome (RHS) or progressive myoclonus ataxia (PMA) is a controversial group of diseases, characterized by the presence of progressive cerebellar ataxia, associated with myoclonus, mild epilepsy, and cognitive dysfunction. In 2014, van Egmond et al. [55] described five RHS patients from the Netherlands (due to a homozygous mutation in GOSR2 gene—Golgi Qb-SNARE gene), presenting with progressive cortical reflex myoclonus, cerebellar ataxia, generalized epileptic seizures, and areflexia. EEG and EMG recordings demonstrated the presence of cortical spikes or spike-waves forms preceding myoclonic jerks.
Autosomal Recessive Cerebellar Ataxias—Other Diseases
The progressive myoclonus epilepsy (PME) group defines a syndrome with myoclonus, severe epilepsy, progressive dementia, and also cerebellar ataxia [56]. This group of diseases includes neuronal ceroid lipofuscinoses (NCLs), Lafora disease, Unverricht-Lundborg disease (ULD), myoclonic epilepsy with ragged red fibers (MERRF), among others. NCLs represent a group of hereditary diseases causing progressive neuronal degeneration, with dementia, refractory epilepsy, movement disorders, including cerebellar ataxia, and progressive visual impairment due to retinal dystrophy. In 2015, Canafoglia et al. [57] evaluated the electroclinical spectrum of the NCLs associated with CLN6 mutations. The authors describe an EEG pattern with slow and poorly organized EEG background, slow spike and waves, and photoparoxysmal responses at low frequencies during photic stimulation. In the follow-up, the EEG became extremely slow and spike-wave discharges proved rare, replaced by individual spikes with multifocal distribution. Lafora disease (LD) is an autosomal recessive inherited disease, characterized by the presence of myoclonus, epileptic seizures, visual hallucinations (occipital seizures), with progressive dementia, and cerebellar ataxia [58]. Diagnosis is based on clinical and EEG findings and detection of two pathogenic mutations of two genes, EPM2A or EPM2B. The EEG typically shows slowing of background activity, paroxysms of generalized irregular spike-wave discharges with occipital predominance, and focal (occipital) abnormalities. ULD, a progressive myoclonic epilepsy type 1, is an autosomal recessive inherited disease characterized by the presence of stimulus-sensitive myoclonus, tonic-clonic epileptic seizures, and cerebellar ataxia [59]. Recently, Gargouri-Berrechid et al. [59] analyzed the long-term evolution of EEG in 17 patients with ULD. The most common EEG abnormalities were slow and disorganized background rhythms, with epileptic abnormalities in 47% of patients, including myoclonic jerks in 28%. Follow up EEGs, performed after regular treatment, showed improvement of background activity, with no epileptic abnormalities. The classic phenotype of glucose transporter type 1 (GLUT1) deficiency syndrome (De Vivo disease) is characterized by infantile-onset epileptic seizures, delayed neurologic development, microcephaly, and movement disorders, including dystonia and cerebellar ataxia [60]. The patients commonly have a low CSF glucose concentration. In 2005, Ito et al. [60] published an interesting case report of GLUT1 deficiency syndrome from Japan, in which pre-/postprandial EEG changes were demonstrated (with postprandial improvement compared to the EEG following an overnight fasting). They suggested that in children with epileptic seizures and unexplainable neurological deterioration, the CSF analysis and pre-postprandial EEG changes may be useful in diagnosing this potentially treatable disorder. More recently, there is increasing recognition that GLUT1 may have a much more varied phenotype [61].
Spinocerebellar Ataxias
In 2005, Rakowicz et al. [62] evaluated 44 patients with spinocerebellar ataxias (SCAs) type 1 and 2, providing data on clinical, electrophysiological, and magnetic resonance imaging. EEG was performed but no significantly abnormalities were noted. In 2012, Beluzzo et al. [63] published a case report of nocturnal frontal lobe epilepsy in a patient with SCA type 17. The awake scalp EEG was unremarkable, whereas the nocturnal video-electroencephalogram recording, demonstrated the epileptic seizure and EEG nonspecific abnormalities. SCA type 10, originally found in Mexico, has been described as a pure cerebellar ataxia associated with epileptic seizures (partial complex and generalized tonic-clonic) [64]. Rasmussen et al. [64] studied four Mexican families with SCA10, and epilepsy was found in 72.2% of patients. Grewal et al. in [65] evaluated clinical features and ATTCT repeat expansion in SCA10. The authors studied two large families with SCA10 and epileptic seizures were frequent with complex partial seizures, or complex partial seizures with secondary generalization, or generalized motor seizures (tonic-clonic), and in one patient status epilepticus was diagnosed. The EEG varied from normal to positive for focal or bilateral epileptiform discharges. Conversely, Teive et al. [66] described the clinical phenotype of five Brazilian families with SCA10 presenting with pure cerebellar ataxia but no associated epilepsy. In 2010, Teive et al. [67] studied the frequency of epilepsy in a large sample of 80 Brazilian patients from 10 Brazilian families. Overall, the frequency of epilepsy was considered rare (3.75%). Two patients had generalized tonic-clonic seizures, and one patient had a combination of myoclonic, complex partial, generalized tonic-clonic seizures, with occasional status epilepticus. Interictal EEG of these three patients was abnormal in only one patient, showing diffuse disorganization but no clear cut epileptiform activity.
Dentatorubral-pallidoluysian atrophy (DRPLA) is a rare autosomal dominant neurodegenerative disease caused by an expansion of a CAG repeat in the atrophin-1 gene on chromosome 12 [68]. DRPLA is characterized by several combinations of cerebellar ataxia, myoclonus, epilepsy, dementia, movement disorders, and psychiatric symptoms. The phenotype may be similar to PME, PMA, Huntington’s disease (HD), and SCAs. The EEG abnormalities include burst of frontal and central slowing, with diffuse spike-wave complexes. Epileptic discharges may be induced by photic stimulation [68].
Episodic Ataxias
EA-2 (CACNA1A gene), the most common syndrome, is characterized by episodes of cerebellar ataxia (with duration of hours to days) associated with interictal nystagmus and sometimes progressive ataxia. Associated symptoms are vertigo, nausea, and vomiting, and migraine is found in 50% of patients. Some patients can also have progressive cerebellar ataxia and epileptic seizures. EA-3, EA-4, EA-7, and EA-8 (UBR4 gene) represent very rare forms of episodic ataxias (EA), and EA-5 (CACNB4 gene) can be associated with generalized epilepsy. EA-6 (SLC1A3 gene) is associated with episodes of hemiplegia and seizures [69, 70]. Other genes associated with EA include ATP1A3, SLC2A1, FGF14, and proline-rich transmembrane protein 2 (PRRT2). PRRT2 gene mutations can cause paroxysmal kinesigenic dyskinesia (PKD), infantile convulsions, epilepsy, migraine, and hemiplegic migraine [71]. In 1996, van Bogaert and Szliwowski [72] presented EEG findings in acetazolamide-responsive hereditary paroxysmal ataxia. The authors studied six family members, and intermittent rhythmic delta activity was found at rest in most patients, associated with less frequent low amplitude spikes. EEG abnormalities were activated by hyperventilation.
Mitochondrial Ataxias
Mitochondrial ataxias represent a rare group of cerebellar and afferent ataxias due to mitochondrial DNA POLG gene mutations [1]. In general, mixed ataxia is associated with peripheral neuropathy, external ophthalmoplegia, ptosis, movement disorder, and epilepsy. Ekbom’s syndrome is a mitochondrial encephalopathy associated with mutation in the mitochondrial DNA, with cerebellar ataxia, cervical lipoma, and photomyoclonus. The EEG may represent a contributory test in the evaluation of this disease [73].
Conclusions
For the most part, EEG findings are nonspecific. EEG, however, may play a potential role in the differential diagnosis of ARCA, PMA, PME (with cerebellar ataxia), SCAs, particularly SCA type 10, and mitochondrial and episodic ataxias.
Speech Assessments in Ataxia
A. P. Vogel, Melbourne, Australia
Profound difficulties communicating affect the majority of people with a degenerative ataxia. Speech severity also correlates with clinical characteristics such as disease duration and severity [74, 75] making it a viable proxy of degeneration [76, 77] and treatment response [78].
Speech in Friedreich’s ataxia (FRDA) and spinocerebellar ataxias (SCA) is characterized by reduced or uncontrolled variation in pitch and loudness, a slower rate of speech and articulatory timing [79], imprecise production of consonants and vowels, dysphonia [80], impaired nasality [81], abnormal resonance [81], and reduced intelligibility [74, 75]. These deficits worsen over time [76]; however, no natural history studies have looked at devolution of speech beyond 4 years. The exact prevalence of dysarthria in these populations is unknown; however, evidence from FRDA suggests that all individuals with a disease duration longer than 4 years present with dysarthria [74]. Efforts to use speech as a differential diagnostic tool have proven difficult with a relative absence of adequately powered data on neurodegenerative ataxias [82, 83]. Nevertheless, current evidence suggests that regularity of alternating and repeating syllables (diadochokinesis; DDK) is markedly impaired in SCA3, whereas individuals with SCA6 can present with more pronounced deficits in speech rate and pitch and loudness variation [82]. With this information in mind, these deficits are also observed in other hereditary ataxias including FRDA and POLG associated ataxia [84] with some studies proposing that specific speech subsystems devolve at different rates across the disease spectrum [74].
Assessment Battery
The tasks used to assess speech in ataxia in daily practice are ideally objective, need to be stable in the absence of change, and sensitive to disease progression or treatment response [85, 86]. Protocols can include examination of the underlying oral musculature structure and function, listener-based ratings of impaired speech features, patient self-report, and objective acoustic analysis to quantify change over time (see Table 3). Aspects of this protocol were chosen for their utility (e.g., ease of use, administration time, clinical information provided, etc.) and psychometric properties (e.g., reliability, validity). Acoustic analysis of speech provides an objective adjunct to listener-based judgments of speech precision and clarity. Acoustic analysis uses a combination of spectrographic and waveform (among other modalities) analysis of the physical properties of sound production to provide information on vocal output. Analysis of fundamental frequency (acoustic correlate of pitch), for example, is estimated from the number of vocal fold pulses the larynx produces within a second and validated against ground truth data derived from electroglottography (EGG) [87]. Other acoustic analysis metrics tap into different neurophysiological responses of disease such as speech-related timing deficits [88].
There is not an established ataxia-specific speech protocol, however. One that considers tasks with varying levels of complexity (cognitive load) can assist in determining the basis of changes to speech (i.e., cognition or motor decline) [89, 90]. Example tasks increasing in complexity include (i) a sustained vowel /a/, (ii) diadochokinesis (DDK) tasks (e.g., pata within SCAFI), (iii) reading, and (iv) unprepared monologue or conversation. Variations of this protocol have been applied in ataxia [74] and other neurodegenerative diseases [91] with demonstrated stability and sensitivity [86, 92]. It is recommended that speech recorded for perceptual and acoustic analysis is acquired using a high-quality equipment (see [93] for tutorial on hardware options). This approach reduces noise in the recorded signal allowing accurate mapping of the acoustic signal designed to pick up perturbations in the voice. Acoustic data can be derived using automated scripts or by hand via free (e.g., Praat) or commercially available software (e.g., KayPentax). Basic acoustic outcomes for ataxia can include measures of timing (e.g., speaking rate (syllables/total signal time), mean pause length [88]), vocal control (e.g., variation of fundamental frequency or intensity), and quality (e.g., harmonics to noise ratio).
Current State of Play
Speech assessment protocols currently used in clinical practice rely heavily on the expertise and experience of the clinician to make judgments about the speaker. They are limited by their subjectivity and poor inter-rater reliability. Listener-derived examinations are well suited for describing the characteristics of a speech disorder but are limited in their capacity to objectively describe changes resulting from neurodegeneration or treatment response. Further, few clinical exams include formalized assessments of the impact of dysarthria on the patient. We suggest clinical researchers employ brief but repeatable tests of speech that utilize acoustic analysis to objectively measure change in production combined with standardized self-report measures on speech-related quality of life and listener-based judgments on set tasks of varying complexity. The future with speech acquisition and analysis lies with remote capture and monitoring of speech in natural settings (i.e., the home) outside of traditional clinic-based approaches.
Gait Assessments in Cerebellar Ataxia
W. Ilg, Tübingen, Germany
Ataxic gait is typically characterized by an increased step width, variable foot placement, irregular foot trajectories, and a resulting unstable, veering navigation with high movement variability [97,98,99] and a high risk of falling [100]. Causes for ataxic gait can be varied, including focal cerebellar disease such as stroke, cerebellar tumors, multiple sclerosis, and degenerative diseases affecting the cerebellum or its afferent pathways (see [99] for a more detailed description). For the most common autosomal dominant spinocerebellar ataxias (SCAs), gait is the initial ataxic symptom in approximately two-thirds of all patients [101, 102].
In the clinical setting, ataxia symptoms are rated commonly using clinical ataxia rating scales like ICARS [103] and more recently SARA [104]. Both scores include, in a semi-quantitative way, stance, the assessment of a 10-m gait test including a half-turn, and execution of tandem gait. Ratings are based on the ability of free walking, the judging of the amount of staggering, and the counting of missteps for the tandem walk. Both scores, ICARS and SARA, include subcategories for gait and posture (e.g., SARAposture&gait ≡ sum of the three SARA items: gait, stance, and sitting) [104, 105], which have been examined as progression marker of gait impairments [106] or as outcome marker for gait rehabilitation studies [107, 108]. In addition to the clinical ataxia scores, additional scores are used to describe the ability of balance and gait control in scenarios relevant to everyday life. Common examples are the self-report of balance confidence in everyday life activities using the Activity-specific Balance Confidence Scale (ABC) [109], the dynamic gait index [110], and BESTest [111], testing more complex gait behavior including walking over obstacles and walking up stairs.
Quantitative Assessments
Quantitative gait assessments and the analyses of spatio-temporal characteristics of ataxic gait patterns have been conducted in order to examine the underlying pathological control mechanisms and to perform a more fine-grained and objective characterization of ataxic gait. Several studies of ataxic gait reveal that gait features like decreased velocity and step length as well as increased step width and step cycle time might reflect predominantly cerebellar-nonspecific safety strategies rather than discrete deficits in control [112,113,114,115,116]. In contrast, the most striking and distinctive features of ataxic gait on the kinemetic level seem to be the high variability in several spatial and temporal gait features (e.g., variability in step length, step width, and gait cycle time) [112,113,114, 117, 118].
The spatiotemporal structure of ataxic gait has also been characterized on the level of leg muscle activity. A considerable widening of EMG bursts and significant temporal shifts in the center of activity has been found due to overall enhanced muscle activation between late swing and mid-stance [119]. Abnormalities in intersegmental coordination have been identified associated with these changes in the leg muscle activity pattern. In addition, an abnormal transient has been found in the vertical ground reaction force and instability of limb loading at heel strike.
In Friedreich’s ataxia, lower limb spasticity has been identified in gastrocnemius and soleus muscles as a sensitive measure which is evident early in the disease and correlated to gait impairments measured by functional gait scores [120].
In summary, the observed characteristic high variability of walking patterns is most likely due to the complex interaction between cerebellar-induced deficits in balance control [115, 121] and multi-joint coordination [112], used safety strategies and inaccurate adjustments to appearing losses of balance. Consequently, this results in a continuous step-by-step adjustment of the gait strategy, making it demanding to quantitatively describe the actual walking behavior of ataxia patients [114].
As gait features describing disease progression, velocity and mean step length as well as step length variability have been identified [106, 122]. Most of these progression markers show correlations with the changes in SARA or ICARS scores for patient populations from moderate to more severe ataxia.
In addition to these patient populations, an emerging research topic including the assessment of ataxia-related movement changes presents the pre-clinical stage of degenerative cerebellar ataxia, the phase before clinical manifestation of the disease [123]. As this stage provides a promising window for future early therapeutic interventions [124], there is a need for measures which can sensitively identify and quantify progression and intervention benefits in the preclinical stage. By their nature, clinical scores lack the sensitivity to quantify subtle movement changes [125]. A recent study on mutation carriers of autosomal dominant spinocerebellar ataxias has delivered evidence, that spatio-temporal gait features in complex gait conditions like tandem walking enable the identification of pre-clinical movement changes in mutation carriers without any clinical gait sign, several years before clinical manifestation [126]. Thereby, features like the temporal variability of gait cycles have shown to be distinctively more sensitive in identifying early behavior changes in tandem walking in comparison to counting missteps, like used in clinical rating [27, 104]. An overview of studies using quantitative gait assessment in cerebellar ataxia can be found in Table 4.
Motivated by emerging research questions like finding objective evaluations of intervention outcome, there is an increasing demand for quantitative movement assessments also in clinical centers which do not have an advanced motion lab with an elaborated whole-body motion capture system. Alternative systems are pressure-sensitive mats to analyse spatio-temporal step parameters (e.g., step length and time) [127,128,129], affordable camera-based systems [130, 131], or portable inertial sensors which are used for instance for instrumented Timed Up and Go tests [132]. Future studies have to validate the application of such quantitative assessments in multi-center environments.
Gait Rehabilitation
Although benefits of motor rehabilitation in degenerative cerebellar disease have been discussed controversially for a long period [133, 134], recent studies reach more and more common acceptance that continuous motor training can improve gait function in degenerative patients, for instance by increasing gait velocity and decreasing step variability and body sway [107, 135,136,137,138,139].
Analyzing Gait and Falls in Everyday Life
The analysis of patients’ behavior in everyday life attracts more and more attention. First studies documented falls and identified measures in quantitative gait assessments like increased step length variability, which are associated with increased fall risk [128, 140]. Other approaches documented the ambulatory activity with portable inertial sensors as an progression or outcome marker [141]. In the future, portable inertial sensors will allow a more detailed characterization of ataxia-related spatio-temporal gait features in more unconstraint assessments and ultimately in everyday life.
Conclusions
The quantitative assessment of gait is less important for differential diagnosis but serves as a very relevant progression marker as well as an important measure for the rating of intervention benefits relevant for everyday life.
Measuring Postural Control
FB Horak, Portland, OR, USA
Balance disorders due to impaired postural control are inevitable in patients with ataxia and have severe consequences. Falls and fall-related injuries are common with 84% of cerebellar ataxic patients reporting at least one fall per year and 74% reporting fall-related injuries [100, 154]. Although nonataxia symptoms in patients with cerebellar involvement, such as pyramidal weakness or spasticity, also contribute to falls, ataxia is associated with hypermetria as well as sensory integration and multisegmental coordination deficits that directly contribute to falls by impairing control of postural equilibrium and orientation.
Ataxia impairs several independent domains of postural control, including (1) postural sway in stance, (2) anticipatory postural adjustments (APAs), and (3) postural responses to external perturbations (APRs). Evidence for impairments in each of these domains of postural control come from laboratory studies using force plates to quantify hypermetric center of foot pressure, surface electromyography to measure intramuscle temporal coordination, and motion capture to characterize control of body center of mass by whole body kinematics. Control of postural sway in stance involves the integration of sensory information from proprioception, vision and vestibular systems, and reweighting dependence upon these sensory systems when sensory conditions change [155]. APAs are preprogrammed postural strategies that precede fast, voluntary movements to prevent postural imbalance [156]. APRs involve activation of multisegmental postural muscle synergies at 100 ms to recover from accidental slips and trips and pushes [157]. Ataxia-related hypermetria, impaired sensory integration, and multisegmental coordination affect all of these domains of postural control.
Postural sway in stance is significantly larger in the majority of people with cerebellar ataxia than in age-matched control subjects [158]. The first quantitative study of the effects of cerebellar ataxia on postural sway using force plates found that 86% of subjects showed larger than normal sway path and/or sway area [159]. However, the particular abnormal frequencies of sway depended on what parts of the cerebellum were involved. For example, spinocerebellar ataxia from Friedreich’s ataxia results in excessive sway at low frequencies (0.1–1 Hz), whereas anterior lobe deficits result in excessive sway at higher frequencies (2–4 Hz) that has been called “postural tremor.” The increase in lower sway frequency may be due to slowed proprioceptive conduction resulting in delayed closed loop feedback control of postural sway. In contrast, the increase in higher sway frequency may be due to excessive use of the hip strategy, rather than ankle strategy, for control of posture [160].
The increase in postural sway in cerebellar, compared to control, subjects is enhanced by eye closure, in all but subjects with vestibulocerebellum involvement [159]. Vestibulocerebellar involvement apparently prevents use of vision for postural stability and perception of verticality as these patients not only sway more, but may also tilt their trunk to one side, even with eyes open. The exaggerated dependence upon vision for postural control in the majority of ataxic patients is likely a compensation for impaired use of proprioception due to spinocerebellar proprioceptive involvement. When the vestibulocerebellum is involved, ataxic patients also show even larger differences in sway from controls when they need to use vestibular information for postural control, e.g., when standing on a compliant surface or with a narrow base of support with eyes closed [161,162,163]. These difficulties suggest that the vestibulocerebellum is important for using vestibular information to control postural orientation and stability.
Postural instability in ataxic patients is characterized by large trunk displacements, velocities, and accelerations and exaggerated ankle roll instability, quantified with motion capture. This instability is likely due to both hypermetric postural responses, as well as delays in the closed-loop feedback control of sway. Despite their larger sway, cerebellar ataxics reduced that sway more than control subjects when diverting their attention to a cognitive task under dual task conditions [164]. This exaggerated reduction in sway during a dual task is thought to be due to a maladaptive increase in muscle co-contraction because it was also associated with more falls under challenging stance conditions [164].
Anticipatory postural adjustments are present, though impaired, in people with cerebellar ataxia, suggesting that the cerebellum is not critical for their development or storage. However, later onsets and disrupted intra-limb and multisegmental timing of muscle activity suggest the cerebellum is involved in muscle activation timing for refined movement metria. For example, activation of tibialis anterior as an APA prior to rising onto toes has a longer latency, is more variable and tonic, rather than phasic burst, in subjects with ataxia [165]. APAs that shifted the center of pressure laterally and forward prior to a voluntary step were also present in subjects with ataxia and could be modified by external feedback, but did not scale with anticipation of external feedback [166]. The first step size and speed was slower than controls, however, and may be compensatory for impaired APAs. Similarly, APAs in the legs associated with sudden release of a load to the arms showed intact muscle activation patterns but with more cocontraction and background muscle activation [167]. However, a recent study showed impaired temporal coordination and long latencies of proximal arm muscles associated with fast finger flexion in supported sitting, suggesting that intralimb coordination is affected [168].
Automatic postural responses to external perturbations in people with cerebellar ataxia have normal latencies with hypermetric response size, abnormal multisegmental coordination, and impaired adaptation to anticipated changes in perturbation characteristics. The short and medium latency postural muscle responses at 50 and 100 ms are normal in cerebellar ataxia, regardless of whether the direction of surface displacement is a translation or rotation, predictable or randomly presented [169,170,171]. Normal latencies of postural muscle responses to proprioceptive stimuli suggest that the cerebellar feedback loop is not critical for triggering or creating the synergy patterns of these rapid postural responses. However, postural response size is hypermetric in ataxia, resulting in postural instability, sometimes resulting in falls in the opposite direction of the perturbation. Postural responses to both slow and fast surface translations or rotations often result in falls, with large trunk displacements. The longest latency responses to perturbations are especially exaggerated in size and duration, perhaps to compensate as antagonists to the hypermetric agonist responses [159, 170, 172]. Abnormal multisegmental coordination is apparent in postural responses also, characterized in excessive locking of the knees, resulting in trunk instability.
In addition to hypermetric postural responses, the size of the postural response, both center of pressure displacement and muscle activation, does not adapt to predicted, upcoming postural perturbation size [170]. A follow-up study showed that although cerebellar ataxics could predict the amplitude of postural perturbations based on prior experience, they could not scale up or down the size of postural responses based on this prediction [173]. Surprisingly, postural response size could be reduced with repetition (habituation), despite the difficulty increasing and decreasing postural response magnitude based on predicted perturbation size. These results suggest that the cerebellum plays a critical role in adapting postural response size based on prior experience, and hypermetric postural responses may be related to this deficit.
Evaluate Ataxia of Posture in a Clinical Setting
Ataxia has a profound effect on the ability to stand, especially when sensory information from vision is reduced and with a narrow base of support. Thus, the most sensitive tests of ataxia of posture control involve standing with eyes closed and with the feet together, tandem, and on one foot, if possible. Often a ratio of standing duration (up to 60 s) with and without vision available is included (Romberg ratio) to focus on the ability to control standing balance when somatosensory and visual inputs must be relied upon. Sitting balance without back support, and sometimes without foot support, is useful for patients who cannot stand unsupported. Because anticipatory postural adjustments are hypermetric, it can also be helpful to examine standing balance associated with rapid, voluntary movements such as step initiation, stepping onto a stair, and bilateral arm raising with weights [111]. Ataxia is seen as excessive trunk instability due to inappropriate anticipatory muscle activation in the legs and trunk. Because postural responses are hypermetric, a manual “Push and Release test” can be used to examine the ability to take a single step to recover equilibrium in response to external perturbations [174]. A patient leans into the examiner’s hands on their scapula just until their body weight is supported, before a rapid release of force. Ataxia is seen as rapid stepping with abnormal, lateral stepping and excessive trunk disequilibrium in response to release from a backward lean.
The quiet stance, anticipatory postural adjustments, and postural responses mentioned above can easily be quantified in clinical environments using body-worn, inertial sensors (IMUs) [175]. For example, a two-axis accelerometer on the lumbar segment can be used to quantify anterior/posterior and lateral postural sway area, velocity, and frequency during quiet stance in standing or sitting [176]. Ataxia is reflected in larger than normal sway area, velocity, and frequency but the direction of the excessive sway depends upon the type of ataxia [159]. A Romberg quotient with sway area eyes closed/eyes open larger than 1.5 would be considered abnormal. Quantification of postural sway allows for more sensitive measures of subtle impairment and more sensitive measures of change in postural control than rating scales. Recently, anticipatory postural adjustments have also been quantified with an IMU on the lumbar segment and legs to substitute for the traditional laboratory center of pressure measures [176]. The Push and Release test has also been instrumented with body-worn, inertial sensors to quantify postural response latency, compensatory step size and speed, and time to recover equilibrium [177]. Thus, postural ataxia can now be assessed in the clinic using a stop watch to measure quiet stance duration under challenging conditions, such as the feet together, eyes closed condition. In addition, body-worn sensor technology will soon be available to quantify ataxic hypermetria of postural sway, anticipatory postural adjustments, and postural responses quickly in the clinic. Instrumented tests have the advantage of being more sensitive and specific than clinical tests, albeit with added time and expense.
Eye Movements: Saccades
A. Butala, D.S. Zee, Baltimore, USA
Saccades are fast and fleeting, minimizing the time retinal image smearing precludes useful vision. The intrinsic association with vision and direction/initiation of attention means saccades have widespread cortical localization including every lobe of the cerebral cortex, limbic regions, and basal ganglia. The superior collicus (SC) is the final conduit to the brainstem and the substantia nigra pars reticulata (SNpr) helps gate a decision process about “what to look at” and “when.” The cerebellum plays a key role as the monitor of the accuracy of movements of all types, and accordingly, assures saccade accuracy in the face of normal development, aging, disease, or trauma. Saccades are biomarkers extraordinaire for investigating physiology, cognitive functions, as well as pathophysiology and diagnosis of disease. The characteristics of saccades, especially speed and accuracy, are easy to evaluate and have specific anatomical, pathological correlations that are useful clinically [180].
The premotor commands that drive the ocular motor neurons to generate the saccade are produced by burst neurons within the pons in the pontine paramedian reticular formation (PPRF) for horizontal saccades and within the midbrain in the rostral interstitial nucleus of the MLF (riMLF) for vertical saccades.
The Cerebellum and Saccades
The ocular motor vermis (lobules 5–7) (OMV) and its underlying projection site in the posterior fastigial nucleus called the fastigial oculomotor region (FOR) are the key areas within the cerebellum that control saccades. The FOR projects to the brainstem saccade generators and, acting as a brake, terminates the burst neuron discharge when the saccade reaches its target goal [181]. Since Purkinje cells inhibit their target neurons in the deep nuclei, the effects of deep nuclei lesions are the reciprocal of vermal lesions. Accordingly, lesions of the FOR lead to saccade overshooting or hypermetria while lesions of the overlying dorsal vermis lead to saccade undershooting or hypometria. Each FOR acts to inhibit ipsilateral saccades and promote contralateral saccades so that unilateral dysfunction of the FOR leads to overshooting of ipsilesional-directed saccades. Likewise, each side of the cerebellar vermis acts to facilitate ipsilateral saccades and inhibit contralateral saccades so that unilateral dysfunction of the vermis leads to undershooting of ipsilesional-directed saccades [182]. Thus, depending on the relative degree and asymmetry of cerebellar malfunction, different patterns of saccade dysmetria can appear. In contrast, saccade speed and saccade initiation (latency) are little affected by lesions restricted to the cerebellum. Some parts of the cerebellar hemispheres adjacent to the OMV and their projection sites in the more lateral cerebellar deep nuclei may also be involved in higher-level, more voluntary control of saccades, e.g., antisaccades, but these types of abnormalities are not easily appreciated clinically [183].
Clinical Examination of Saccades and Considerations on Saccade Pathology and Localization [184]
Range of Motion
The first consideration in the assessment of saccades is whether there is a primary problem with the eye muscles themselves that is limiting the range of motion. To assess range, ask the patient to look in the nine cardinal directions of gaze. If there is a limitation of range, a supranuclear process must be excluded, using other stimuli, such as a slowly moving target, optokinetic tape or mirror, or passive head rotations, to show that the range of motion can be improved using tracking or vestibular mechanisms. If so, this establishes a supranuclear component to the deficit. A typical example is a restriction of voluntary vertical gaze in patients with the Richardson variant of progressive supranuclear palsy (PSP) or Niemann Pick type C, both of which conditions may have ataxia as a prominent component. Range of motion of ocular movements is readily assessed by several methodologies reviewed later.
Velocity
Reduced velocity of voluntary, visually guided saccades is appreciated when patients are asked to make saccades between two relatively widely spaced targets, such as between the examiner’s finger, placed eccentrically, and the examiner’s nose. Slow horizontal or vertical saccades result from lesions affecting burst neurons within the PPRF and riMLF, respectively. Typical examples are slowing of horizontal saccades in spinocerebellar ataxia type 2 (SCA2) [185] and of vertical saccades in Whipple’s disease, Niemann-Pick type C [186], and PSP [187]. Quantification of saccade speed with recording devices can document slowing of saccades. The normal peak velocity–amplitude relationship for saccades is known as the “main sequence.” Unfortunately, the range of maximum peak velocities in normal subjects is wide so that multiple measures over time are often required to document a progressive decrease in saccade speed. Velocity and trajectory measurements require high bandwidth (150–300 Hz) for accurate and reproducible results.
Accuracy
Saccade accuracy is examined similarly, asking the patient to make saccades on command to the eccentrically located finger and then back to the examiner’s nose in both hemifields of gaze. Corrective saccades are the signature of dysmetria as one infers whether the first saccade was hyper- or hypometric based on the direction of the correction. Extreme hypermetria, usually with fastigial nucleus lesions, leads to macrosaccadic oscillations in which case repetitive, overshooting saccades take the eyes back and forth about the position of the target as a saccade small enough to just reach the target cannot be made. Extreme hypometria is a feature of lesions in the dorsal vermis. Similar to speed assessment, accurate gain measurement requires high bandwidth temporal resolution oculography.
Initiation
Saccade initiation defects, resulting in increased saccade latency, are only appreciated at the bedside if they are marked, and are best quantified with eye movement recordings. Increased latencies are not a feature of pure cerebellar disease, but imply cerebral hemisphere or basal ganglia disturbances [e.g., ataxia telangectasia (AT) or ataxia with oculomotor apraxia (AOA)]. Patients with saccade initiation defects often have conspicuous overshooting head movements and are mislabeled as having an apraxia [188]. Prolonged latency, lasting milliseconds, necessitates high temporal resolution detection coupled against prompted visual stimuli.
Saccade Testing Batteries
Since an early cerebellar component is often a feature of many neurodegenerative disorders that also involve the cerebral hemispheres, basal ganglia, or brainstem, it is important to evaluate eye movements in ataxia patients in the context of what might be accounted for by extracerebellar pathology. A battery of testing paradigms (antisaccades, memory-guided saccades, scanning saccades, sequence of saccades, predictive saccades, etc.) is available, and certain patterns of saccade abnormalities often help in localization and diagnosis. These types of abnormalities are best appreciated when eye movements are recorded and quantified in response to carefully controlled stimuli. Contemporary, non-invasive, video-based, recording techniques are well tolerated, easily applied, and quantitative, [189] integrating both high-temporal and spatial resolutions required for reproducible and accurate measurement. Typical examples of patterns of abnormalities of saccades associated with extracerebellar deficits include (1) the relative sparing of reflexive saccades to a novel stimulus versus difficulty in making internally-generated saccades, rapidly back and forth, between fixed stationary targets, as occurs in Parkinson’s disease; (2) slowed vertical saccades with profoundly hypometric horizontal saccades and incessant, prominent horizontal saccade intrusions (square-wave jerks) in progressive supranuclear palsy; and (3) marked inability to suppress reflexive saccades toward a novel visual stimulus when the instruction is to look away, at the mirror location, from the visual target (the antisaccade test) as occurs in Huntington’s disease [190].
To reiterate the main points about saccades and cerebellar disease: inaccuracy is the most prominent and consistent sign of saccade dysfunction in cerebellar disease. Saccade inaccuracy can usually be discerned at the bedside with simple visual inspection and is also easily quantified with eye movement recordings. Slowing of saccades can often be appreciated at the bedside, but subtle degrees require quantification with eye movement recordings. Slow saccades imply pathology in the brainstem reticular formation where premotor commands are generated. Defects in saccade initiation are not a feature of pure cerebellar disease. They are usually best appreciated by measuring latencies with eye movement recordings.
Eye Movements: Vestibulo-Ocular Reflex
A. Butala, D.S. Zee, Baltimore, USA
A careful examination of the vestibular system is essential for the evaluation of cerebellar ataxia. Not only do cerebellar lesions often lead to vestibular abnormalities, but many ataxia syndromes are associated with profound loss of vestibular function, which has both diagnostic and therapeutic (for rehabilitation) implications. The advent of new bedside clinical examination techniques and easy-to-use video-oculography (VOG) has made the clinical and quantitative evaluation of the vestibular system easy.
The most primitive part of the cerebellum—called the archi- or vestibulocerebellum—is extensively interconnected with the vestibular and other brainstem nuclei and also receives afferents directly from the labyrinth. Thus, it is not surprising that vestibular dysfunction is common in patients with cerebellar disease. The relevant anatomical structures in the cerebellum are the flocculus, paraflocculus (tonsil), ventral uvula, and nodulus. These structures project to the deep cerebellar nuclei and directly to the brainstem vestibular nuclei, where they can influence the direct, three-neuron arc of the vestibulo-ocular reflex (VOR) as it traverses the brainstem. We emphasize three key vestibuloocular reflexes: (1) the rotational VOR, responding to angular acceleration sensed by the semicircular canals (SCC), transduces head rotation; (2) the translational VOR, responding to linear acceleration sensed by the otolith organs, transduces head translation; and (3) the ocular counter-rolling (torsion) reflex (OCR), responding to the change in linear acceleration associated with static tilt of the head with respect to gravity. The OCR reflex, which aims to keep the retina aligned with the direction of the pull of gravity, is vestigial in humans but in pathology often becomes a prominent source of symptoms with accompanying corresponding signs. Positional nystagmus is another common finding in ataxia patients. It is caused by an abnormal response to the change in linear acceleration when the head is tilted with respect to gravity.
Disturbances of vestibular reflexes can be static, i.e., with the head still, when there is a tone imbalance in the resting activity of the vestibular nuclei. They are manifested as spontaneous nystagmus due to imbalance in semicircular canal activity, and a subjective tilt of the visual world [with associated counterrolling (torsion) of the globes] from imbalance in utricular activity. With ocular counterrolling, there may also be a head tilt and skew deviation (vertical misalignment of the eyes). This constellation of signs is known as the ocular tilt reaction (OTR) [191].
Dynamic imbalance occurs during head rotations or translations when the response of the VOR does not match what is needed to compensate correctly for the associated head motion. This leads to blurred vision (oscillopsia) during head movement. Dynamic disturbances can be related to hypofunction (e.g., a loss of labyrinthine responsiveness), hyperfunction (e.g., increased amplitude of response as can occur in cerebellar disease), or misdirected responses (e.g., vertical slow phase with a horizontal head rotation).
Clinical Examination of the VOR: Pathological Correlates
Static Disturbances
Spontaneous nystagmus, as an indicator of a static vestibular imbalance in the SCC, is best looked for first with fixation eliminated (e.g., using lenses which blur the patient’s view) and then compared with fixation allowed. With many central lesions, including cerebellar disease involving the flocculus and paraflocculus (tonsil), there is a failure of the normal ability to use vision to suppress an unwanted spontaneous nystagmus. This abnormality is closely tied to coexisting defects in smooth pursuit and cancellation of vestibular responses when patients track targets moving with the head. Many such patients also have a spontaneous downbeating nystagmus that is usually not suppressed by visual fixation. It likely reflects an imbalance in the inhibitory cerebellar influences over vertical semicircular canal pathways in the brainstem. Gaze-evoked nystagmus on attempted far lateral gaze often occurs with downbeat nystagmus and impaired smooth pursuit; together, these are the characteristic eye movement abnormalities associated with the lesions in the flocculus/paraflocculus (tonsil) [192].
Ocular counter-rolling (torsion) is an indicator of a static vestibular imbalance in the otolith system It is best inferred from measuring the subjective visual vertical (SVV). In this test, a patient is instructed to orient a vertical line parallel to their subjective sense of upright. It is readily performed at the bedside with the bucket test [193] in which patients must report when a line appears to be upright with no other visual cues available. The actual orientation of the eyes may be measured with fundus photography or various video methods [194]. Another feature of otolith imbalance may be a skew deviation (vertical misalignment of the eyes) that reflects the emergence of a phylogenetically old, ocular righting response of a lateral-eyed animal in response to lateral tilt of the head. Coupled with the ocular torsion, there is often tilt of the head, in the same direction as the counter-roll of the eyes, as part of the OTR. The OTR commonly occurs with lesions in the brainstem though less frequently with isolated cerebellar lesions.
Dynamic Disturbances
Assaying dynamic function of the VOR is centered around comparing the amplitude (and direction) of the compensatory eye movement, the slow-phase, to that of the stimulus, head motion. Quantitatively, is the gain (output eye movement/input head movement) = 1.0? One may begin with testing dynamic visual acuity (DVA). With the patient viewing a distance acuity chart and the head stationary, the lowest line the patient can read is ascertained. Then acuity is measured while shaking the head horizontally and then vertically at a frequency of at least 2 Hz. One notes the number of lines on the acuity chart lost with head shaking; more than two is abnormal. More objective and quantitative testing can be obtained by recording head movements and only displaying the acuity optotypes when the head has reached a specific speed [195, 196].
Head Impulse Test
Next, the VOR is assessed using the head impulse test (HIT) in which the subject fixes on a stationary object (such as the examiner’s nose) during a brief but high-acceleration movement of the head imparted by the examiner. The examiner monitors for corrective saccades (e.g., if the reflex is hypoactive the eye moves away from the point of fixation and a corrective saccade opposite to head rotation is needed to bring the fovea back to the center target). These corrective saccades can be overt, occurring after the head movement and easily seen on simple visual inspection, or covert, taking place during the head movement and difficult to discern by eye. While subject to artifacts, VOG goggles can still be used to quantify reliably both the gain of the slow phase and any corrective saccades [197,198,199]. In cerebellar disease, these measures of the VOR become excellent biomarkers for diagnosis (both acutely and chronically), progression, and response to treatment in patients [200, 201]. This is well illustrated in cerebellar ataxia, neuropathy, vestibular areflexia syndrome (CANVAS) in which there is profound loss of labyrinth function [202].
A common vexing clinical scenario which illustrates the practical use of the HIT is the determination whether a patient with acute onset isolated vertigo and spontaneous nystagmus has a stroke. These patients usually have a benign viral affliction of the inner ear but occasionally these symptoms herald a cerebellar infarction. Quantification of the HIT with VOG helps to determine whether the lesion might be central, and in some patients, points to which particular part of the cerebellum is at fault [203]. A positive HINTS algorithm—head impulse negative, nystagmus that changes direction depending on eccentric gaze direction, and a skew deviation—argues for a central lesion and patients must be evaluated for a stroke. Lesions of the flocculus (supplied by the anterior inferior cerebellar artery) are associated with decreased head impulse responses, while lesions in the tonsil and ventral uvula/nodulus (supplied by the posterior inferior cerebellar artery) are not. Another feature of the HIT response that points to cerebellar dysfunction is cross-coupling, i.e., the slow-phase response has a component that is not in the same direction as the head rotation. The most common pattern is an upward slow phase (and downward correction) with horizontal head rotations; this localizes to lesions in the vestibulocerebellum [204].
Head-Shaking-Induced Nystagmus and Tilt Suppression of Post-Rotatory Nystagmus
Two other dynamic tests are particularly useful for analysis and localization of cerebellar dysfunction: post head-shaking-induced nystagmus and tilt suppression of post-rotatory nystagmus [205]. Both are best evaluated using quantitative VOG. With a unilateral peripheral lesion, there is often a transient horizontal nystagmus following a short period (10–15 s) of brisk (2 Hz) horizontal head-shaking. The slow phases are directed toward the side of the hypofunctioning labyrinth. With cerebellar lesions and especially when the nodulus/uvula is affected, the post-head shaking nystagmus usually has different characteristics; a vertical component, a rapid reversal phase, or being in the opposite direction to any spontaneous nystagmus. Tilt suppression of post-rotatory nystagmus is also abnormal with uvula-nodulus lesions; there is a loss of the normal suppression of post-rotatory nystagmus when the head is tilted just after the chair stops rotating (as reflected in the time constant of decay of post-rotatory nystagmus). This abnormality shows the importance of the nodulus in the normal inhibitory control over the vestibular velocity-storage mechanism in the brainstem. This mechanism perseverates vestibular responses beyond what the SCC sense when the head rotates at a constant speed. Lesions of the nodulus preclude inhibition of velocity-storage and, in extreme cases, leads to periodic alternating nystagmus, a classic sign of cerebellar disease.
Central Positional Nystagmus
Lastly, positional nystagmus is a cardinal sign of cerebellar disorder (especially implicating nodulus/uvula dysfunction). The two major types are (1) downbeat nystagmus provoked by placing the patient in a supine, head-hanging position, and (2) apogeotropic, direction-changing horizontal positional nystagmus (always beating skyward regardless of which ear is groundward). Both types have characteristics that differentiate them from the usual peripheral causes of positional nystagmus, posterior or lateral canal benign paroxysmal positional vertigo [206].
Quantitative Methodology for Evaluating Eye Movements in Patients with Suspected Cerebellar Dysfunction
Quantitative recordings are essential in neurology since they provide clinicians and researchers a simplified, reliable, and objective physiological biomarker complementary to the vagaries of historical and examination subjectivity [8]. A detailed description of the methodology and advantages and disadvantages of various types of eye movement recoding techniques can be found in appendix B of [8]. The earliest DC electro-oculography systems, though non-invasive, inexpensive and fairly accurate in horizontal range up to ± 40° are prone to electrical, muscle and lid artifact and not useful for vertical eye movements. Thus, for years, the magnetic-field search-coil technique, in which subjects sit in a weak magnetic field and wear a silastic scleral annulus in which a wire is embedded, has been the gold standard for reliability, reproducibility, and versatility for assessing eye movements. Magnetic search coils are sensitive to minute changes of arc with a wide linear range (± 180) in the horizontal and vertical and torsional rotations when eyes are open or closed. However, this technique has never been used in a routine laboratory setting because the scleral annulus and wire are uncomfortable and not tolerated by all subjects. There also is a small risk for corneal abrasions. In the last decade, there has been marked improvement in video recording techniques with higher frame rate and high-resolution. They are now in a portable, compact set of goggles, easily applied even at the bedside, and well tolerated by almost all patients. Their drawback is possible artifacts, primarily related to the position of the lids or slippage of the goggles on the head, which may make measures of eye velocity artificially high. An additional requirement now is that signal digitization for secondary processing requires increasing computation power for increasingly algorithmic and automated analysis. As for all eye movement recordings, patient alertness and cooperation are required. Despite these limitations, the VOG goggles provide relatively accurate measures for saccades and vestibular movements and, hence, much needed quantitative data [197]. Finally, we emphasize that the careful study of eye movements and vestibular responses in patients is a crucial ingredient to the successful diagnosis and management of the ataxic patient.
Discussion
Clearly, all authors agreed that standard electrophysiological measures are useful to demonstrate and, to a certain extent, quantify extracerebellar involvement in ataxias in daily practice. Many ataxias have accompanying polyneuropathy, spinal cord and brain stem involvement along with pyramidal tracts [11, 12, 21]. Although less common, epilepsy is also present in a subset of ataxias. All authors agreed that standard nerve conduction studies, sensory and motor evoked potentials, and electroencephalography should be performed as part of the diagnostic work-up in patients with unexplained ataxia. Some findings are highly characteristic. For example, sensory axonal polyneuropathy is a typical finding in Friedreich’s ataxia, and motor evoked potentials (MEP) show increased central motor conduction times in spinocerebellar ataxia type 1 (SCA1) [15, 26]. The presence of significant polyneuropathy and spinal cord involvement, on the other hand, makes the diagnosis of spinocerebellar ataxia type 6 (SCA6) or the cerebellar type of multisystem atrophy (MSA-C) very unlikely [22]. None of the electrophysiological findings, however, are specific to only one type of ataxia. There are ataxias with similar phenotypes, e.g., ataxia with vitamin E deficiency (AVED) resembles FRDA [31], on the one hand, and different phenotypes of the same type of ataxia on the other hand. Finally, many ataxias are accompanied by polyneuropathy and spinal cord involvement at least to some extent. That is, abnormalities found in standard electrophysiological testing may often be unspecific. Overall, compared to nerve conduction studies and sensory and motor evoked potentials, EEG may only play a secondary role. Whereas EEG may play an adjunctive role in a subset of ataxias which can present with epilepsy (e.g., SCA10, episodic ataxias), for the most part EEG findings are nonspecific in ataxias [64, 70]. In contrast, rigorous and standardized clinical assessment of saccades and the vestibuloocular reflex, coupled with quantitative recordings using infrared goggles or other recording devices may be sensitive and specific to cerebellar dysfunction in ataxias [8].
All electrophysiological measures, however, are easily available and inexpensive. The authors recommend performing electrophysiological assessments including EEG to get a most complete picture of the patients’ phenotype. Together with the family history, the clinical signs and brain MRI findings provide clues to ataxic subtype and, consequently, inform further genetic testing. On the other hand, when results are unclear with genetic panels or whole exome sequencing (such as with variants of unknown significance or mutations not deemed pathogenic), electrophysiological phenotyping can help determine whether or not a given phenotype matches with probable abnormal genetic findings. Yet, for many types of ataxias, comprehensive studies of electrophysiological measures are missing. Up to now, the majority of studies have been performed only in patients with SCA1, 2, 3, and 6. The authors agree that future studies describing the phenotype of, e.g., newly discovered ataxia-genes should include a full standard electrophysiological assessment. Finally, review of the literature shows that nerve conduction studies and MEPs can be abnormal in the presymptomatic state of SCAs [25, 38]. Thus electrophysiological measures may be helpful to define the onset of the disease and, therefore at which time future treatments should start. The authors agree that future studies are warranted to investigate whether these electrophysiological measures are sensitive enough to show small changes, and can be used as biomarkers in clinical trials.
As yet, there is lack of a singular holistic electrophysiological measure that addresses all functions of the cerebellum. All authors agree that it is worthwhile to explore the usefulness of cerebellar brain inhibition (CBI) in future studies. CBI is a measure of cerebellar-motor cortex (M1) connectivity which allows to indirectly infer the state of cerebellar excitability [49]. CBI may be of particular use in early stages of the disease where it is frequently difficult to decide whether or not there is involvement of the cerebellum. CBI may also provide additional knowledge on the pathophysiology of ataxias, i.e., to localize the anatomical origin of ataxias (efferent vs. afferent pathways). Findings should also be different in ataxias affecting primarily the cerebellar cortex or the nuclei (at least in the beginning of the disease when little secondary changes have been taken place). CBI, however, is based on a paired-pulse TMS paradigm which needs not only two coils and magnetic stimulators, but more significant, operator expertise and patient cooperation. Future studies are needed to investigate the feasibility and usefulness of CBI as part of the routine diagnostic work-up of ataxias.
The authors agree that quantitative assessments of the leading cerebellar signs—that is dysarthria, ataxia of stance and gait, and foremost disordered eye movements—are of limited additional use in the diagnostic work-up in ataxias in the daily practice. Quantitative assessments usually do not provide significantly more information compared to a thorough clinical examination. For example, the ability of most quantitative measures to differentiate between different causes of balance and gait problems is limited. There is, e.g., no single parameter which allows the unequivocal conclusion of a cerebellar deficit. Recording of eye movement is an exception, but here, as explained in detail in this article, a comprehensive clinical examination does not fall short. A detailed examination of eye movements can be very helpful to decide whether or not there is cerebellar involvement and/or extracerebellar signs.
There is increasing need in the field of ataxias for sensitive biomarkers, in particular to monitor very early stages of disease. An increasing number of treatment trials are in the pipeline. These trials include both drug and rehabilitation interventions, the latter including physiotherapy and speech therapy. In the interest in satisfying the Food and Drug Administration’s (USA) mandate that drug trials employ meaningful outcome measures, metrics that measure vision, talking, and walking are increasingly important. Here, clinical measures lack sensitivities despite the development of validated clinical ataxia scores [104]. Quantitative measures of ataxia as yet largely depend on expensive and advanced equipment, e.g., force plates and multiple camera systems. Currently, systems on the basis of body-worn sensor technology are developed to quantify gait and balance performance in daily life. More portable measures of eye movements exist and these may serve as a proxy for cerebellar dysfunction in gait and posture. For example, quantifying the amplitude (gain) of the vestibulo-ocular reflex can be correlated with other measures of progression in patients with SCA6 [200]. All of these systems will allow assessment of treatment responses during daily life, for instance quantifying the improvement in gait variability and body sway at home or walking outside.
The authors note that ataxias are also frequently accompanied by dysphagia [207] and sleeping disorders. Polysomnography and clinical and instrumental swallowing diagnostics are helpful tools, which should be applied on a more regular basis in ataxia patients.
In summary, the authors recommend performing standard electrophysiological measures including nerve conduction studies, sensory and motor evoked potentials, and EEG in all patients with newly diagnosed ataxias. Whether or not these measures are useful biomarkers need to be established in future studies. Future studies are also needed to explore whether cerebellar brain inhibition (CBI), which addresses cerebellar function more directly, is a useful additional TMS measure. Quantitative measures of ataxia and eye movements are likely useful biomarkers, but this also needs to be investigated in the future.
References
Teive HA, Ashizawa T. Primary and secondary ataxias. Curr Opin Neurol. 2015 Aug;28(4):413–22.
Beaudin M, Klein CJ, Rouleau GA, Dupre N. Systematic review of autosomal recessive ataxias and proposal for a classification. Cerebellum Ataxias. 2017;4:3.
Synofzik M, Schule R. Overcoming the divide between ataxias and spastic paraplegias: shared phenotypes, genes, and pathways. Mov Disord. 2017 Mar;32(3):332–45.
Klockgether T. Sporadic ataxia with adult onset: classification and diagnostic criteria. Lancet Neurol. 2010 Jan;9(1):94–104.
Koeppen AH, Mazurkiewicz JE. Friedreich ataxia: neuropathology revised. J Neuropathol Exp Neurol. 2013 Feb;72(2):78–90.
van de Warrenburg BP, Schouten MI, de Bot ST, Vermeer S, Meijer R, Pennings M, et al. Clinical exome sequencing for cerebellar ataxia and spastic paraplegia uncovers novel gene-disease associations and unanticipated rare disorders. Eur J Human Genet : EJHG. 2016 Oct;24(10):1460–6.
Valero-Cuevas FJ, Hoffmann H, Kurse MU, Kutch JJ, Theodorou EA. Computational models for neuromuscular function. IEEE Rev Biomed Eng. 2009;2:110–35.
Leigh RJ, Zee DS. The neurology of eye movements. USA: Oxford University Press; 2015.
Anheim M, Tranchant C, Koenig M. The autosomal recessive cerebellar ataxias. N Engl J Med. 2012 Feb 16;366(7):636–46.
Liang L, Chen T, Wu Y. The electrophysiology of spinocerebellar ataxias. Neurophysiol Clin. 2016 Feb;46(1):27–34.
Schols L, Amoiridis G, Buttner T, Przuntek H, Epplen JT, Riess O. Autosomal dominant cerebellar ataxia: phenotypic differences in genetically defined subtypes? Ann Neurol. 1997 Dec;42(6):924–32.
Schols L, Linnemann C, Globas C. Electrophysiology in spinocerebellar ataxias: spread of disease and characteristic findings. Cerebellum. 2008;7(2):198–203.
van de Warrenburg BP, Notermans NC, Schelhaas HJ, van Alfen N, Sinke RJ, Knoers NV, et al. Peripheral nerve involvement in spinocerebellar ataxias. Arch Neurol. 2004 Feb;61(2):257–61.
Anheim M, Monga B, Fleury M, Charles P, Barbot C, Salih M, et al. Ataxia with oculomotor apraxia type 2: clinical, biological and genotype/phenotype correlation study of a cohort of 90 patients. Brain. 2009 Oct;132(Pt 10):2688–98.
Schöls L, Amoiridis G, Przuntek H, Frank G, Epplen JT, Epplen C. Friedreich's ataxia. Revision of the phenotype according to molecular genetics. Brain. 1997 Dec;120(Pt 12):2131–40.
Synofzik M, Srulijes K, Godau J, Berg D, Schols L. Characterizing POLG ataxia: clinics, electrophysiology and imaging. Cerebellum. 2012 Dec;11(4):1002–11.
El Euch-Fayache G, Bouhlal Y, Amouri R, Feki M, Hentati F. Molecular, clinical and peripheral neuropathy study of Tunisian patients with ataxia with vitamin E deficiency. Brain : J Neurol 2014 Feb;137(Pt 2):402-410.
Lelli S, Trevisan C, Ataxia-teleangectasia NP. neurophysiological studies in 8 patients. Electromyogr Clin Neurophysiol. 1995 Aug-Sep;35(5):311–5.
Le Ber I, Moreira MC, Rivaud-Pechoux S, Chamayou C, Ochsner F, Kuntzer T, et al. Cerebellar ataxia with oculomotor apraxia type 1: clinical and genetic studies. Brain : J Neurol. 2003 Dec;126(Pt 12):2761–72.
Gazulla J, Benavente I, Vela AC, Marin MA, Pablo LE, Tessa A, et al. New findings in the ataxia of Charlevoix-Saguenay. J Neurol. 2012 May;259(5):869–78.
Abele M, Burk K, Andres F, Topka H, Laccone F, Bosch S, et al. Autosomal dominant cerebellar ataxia type I. Nerve conduction and evoked potential studies in families with SCA1, SCA2 and SCA3. Brain. 1997 Dec;120(Pt 12):2141–8.
Linnemann C, Tezenas du Montcel S, Rakowicz M, Schmitz-Hubsch T, Szymanski S, Berciano J, et al. Peripheral neuropathy in spinocerebellar ataxia type 1, 2, 3, and 6. Cerebellum. 2016 Apr;15(2):165–73.
Klockgether T, Schols L, Abele M, Burk K, Topka H, Andres F, et al. Age related axonal neuropathy in spinocerebellar ataxia type 3/Machado-Joseph disease (SCA3/MJD). J Neurol Neurosurg Psychiatr. 1999 Feb;66(2):222–4.
Schols L, Amoiridis G, Epplen JT, Langkafel M, Przuntek H, Riess O. Relations between genotype and phenotype in German patients with the Machado-Joseph disease mutation. J Neurol Neurosurg Psychiatr. 1996 Nov;61(5):466–70.
Velazquez Perez L, Sanchez Cruz G, Canales Ochoa N, Rodriguez Labrada R, Rodriguez Diaz J, Almaguer Mederos L, et al. Electrophysiological features in patients and presymptomatic relatives with spinocerebellar ataxia type 2. J Neurol Sci. 2007 Dec 15;263(1-2):158–64.
Schols L, Riess O, Schols S, Zeck S, Amoiridis G, Langkafel M, et al. Spinocerebellar ataxia type 1: clinical and neurophysiological characteristics in German kindreds. Acta Neurolo Scand. 1995 Dec;92(6):478–85.
Velazquez-Perez L, Rodriguez-Labrada R, Canales-Ochoa N, Sanchez-Cruz G, Fernandez-Ruiz J, Montero JM, et al. Progression markers of Spinocerebellar ataxia 2. A twenty years neurophysiological follow up study. J Neurol Sci. 2010 Mar 15;290(1-2):22–6.
Schöls L, Bauer P, Schmidt T, Schulte T, Riess O. Autosomal dominant cerebellar ataxias: clinical features, genetics, and pathogenesis. Lancet Neurol. 2004 May;3(5):291–304.
David G, Durr A, Stevanin G, Cancel G, Abbas N, Benomar A, et al. Molecular and clinical correlations in autosomal dominant cerebellar ataxia with progressive macular dystrophy (SCA7). Hum Mol Genet. 1998 Feb;7(2):165–70.
Schwenkreis P, Tegenthoff M, Witscher K, Bornke C, Przuntek H, Malin JP, et al. Motor cortex activation by transcranial magnetic stimulation in ataxia patients depends on the genetic defect. Brain. 2002 Feb;125(Pt 2):301–9.
Zouari M, Feki M, Ben Hamida C, Larnaout A, Turki I, Belal S, et al. Electrophysiology and nerve biopsy: comparative study in Friedreich's ataxia and Friedreich's ataxia phenotype with vitamin E deficiency. Neuromuscul Disord. 1998 Aug;8(6):416–25.
Scarpini C, Mondelli M, Guazzi GC, Federico A. Ataxia-telangiectasia: somatosensory, brainstem auditory and motor evoked potentials in six patients. Dev Med Child Neurol. 1996 Jan;38(1):65–73.
Garcia A, Criscuolo C, de Michele G, Berciano J. Neurophysiological study in a Spanish family with recessive spastic ataxia of Charlevoix-Saguenay. Muscle Nerve. 2008 Jan;37(1):107–10.
Tremblay S, Austin D, Hannah R, Rothwell JC. Non-invasive brain stimulation as a tool to study cerebellar-M1 interactions in humans. Cerebellum Ataxias. 2016;3:19.
Celnik P. Understanding and modulating motor learning with cerebellar stimulation. Cerebellum. 2015 Apr;14(2):171–4.
Carrillo F, Palomar FJ, Conde V, Diaz-Corrales FJ, Porcacchia P, Fernandez-Del-Olmo M, et al. Study of cerebello-thalamocortical pathway by transcranial magnetic stimulation in Parkinson's disease. Brain Stimul. 2013 Jul;6(4):582–9.
Koch G, Porcacchia P, Ponzo V, Carrillo F, Caceres-Redondo MT, Brusa L, et al. Effects of two weeks of cerebellar theta burst stimulation in cervical dystonia patients. Brain Stimul. 2014 Jul-Aug;7(4):564–72.
Ragno M, Perretti AC, Castaldo I, Scarcella M, Acciarri S, Manganelli F, et al. Multimodal electrophysiologic follow-up study in 3 mutated but presymptomatic members of a spinocerebellar ataxia type 1 (SCA1) family. Neurol Sci. 2005 Jun;26(2):67–71.
Farrar MA, Vucic S, Nicholson G, Kiernan MC. Motor cortical dysfunction develops in spinocerebellar ataxia type 3. Clin Neurophysiol. 2016 Nov;127(11):3418–24.
Restivo DA, Giuffrida S, Rapisarda G, Antonuzzo A, Saponara R, Reggio A, et al. Central motor conduction to lower limb after transcranial magnetic stimulation in spinocerebellar ataxia type 2 (SCA2). Clin Neurophysiol. 2000 Apr;111(4):630–5.
Schols L, Amoiridis G, Langkafel M, Schols S, Przuntek H. Motor evoked potentials in the spinocerebellar ataxias type 1 and type 3. Muscle Nerve. 1997 Feb;20(2):226–8.
Yokota T, Sasaki H, Iwabuchi K, Shiojiri T, Yoshino A, Otagiri A, et al. Electrophysiological features of central motor conduction in spinocerebellar atrophy type 1, type 2, and Machado-Joseph disease. J Neurol Neurosurg Psychiatry. 1998 Oct;65(4):530–4.
Chen JT, Lin YY, Lee YC, Soong BW. Wu ZA, Liao KK. Prolonged central motor conduction time of lower limb muscle in spinocerebellar ataxia 6. J Clin Neurosci : Off J Neurosurg Soc Aust. 2004 May;11(4):381–3.
Restivo DA, Lanza S, Saponara R, Rapisarda G, Giuffrida S, Palmeri A. Changes of cortical excitability of human motor cortex in spinocerebellar ataxia type 2. A study with paired transcranial magnetic stimulation. J Neurol Sci. 2002 Jun 15;198(1-2):87–92.
Velazquez-Perez L, Rodriguez-Labrada R, Torres-Vega R, Medrano Montero J, Vazquez-Mojena Y, Auburger G, et al. Abnormal corticospinal tract function and motor cortex excitability in non-ataxic SCA2 mutation carriers: a TMS study. Clin Neurophysiol. 2016 Aug;127(8):2713–9.
Berardelli A, Abbruzzese G, Chen R, Orth M, Ridding MC, Stinear C, et al. Consensus paper on short-interval intracortical inhibition and other transcranial magnetic stimulation intracortical paradigms in movement disorders. Brain Stimul. 2008 Jul;1(3):183–91.
Schelhaas HJ, van de Warrenburg BP, Bos MM, Houtman CJ, Scheffer H, Gabreels-Festen A, et al. Neurophysiologic studies in early-onset cerebellar ataxia. J Clin Neurophysiol : Off Publ Am Electroencephalogr Soc. 2006 Aug;23(4):381–7.
Iwata NK, Ugawa Y. The effects of cerebellar stimulation on the motor cortical excitability in neurological disorders: a review. Cerebellum. 2005;4(4):218–23.
Ugawa Y, Terao Y, Hanajima R, Sakai K, Furubayashi T, Machii K, et al. Magnetic stimulation over the cerebellum in patients with ataxia. Electroencephalogr Clin Neurophysiol. 1997 Sep;104(5):453–8.
Matsunaga K, Uozumi T, Hashimoto T, Tsuji S. Cerebellar stimulation in acute cerebellar ataxia. Clin Neurophysiol. 2001 Apr;112(4):619–22.
Ugawa Y, Genba-Shimizu K, Rothwell JC, Iwata M, Kanazawa I. Suppression of motor cortical excitability by electrical stimulation over the cerebellum in ataxia. Ann Neurol. 1994 Jul;36(1):90–6.
Spampinato DA, Block HJ, Celnik PA. Cerebellar-M1 connectivity changes associated with motor learning are somatotopic specific. J Neurosci. 2017 Mar 1;37(9):2377–86.
Remillard G, Andermann F, Blitzer L, Andermann E. Electroencephalographic findings in Friedreich's ataxia. Can J Neurol Sci. 1976 Nov;3(4):309–12.
Anheim M, Chaigne D, Fleury M, Santorelli FM, De Seze J, Durr A, et al. Autosomal recessive spastic ataxia of Charlevoix-Saguenay: study of a family and review of the literature. Rev Neurol. 2008 Apr;164(4):363–8.
van Egmond ME, Verschuuren-Bemelmans CC, Nibbeling EA, Elting JW, Sival DA, Brouwer OF, et al. Ramsay Hunt syndrome: clinical characterization of progressive myoclonus ataxia caused by GOSR2 mutation. Mov Disord. 2014 Jan;29(1):139–43.
Girard JM, Turnbull J, Ramachandran N, Minassian BA. Progressive myoclonus epilepsy. Handb Clin Neurol. 2013;113:1731–6.
Canafoglia L, Gilioli I, Invernizzi F, Sofia V, Fugnanesi V, Morbin M, et al. Electroclinical spectrum of the neuronal ceroid lipofuscinoses associated with CLN6 mutations. Neurology. 2015 Jul 28;85(4):316–24.
Jansen AC, Andermann E. Progressive Myoclonus Epilepsy, Lafora Type. In: Adam MP, Ardinger HH, Pagon RA, Wallace SE, Bean LJH, Mefford HC, et al editors. GeneReviews((R)). Seattle (WA) 1993.
Gargouri-Berrechid A, Nasri A, Kacem I, Sidhom Y, Abdelkefi I, Hizem Y, et al. Long-term evolution of EEG in Unverricht-Lundborg disease. Neurophysiol Clin = Clin Neurophysiol. 2016 Apr;46(2):119–24.
Ito Y, Gertsen E, Oguni H, Nakayama T, Matsuo M, Funatsuka M, et al. Clinical presentation, EEG studies, and novel mutations in two cases of GLUT1 deficiency syndrome in Japan. Brain Dev. 2005 Jun;27(4):311–7.
Hully M, Vuillaumier-Barrot S, Le Bizec C, Boddaert N, Kaminska A, Lascelles K, et al. From splitting GLUT1 deficiency syndromes to overlapping phenotypes. Eur J Med Genet. 2015 Sep;58(9):443–54.
Rakowicz M, Zdzienicka E, Poniatowska R, Waliniowska E, Sulek A, Jakubowska T, et al. Spinocerebellar ataxias type 1 and 2: comparison of clinical, electrophysiological and magnetic resonance evaluation. Neurol Neurochir Pol. 2005 Jul-Aug;39(4):263–75.
Belluzzo M, Musho-Ilbeh S, Monti F, Pizzolato G. A case of nocturnal frontal lobe epilepsy in a patient with spinocerebellar ataxia type 17. Seizure. 2012 Dec;21(10):805–6.
Rasmussen A, Matsuura T, Ruano L, Yescas P, Ochoa A, Ashizawa T, et al. Clinical and genetic analysis of four Mexican families with spinocerebellar ataxia type 10. Ann Neurol. 2001 Aug;50(2):234–9.
Grewal RP, Achari M, Matsuura T, Durazo A, Tayag E, Zu L, et al. Clinical features and ATTCT repeat expansion in spinocerebellar ataxia type 10. Arch Neurol. 2002 Aug;59(8):1285–90.
Teive HA, Roa BB, Raskin S, Fang P, Arruda WO, Neto YC, et al. Clinical phenotype of Brazilian families with spinocerebellar ataxia 10. Neurology. 2004 Oct 26;63(8):1509–12.
Teive HA, Munhoz RP, Raskin S, Arruda WO, de Paola L, Werneck LC, et al. Spinocerebellar ataxia type 10: frequency of epilepsy in a large sample of Brazilian patients. Mov Disord. 2010 Dec 15;25(16):2875–8.
Licht DJ, Lynch DR. Juvenile dentatorubral-pallidoluysian atrophy: new clinical features. Pediatr Neurol. 2002 Jan;26(1):51–4.
Choi KD, Choi JH. Episodic ataxias: clinical and genetic features. J Mov Disord. 2016 Sep;9(3):129–35.
Jen JC, Graves TD, Hess EJ, Hanna MG, Griggs RC, Baloh RW, et al. Primary episodic ataxias: diagnosis, pathogenesis and treatment. Brain. 2007 Oct;130(Pt 10):2484–93.
Gardiner AR, Bhatia KP, Stamelou M, Dale RC, Kurian MA, Schneider SA, et al. PRRT2 gene mutations: from paroxysmal dyskinesia to episodic ataxia and hemiplegic migraine. Neurology. 2012 Nov 20;79(21):2115–21.
Van Bogaert P, Szliwowski HB. EEG findings in acetazolamide-responsive hereditary paroxysmal ataxia. Neurophysiol Clin = Clin Neurophysiol. 1996;26(5):335–40.
Traff J, Holme E, Ekbom K, Nilsson BY. Ekbom's syndrome of photomyoclonus, cerebellar ataxia and cervical lipoma is associated with the tRNA(Lys) A8344G mutation in mitochondrial DNA. Acta Neurol Scand. 1995 Nov;92(5):394–7.
Folker JE, Murdoch BE, Cahill LM, Delatycki MB, Corben LA, Vogel AP. Dysarthria in Friedreich’s ataxia: a perceptual analysis. Folia Phoniatr Logop. 2010;62(3):97–103.
Brendel B, Ackermann H, Berg D, Lindig T, Schölderle T, Schöls L, et al. Friedreich Ataxia: Dysarthria Profile and Clinical Data. Cerebellum. 2013 2013/08/01;12(4):475–84.
Rosen KM, Folker JE, Vogel AP, Corben LA, Murdoch BE, Delatycki MB. Longitudinal change in dysarthria associated with Friedreich ataxia: a potential clinical endpoint. J Neurol. 2012 2012/11/01;259(11):2471–7.
Schalling E, Hammarberg B, Hartelius L. A longitudinal study of dysarthria in spinocerebellar ataxia (SCA): aspects of articulation, prosody, and voice. J Med Speech Lang Pathol. 2008 2008/06//;16(2):103–14.
Yiu EM, Tai G, Peverill RE, Lee KJ, Croft KD, Mori TA, et al. An open-label trial in Friedreich ataxia suggests clinical benefit with high-dose resveratrol, without effect on frataxin levels. J Neurol. 2015 2015/04/07:1–10.
Schalling E, Hammarberg B, Hartelius L. Perceptual and acoustic analysis of speech in individuals with spinocerebellar ataxia (SCA). Logoped Phoniatr Vocol. 2007;32(1):31–46.
Vogel AP, Wardrop MI, Folker JE, Synofzik M, Corben LA, Delatycki MB, et al. Voice in Friedreich Ataxia. J Voice 2016.
Poole ML, Wee JS, Folker JE, Corben LA, Delatycki MB, Vogel AP. Nasality in Friedreich ataxia. Clin Linguist Phon. 2015;29(1):46–58.
Brendel B, Synofzik M, Ackermann H, Lindig T, Schölderle T, Schöls L, et al. Comparing speech characteristics in spinocerebellar ataxias type 3 and type 6 with Friedreich ataxia. J Neurol. 2015 2015/01/01;262(1):21–6.
Sidtis JJ, Ahn JS, Gomez C, Sidtis D. Speech characteristics associated with three genotypes of ataxia. J Commun Disord. 2011;44(4):478–92.
Vogel AP, Rommel N, Oettinger A, Horger M, Krumm P, Kraus E-M, et al. Speech and swallowing abnormalities in adults with POLG associated ataxia (POLG-A). Mitochondrion. 2017;
Vogel AP, Maruff P. Monitoring change requires a rethink of assessment practices in voice and speech. Logoped Phoniatr Vocol. 2014;39(2):56–61.
Vogel AP, Morgan AT. Assessment of impairment or monitoring change in Friedreich ataxia. Mov Disord. 2010 Aug 15;25(11):1753–4.
Tsanas A, Zañartu M, Little MA, Fox C, Ramig LO, Clifford GD. Robust fundamental frequency estimation in sustained vowels: Detailed algorithmic comparisons and information fusion with adaptive Kalman filtering. J Acoust Soc Am. 2014;135(5):2885–901.
Rosen KM, Murdoch BE, Folker JE, Vogel AP, Cahill L, Delatycki MB, et al. Automatic method of pause measurement for normal and dysarthric speech. Clin Linguist Phon. 2010;24(2):141–54.
Vogel AP, Fletcher J, Maruff P. The impact of task automaticity on speech in noise. Speech Comm. 2014;65:1–8.
Vogel AP, Poole ML, Pemberton H, Caverle MW, Boonstra F, Low E, et al. Motor speech signature of behavioral variant frontotemporal dementia: refining the phenotype. Neurology. 2017;
Vogel AP, Shirbin C, Churchyard AJ, Stout JC. Speech acoustic markers of early stage and prodromal Huntington's disease: a marker of disease onset? Neuropsychologia. 2012;50(14):3273–8.
Vogel AP, Fletcher J, Snyder PJ, Fredrickson A, Maruff P. Reliability, stability, and sensitivity to change and impairment in acoustic measures of timing and frequency. J Voice. 2011;25(2):137–49.
Vogel AP, Morgan AT. Factors affecting the quality of sound recording for speech and voice analysis. Int J Speech Lang Pathol. 2009;11(6):431–7.
Enderby P, Palmer R. Frenchay Dysarthria Assessment—Second Edition. Pro-Ed: Austin, TX; 2008.
Schmitz-Hübsch T, Giunti P, Stephenson DA, Globas C, Baliko L, Saccà F, et al. SCA Functional Index: a useful compound performance measure for spinocerebellar ataxia. Neurology. 2008 August 12, 2008;71(7):486–92.
Walshe M, Peach RK, Miller N. Dysarthria Impact Profile: development of a scale to measure psychosocial effects. Int J Lang Comm Disord. 2009;44(5):693–715.
Diener HC, Dichgans J. Cerebellar and spinocerebellar gait disorders. In: Bronstein AM, Brandt T, Woollacott, editors. Clinical disorders of posture and gait. London. 1996. p. 147–55.
Morton SM, Bastian AJ. Cerebellar control of balance and locomotion. Neuroscientist. 2004 Jun;10(3):247–59.
Ilg W, Timmann D. Gait ataxia-specific cerebellar influences and their rehabilitation. Mov Disord. 2013 Sep 15;28(11):1566–75.
Fonteyn EM, Schmitz-Hubsch T, Verstappen CC, Baliko L, Bloem BR, Boesch S, et al. Prospective analysis of falls in dominant ataxias. Eur Neurol. 2012 Nov 7;69(1):53–7.
Globas C, du Montcel ST, Baliko L, Boesch S, Depondt C, DiDonato S, et al. Early symptoms in spinocerebellar ataxia type 1, 2, 3, and 6. Mov Disord 2008 Nov 15;23(15):2232-2238.
Luo L, Wang J, Lo RY, Figueroa KP, Pulst SM, Kuo PH, et al. The initial symptom and motor progression in spinocerebellar ataxias. Cerebellum. 2016 Nov 15.
Trouillas P, Takayanagi T, Hallett M, Currier RD, Subramony SH, Wessel K, et al. International cooperative ataxia rating scale for pharmacological assessment of the cerebellar syndrome. The Ataxia Neuropharmacology Committee of the World Federation of Neurology. J Neurol Sci. 1997 Feb 12;145(2):205–11.
Schmitz-Hübsch T, du Montcel ST, Baliko L, Berciano J, Boesch S, Depondt C, et al. Scale for the assessment and rating of ataxia: development of a new clinical scale. Neurology. 2006 Jun 13;66(11):1717–20.
Jacobi H, Hauser TK, Giunti P, Globas C, Bauer P, Schmitz-Hubsch T, et al. Spinocerebellar ataxia types 1, 2, 3 and 6: the clinical spectrum of ataxia and morphometric brainstem and cerebellar findings. Cerebellum. 2012 Mar;11(1):155–66.
Morton SM, Tseng YW, Zackowski KM, Daline JR, Bastian AJ. Longitudinal tracking of gait and balance impairments in cerebellar disease. Mov Disord. 2010 Sep 15;25(12):1944–52.
Ilg W, Synofzik M, Brötz D, Burkard S, Giese MA, Schöls L. Intensive coordinative training improves motor performance in degenerative cerebellar disease. Neurology. 2009 Dec 1;73(22):1823–30.
Ilg W, Schatton C, Schicks J, Giese MA, Schols L, Synofzik M. Video game-based coordinative training improves ataxia in children with degenerative ataxia. Neurology. 2012 Nov 13;79(20):2056–60.
Powell LE, Myers AM. The activities-specific balance confidence (ABC) Scale. J Gerontol. 1995 Jan;50A(1):M28–34.
Yack HJ, Berger RC. Dynamic stability in the elderly: identifying a possible measure. J Gerontol. 1993 Sep;48(5):M225–30.
Horak FB, Wrisley DM, Frank J. The balance evaluation systems test (BESTest) to differentiate balance deficits. Phys Ther. 2009 May;89(5):484–98.
Ilg W, Golla H, Thier P, Giese MA. Specific influences of cerebellar dysfunctions on gait. Brain. 2007;130(3):786–98.
Palliyath S, Hallett M, Thomas SL, Lebiedowska MK. Gait in patients with cerebellar ataxia. Mov Disord. 1998 Nov;13(6):958–64.
Serrao M, Pierelli F, Ranavolo A, Draicchio F, Conte C, Don R, et al. Gait pattern in inherited cerebellar ataxias. Cerebellum. 2012 Mar;11(1):194–211.
Morton SM, Bastian AJ. Relative contributions of balance and voluntary leg-coordination deficits to cerebellar gait ataxia. J Neurophysiol. 2003 Apr;89(4):1844–56.
Stolze H, Klebe S, Petersen G, Raethjen J, Wenzelburger R, Witt K, et al. Typical features of cerebellar ataxic gait. J Neurol Neurosurg Psychiatry. 2002 Sep;73(3):310–2.
Wuehr M, Schniepp R, Ilmberger J, Brandt T, Jahn K. Speed-dependent temporospatial gait variability and long-range correlations in cerebellar ataxia. Gait Posture. 2013 Feb;37(2):214–8.
Milne SC, Hocking DR, Georgiou-Karistianis N, Murphy A, Delatycki MB, Corben LA. Sensitivity of spatiotemporal gait parameters in measuring disease severity in Friedreich ataxia. Cerebellum. 2014 Dec;13(6):677–88.
Martino G, Ivanenko YP, Serrao M, Ranavolo A, d'Avella A, Draicchio F, et al. Locomotor patterns in cerebellar ataxia. J Neurophysiol. 2014 Dec 1;112(11):2810–21.
Milne SC, Corben LA, Yiu E, Delatycki MB, Gastrocnemius G-KN. soleus spasticity and muscle length in Friedreich's ataxia. J Clin Neurosci : Off J Neurosurg Soc Aust. 2016 Jul;29:29–34.
Caliandro P, Iacovelli C, Conte C, Simbolotti C, Rossini PM, Padua L, et al. Trunk-lower limb coordination pattern during gait in patients with ataxia. Gait Posture. 2017 2017/09/01/;57:252–7.
Serrao M, Chini G, Casali C, Conte C, Rinaldi M, Ranavolo A, et al. Progression of gait ataxia in patients with degenerative cerebellar disorders: a 4-year follow-up study. Cerebellum. 2016 Dec 06.
Jacobi H, Reetz K, du Montcel ST, Bauer P, Mariotti C, Nanetti L, et al. Biological and clinical characteristics of individuals at risk for spinocerebellar ataxia types 1, 2, 3, and 6 in the longitudinal RISCA study: analysis of baseline data. Lancet Neurol. 2013 Jul;12(7):650–8.
Maas RP, van Gaalen J, Klockgether T, van de Warrenburg BP. The preclinical stage of spinocerebellar ataxias. Neurology. 2015 Jul 7;85(1):96–103.
Storey E. Presymptomatic features of spinocerebellar ataxias. Lancet Neurol. 2015;12(7):625–6.
Ilg W, Fleszar Z, Schatton C, Hengel H, Harmuth F, Bauer P, et al. Individual changes in preclinical spinocerebellar ataxia identified via increased motor complexity. Mov Disord. 2016 Dec;31(12):1891–900.
Rochester L, Galna B, Lord S, Mhiripiri D, Eglon G, Chinnery PF. Gait impairment precedes clinical symptoms in spinocerebellar ataxia type 6. Mov Disord. 2014 Feb;29(2):252–5.
Schniepp R, Wuehr M, Schlick C, Huth S, Pradhan C, Dieterich M, et al. Increased gait variability is associated with the history of falls in patients with cerebellar ataxia. J Neurol. 2014 Jan;261(1):213–23.
Schmitz-Hubsch T, Brandt AU, Pfueller C, Zange L, Seidel A, Kuhn AA, et al. Accuracy and repeatability of two methods of gait analysis—GaitRite und Mobility Lab—in subjects with cerebellar ataxia. Gait Posture. 2016 May 25;48:194–201.
Geerse DJ, Coolen BH, Roerdink M. Kinematic validation of a Multi-Kinect v2 instrumented 10-meter walkway for quantitative gait assessments. PLoS ONE. 2015;10(10):e0139913.
Muller B, Ilg W, Giese MA, Ludolph N. Validation of enhanced kinect sensor based motion capturing for gait assessment. PLoS ONE. 2017;12(4):e0175813.
Salarian A, Horak FB, Zampieri C, Carlson-Kuhta P, Nutt JG, Aminian K. iTUG, a sensitive and reliable measure of mobility. IEEE Trans Neural Syst Rehabil Eng. 2010;18(3):303–10.
Morton SM, Bastian AJ. Can rehabilitation help ataxia? Neurology. 2009 Dec 1;73(22):1818–9.
Panturin E. Maximizing functional recovery. Phys Ther. 1997 Oct;77(10):1112–3.
Ilg W, Brötz D, Burkard S, Giese MA, Schöls L, Synofzik M. Long-term effects of coordinative training in degenerative cerebellar disease. Mov Disord. 2010 Oct 15;25(13):2239–46.
Keller JL, Bastian AJ. A home balance exercise program improves walking in people with cerebellar ataxia. Neurorehabil Neural Repair. 2014 Oct;28(8):770–8.
Miyai I, Ito M, Hattori N, Mihara M, Hatakenaka M, Yagura H, et al. Cerebellar ataxia rehabilitation trial in degenerative cerebellar diseases. Neurorehabil Neural Repair. 2012 Jun;26(5):515–22.
Ilg W, Bastian AJ, Boesch S, Burciu RG, Celnik P, Claassen J, et al. Consensus paper: management of degenerative cerebellar disorders. Cerebellum. 2014 Apr;13(2):248–68.
Fonteyn EM, Heeren A, Engels JJ, Boer JJ, van de Warrenburg BP, Weerdesteyn V. Gait adaptability training improves obstacle avoidance and dynamic stability in patients with cerebellar degeneration. Gait Posture. 2014 May;40(1):247–51.
Schniepp R, Schlick C, Pradhan C, Dieterich M, Brandt T, Jahn K, et al. The interrelationship between disease severity, dynamic stability, and falls in cerebellar ataxia. J Neurol. 2016 Jul;263(7):1409–17.
Klenk J, Srulijes K, Schatton C, Schwickert L, Maetzler W, Becker C, et al. Ambulatory activity components deteriorate differently across neurodegenerative diseases: a cross-sectional sensor-based study. Neurodegener Dis. 2016;16(5-6):317–23.
Mitoma H, Hayashi R, Yanagisawa N, Tsukagoshi H. Characteristics of parkinsonian and ataxic gaits: a study using surface electromyograms, angular displacements and floor reaction forces. J Neurol Sci 2000 Mar 1;174(1):22-39.
Ilg W, Christensen A, Mueller OM, Goericke SL, Giese MA, Timmann D. Effects of cerebellar lesions on working memory interacting with motor tasks of different complexities. J Neurophysiol. 2013 Nov;110(10):2337–49.
Crowdy KA, Hollands MA, Ferguson IT, Marple-Horvat DE. Evidence for interactive locomotor and oculomotor deficits in cerebellar patients during visually guided stepping. Exp Brain Res. 2000 Dec;135(4):437–54.
Crowdy KA, Kaur-Mann D, Cooper HL, Mansfield AG, Offord JL, Marple-Horvat DE. Rehearsal by eye movement improves visuomotor performance in cerebellar patients. Exp Brain Res. 2002 Sep;146(2):244–7.
Timmann D, Horak FB. Perturbed step initiation in cerebellar subjects. 1. Modifications of postural responses. Exp Brain Res. 1998 Mar;119(1):73–84.
Conte C, Serrao M, Casali C, Ranavolo A, Silvia M, Draicchio F, et al. Planned gait termination in cerebellar ataxias. Cerebellum. 2012 Dec;11(4):896–904.
Mari S, Serrao M, Casali C, Conte C, Ranavolo A, Padua L, et al. Turning strategies in patients with cerebellar ataxia. Exp Brain Res. 2012 Oct;222(1-2):65–75.
Earhart GM, Bastian AJ. Selection and coordination of human locomotor forms following cerebellar damage. J Neurophysiol. 2001 Feb;85(2):759–69.
Morton SM, Dordevic GS, Bastian AJ. Cerebellar damage produces context-dependent deficits in control of leg dynamics during obstacle avoidance. Exp Brain Res. 2004 May;156(2):149–63.
Earhart GM, Fletcher WA, Horak FB, Block EW, Weber KD, Suchowersky O, et al. Does the cerebellum play a role in podokinetic adaptation? Exp Brain Res. 2002 Oct;146(4):538–42.
Morton SM, Bastian AJ. Cerebellar contributions to locomotor adaptations during splitbelt treadmill walking. J Neurosci. 2006 Sep 6;26(36):9107–16.
Ilg W, Giese MA, Gizewski ER, Schoch B, Timmann D. The influence of focal cerebellar lesions on the control and adaptation of gait. Brain. 2008 Nov;131(Pt 11):2913–27.
Fonteyn EM, Schmitz-Hubsch T, Verstappen CC, Baliko L, Bloem BR, Boesch S, et al. Falls in spinocerebellar ataxias: results of the EuroSCA fall study. Cerebellum 2010 Feb 16.
Peterka RJ. Sensorimotor integration in human postural control. J Neurophysiol. 2002 Sep;88(3):1097–118.
Macpherson JM, Horak F. Neural control of posture. In: Kandel ER, Schwartz J, Jessell TM, Siegelbaum SA, Hudspeth AJ, editors. Principles of Neural Science. 5th ed. New York: Elsevier; 2014. p. 811–22.
Horak FB, Nashner LM. Central programming of postural movements: adaptation to altered support-surface configurations. J Neurophysiol. 1986 Jun;55(6):1369–81.
Matsushima A, Yoshida K, Genno H, Murata A, Matsuzawa S, Nakamura K, et al. Clinical assessment of standing and gait in ataxic patients using a triaxial accelerometer. Cerebellum Ataxias. 2015;2:9.
Diener HC, Dichgans J, Bacher M, Gompf B. Quantification of postural sway in normals and patients with cerebellar diseases. Electroencephalogr Clin Neurophysiol. 1984 Feb;57(2):134–42.
Horak FB. Postural ataxia related to somatosensory loss. Adv Neurol. 2001;87:173–82.
Van de Warrenburg BP, Bakker M, Kremer BP, Bloem BR, Allum JH. Trunk sway in patients with spinocerebellar ataxia. Mov Disord. 2005 Aug;20(8):1006–13.
Schoch B, Hogan A, Gizewski ER, Timmann D, Konczak J. Balance control in sitting and standing in children and young adults with benign cerebellar tumors. Cerebellum. 2010 Sep;9(3):324–35.
Bunn LM, Marsden JF, Giunti P, Day BL. Stance instability in spinocerebellar ataxia type 6. Mov Disord. 2013 Apr;28(4):510–6.
Jacobi H, Alfes J, Minnerop M, Konczak J, Klockgether T, Timmann D. Dual task effect on postural control in patients with degenerative cerebellar disorders. Cerebellum Ataxias. 2015;2:6.
Diener HC, Dichgans J, Guschlbauer B, Bacher M, Rapp H, Klockgether T. The coordination of posture and voluntary movement in patients with cerebellar dysfunction. Mov Disord. 1992;7(1):14–22.
Timmann D, Horak FB. Perturbed step initiation in cerebellar subjects: 2. Modification of anticipatory postural adjustments. Exp Brain Res. 2001 Nov;141(1):110–20.
Asaka T, Wang Y. Feedforward postural muscle modes and multi-mode coordination in mild cerebellar ataxia. Exp Brain Res. 2011 Apr;210(1):153–63.
Bruttini C, Esposti R, Bolzoni F, Vanotti A, Mariotti C, Cavallari P. Temporal disruption of upper-limb anticipatory postural adjustments in cerebellar ataxic patients. Exp Brain Res. 2015 Jan;233(1):197–203.
Diener HC, Dichgans J, Bacher M, Guschlbauer B. Characteristic alterations of long-loop "reflexes" in patients with Friedreich's disease and late atrophy of the cerebellar anterior lobe. J Neurol Neurosurg Psychiatr. 1984 Jul;47(7):679–85.
Horak FB, Diener HC. Cerebellar control of postural scaling and central set in stance. J Neurophysiol. 1994 Aug;72(2):479–93.
Mummel P, Timmann D, Krause UW, Boering D, Thilmann AF, Diener HC, et al. Postural responses to changing task conditions in patients with cerebellar lesions. J Neurol Neurosurg Psychiatr. 1998 Nov;65(5):734–42.
Bakker M, Allum JH, Visser JE, Gruneberg C, van de Warrenburg BP, Kremer BH, et al. Postural responses to multidirectional stance perturbations in cerebellar ataxia. Exp Neurol. 2006 Nov;202(1):21–35.
Timmann D, Prediction HFB. set-dependent scaling of early postural responses in cerebellar patients. Brain. 1997 Feb;120(Pt 2):327–37.
Jacobs JV, Horak FB, Van Tran K, Nutt JG. An alternative clinical postural stability test for patients with Parkinson's disease. J Neurol. 2006 Nov;253(11):1404–13.
Mancini M, Horak FB. Potential of APDM mobility lab for the monitoring of the progression of Parkinson's disease. Expert Rev Med Devices. 2016 May;13(5):455–62.
Mancini M, Salarian A, Carlson-Kuhta P, Zampieri C, King L, Chiari L, et al. ISway: a sensitive, valid and reliable measure of postural control. J Neuroeng Rehabil. 2012 Aug 22;9:59.
Smith BA, Carlson-Kuhta P, Horak FB. Consistency in administration and response for the backward push and release test: a clinical assessment of postural responses. Physiother Res Int. 2016 Mar;21(1):36–46.
Konczak J, Schoch B, Dimitrova A, Gizewski E, Timmann D. Functional recovery of children and adolescents after cerebellar tumour resection. Brain. 2005 Jun;128(Pt 6):1428–41.
Paquette C, Franzen E, Horak FB. More falls in cerebellar ataxia when standing on a slow up-moving tilt of the support surface. Cerebellum. 2016 Jun;15(3):336–42.
Pouget P. The cortex is in overall control of 'voluntary' eye movement. Eye (Lond). 2015 Feb;29(2):241–5.
Rucker JC, Ying SH, Moore W, Optican LM, Buttner-Ennever J, Keller EL, et al. Do brainstem omnipause neurons terminate saccades? Ann N Y Acad Sci. 2011 Sep;1233:48–57.
Eggert T, Robinson FR, Straube A. Modeling inter-trial variability of saccade trajectories: effects of lesions of the oculomotor part of the fastigial nucleus. PLoS Comput Biol. 2016 Jun;12(6):e1004866.
Kunimatsu J, Suzuki TW, Tanaka M. Implications of lateral cerebellum in proactive control of saccades. J Neurosci. 2016 Jun 29;36(26):7066–74.
Ramat S, Leigh RJ, Zee DS, Optican LM. What clinical disorders tell us about the neural control of saccadic eye movements. Brain. 2007 Jan;130(Pt 1):10–35.
Seifried C, Velazquez-Perez L, Santos-Falcon N, Abele M, Ziemann U, Almaguer LE, et al. Saccade velocity as a surrogate disease marker in spinocerebellar ataxia type 2. Ann Ny Acad Sci. 2005;1039(1):524–7.
Salsano E, Umeh C, Rufa A, Pareyson D, Zee DS. Vertical supranuclear gaze palsy in Niemann-Pick type C disease. Neurol Sci. 2012 Dec;33(6):1225–32.
Bhidayasiri R, Riley DE, Somers JT, Lerner AJ, Buttner-Ennever JA, Leigh RJ. Pathophysiology of slow vertical saccades in progressive supranuclear palsy. Neurology 2001 Dec 11;57(11):2070-2077.
Salman MS. Infantile-onset saccade initiation delay (congenital ocular motor apraxia). Curr Neurol Neurosci Rep. 2015 May;15(5):24.
Antoniades C, Ettinger U, Gaymard B, Gilchrist I, Kristjansson A, Kennard C, et al. An internationally standardised antisaccade protocol. Vision Res. 2013 May 24;84:1–5.
MacAskill MR, Anderson TJ. Eye movements in neurodegenerative diseases. Curr Opin Neurol. 2016 Feb;29(1):61–8.
Gresty MA, Bronstein AM, Brandt T, Dieterich M. Neurology of otolith function. Peripheral and central disorders. Brain. 1992;115(3):647–73.
Kheradmand A, Colpak AI, Zee DS. Chapter 8 - Eye movements in vestibular disorders. In: Joseph MF, Thomas L, editors. Handbook of Clinical Neurology. Volume 137: Elsevier; 2016. p. 103–17.
Zwergal A, Rettinger N, Frenzel C, Dieterich M, Brandt T, Strupp M. A bucket of static vestibular function. Neurology. 2009 May 12;72(19):1689–92.
Otero-Millan J, Roberts DC, Lasker A, Zee DS, Kheradmand A. Knowing what the brain is seeing in three dimensions: a novel, noninvasive, sensitive, accurate, and low-noise technique for measuring ocular torsion. J Vis. 2015;15(14):11.
Schubert MC, Migliaccio AA, Ng TW, Shaikh AG, Zee DS. The under-compensatory roll aVOR does not affect dynamic visual acuity. J Assoc Res Otolaryngol : JARO. 2012 Aug;13(4):517–25.
Colagiorgio P, Colnaghi S, Versino M, Ramat S. A new tool for investigating the functional testing of the VOR. Front Neurol. 2013;4:165.
Mantokoudis G, Saber Tehrani AS, Wozniak A, Eibenberger K, Kattah JC, Guede CI, et al. Impact of artifacts on VOR gain measures by video-oculography in the acute vestibular syndrome. J Vestib Res. 2016 Nov 03;26(4):375–85.
Chen L, Todd M, Halmagyi GM, Aw S. Head impulse gain and saccade analysis in pontine-cerebellar stroke and vestibular neuritis. Neurology. 2014 Oct 21;83(17):1513–22.
Mantokoudis G, Tehrani AS, Wozniak A, Eibenberger K, Kattah JC, Guede CI, et al. VOR gain by head impulse video-oculography differentiates acute vestibular neuritis from stroke. Otol Neurotol. 2015 Mar;36(3):457–65.
Huh YE, Kim JS, Kim HJ, Park SH, Jeon BS, Kim JM, et al. Vestibular performance during high-acceleration stimuli correlates with clinical decline in SCA6. Cerebellum. 2015 Jun;14(3):284–91.
Kattah JC, Dhanani SS, Pula JH, Mantokoudis G, Tehrani ASS, Toker DEN. Vestibular signs of thiamine deficiency during the early phase of suspected Wernicke encephalopathy. Neurology: Clin Pract. 2013;3(6):460–8.
Szmulewicz DJ, Roberts L, McLean CA, MacDougall HG, Halmagyi GM, Storey E. Proposed diagnostic criteria for cerebellar ataxia with neuropathy and vestibular areflexia syndrome (CANVAS). Neurol Clin Pract. 2016 Feb;6(1):61–8.
Newman-Toker DE, Saber Tehrani AS, Mantokoudis G, Pula JH, Guede CI, Kerber KA, et al. Quantitative video-oculography to help diagnose stroke in acute vertigo and dizziness: toward an ECG for the eyes. Stroke. 2013 Apr;44(4):1158–61.
Choi JY, Jung I, Jung JM, Kwon DY, Park MH, Kim HJ, et al. Characteristics and mechanism of perverted head-shaking nystagmus in central lesions: video-oculography analysis. Clin Neurophysiol. 2016 Sep;127(9):2973–8.
Lee SU, Choi JY, Kim HJ, Park JJ, Zee DS, Kim JS. Impaired tilt suppression of post-rotatory nystagmus and cross-coupled head-shaking nystagmus in cerebellar lesions: image mapping study. Cerebellum. 2016 Mar 11.
Choi JY, Kim JH, Kim HJ, Glasauer S, Kim JS. Central paroxysmal positional nystagmus: characteristics and possible mechanisms. Neurology. 2015 Jun 02;84(22):2238–46.
Keage MJ, Delatycki MB, Gupta I, Corben LA, Vogel AP. Dysphagia in Friedreich Ataxia. Dysphagia. 2017 May 4.
Beh SC, Frohman TC, Frohman EM. Neuro-ophthalmic manifestations of cerebellar disease. Neurol Clin. 2014 Nov;32(4):1009–80.
Beh SC, Frohman TC, Frohman EM. Cerebellar control of eye movements. J Neuroophthalmol : Off J North Am Neuroophthalmol Soc. 2017 Mar;37(1):87–98.
Choi JY, Nystagmus KJS. central vestibular disorders. Curr Opin Neurol. 2017 Feb;30(1):98–106.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interests
Rights and permissions
About this article
Cite this article
Ilg, W., Branscheidt, M., Butala, A. et al. Consensus Paper: Neurophysiological Assessments of Ataxias in Daily Practice. Cerebellum 17, 628–653 (2018). https://doi.org/10.1007/s12311-018-0937-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12311-018-0937-2