Abstract
Chronic obstructive pulmonary disease (COPD) is associated with high morbidity and mortality. COPD is typified by persistent, progressive airflow limitation and a range of respiratory and systemic symptoms such as breathlessness, coughing, wheezing, depression, anxiety, general fatigue, and sleeping difficulties. Despite receiving treatment for COPD, many patients suffer from regular symptoms that affect their daily lives and lead to increased morbidity. These symptoms vary in severity, frequency, and type, and can occur at any time throughout the 24-h day, with over half of patients with COPD experiencing symptoms in the morning, during the day, and at nighttime. Despite the prevalence of symptoms, patient and physician perception of the impact of COPD symptoms on patients’ lives is not always in concordance. Dual bronchodilator therapy with a long-acting muscarinic antagonist (LAMA) and long-acting beta agonist (LABA) has the potential to treat the symptoms of COPD in addition to improving lung function. This review therefore examines the burden of symptoms experienced throughout the day by patients with COPD and the evidence for combined LAMA/LABA treatment in terms of symptom management. As patients with COPD experience varying symptoms throughout the course of their disease, the role of tailoring treatment to the individual needs of the patient is also examined. We conclude that the symptoms of COPD are troublesome, variable, can occur during all parts of the 24-h day, and have a substantial impact on patients’ health status and quality of life. In order to provide effective, patient-orientated care, patients with COPD should be evaluated on the basis of lung function, the frequency of symptoms, and patient-perceived impact of symptoms on their lives. Therapy should be chosen carefully based on individualized assessment, ensuring personalization to the individual needs of the patient.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic obstructive pulmonary disease (COPD) is predicted to be the fourth leading cause of morbidity and mortality around the world by 2030, and confers an increasing socioeconomic burden [1]. The World Health Organisation estimates that, globally, 64 million people had moderate to severe COPD in 2004 [2], although the total burden of COPD is thought to be underestimated due to diagnosis usually only occurring when the disease is clinically apparent and moderately advanced [3]. The rise in morbidity and mortality from COPD over the next two decades is expected to be most dramatic in Asia and Africa, due in part to the progressive increase in the prevalence of smoking in these regions [2, 4].
COPD is characterized by expiratory airflow obstruction, reduced elastic recoil, and reduced parenchymal tethering [5]. Reduced elastic recoil leads to hyperinflation of the lungs, which impairs chest wall and diaphragm mechanics, making breathing more difficult and increasing dyspnea. As well as dyspnea, patients with COPD experience a range of symptoms, both respiratory and systemic; these symptoms and their severity can be highly variable [5].
There are currently several treatment options/actions for patients with COPD that can help to reduce and/or manage their symptoms, including pharmacologic therapies, pulmonary rehabilitation, and smoking cessation, all of which can also improve bronchodilation, reduce the frequency and severity of exacerbations, and improve health status and exercise tolerance [5]. However, many patients still suffer from regular symptoms that affect their daily lives and lead to increased morbidity. Therefore, selecting the right therapies and optimizing treatment to reduce airway obstruction and improve symptoms is key in improving quality of life for each patient with COPD.
This review examines the burden of symptoms experienced throughout the day by patients with COPD, the evidence for combined long-acting muscarinic antagonist and long-acting beta agonist (LAMA/LABA) treatment in terms of symptom management, and the role of tailoring treatment to the specific, individual needs of the patient.
Compliance with Ethics Guidelines
This article is based on previously conducted studies, and does not involve any new studies of human or animal subjects performed by any of the authors.
Daily Symptom Burden of COPD
Patients with COPD experience a range of symptoms that can vary greatly in severity. Symptoms can be respiratory-related, such as breathlessness, phlegm, cough, wheezing, and chest-tightness, as well as less specific symptoms relating to comorbidity, such as depression, anxiety, general fatigue, despondency, and sleeping difficulties [6]. Importantly, the majority of patients with COPD frequently continue to experience symptoms despite receiving treatment [6, 7].
COPD symptoms can vary in frequency, severity, and type throughout the 24-h period, often depending on the age of the patient and the severity of their disease, with morning and nighttime symptoms reported as being particularly troublesome [6, 8, 9]. When patients do experience variability or worsening of their symptoms, many do not know how to self-manage this therapeutically, and a large proportion simply continue to use their medication in the same way [6]. Table 1 provides a summary of studies of symptom variability in patients with COPD.
24-Hour Symptom Profile
COPD symptoms and variation in symptoms over a 24-h day were investigated in the ASSESS observational study, which explored the relationship between the 24-h symptom profile and patient-reported outcomes (PROs), using a novel, 33-item questionnaire developed by the sponsor of the study [7]. The study evaluated the prevalence and severity of symptoms over three periods: in the early morning, during the daytime, and at night [7]. Severity of airflow obstruction, health status, anxiety, depression, sleep quality, and physical activity were also evaluated to gauge the impact of symptoms. Over 90% of patients experienced COPD symptoms during at least one period of the 24-h day, and 57% of patients reported experiencing symptoms during all three periods. Stratification by disease severity revealed that even among patients with mild COPD, over 80% experienced symptoms during at least one part of the 24-h day [7].
In ASSESS, a significant relationship was seen between severity of disease and symptoms during the early morning and the daytime, with a higher percentage of patients with severe or very severe COPD experiencing symptoms in the morning and during the day versus those with mild or moderate disease [7]. However, the proportion of patients with nighttime symptoms was similar in patients with mild, moderate, severe, and very severe disease [7, 10]. Nearly two-thirds of patients experienced nighttime symptoms, regardless of the severity of the disease (Fig. 1a) [7].
a Percentage of patients experiencing symptoms in the early morning, the daytime, and at night, according to COPD severity; b prevalence of individual COPD symptoms throughout the 24-h day. COPD chronic obstructive pulmonary disease. Adapted from Miravitlles et al. 2014 (Copying and redistribution of the materials allowed in any medium or format: CC BY-NC 4.0) [7]
The prevalence of individual symptoms also varied throughout the 24-h period, with breathlessness being most prevalent overall, reported in around 70% of patients. In the early morning, coughing, bringing up phlegm, and breathlessness were reported in around half of patients. During the day, over two-thirds of patients with COPD experienced breathlessness, around half experienced coughing symptoms, and just under half reported bringing up phlegm. During the night, coughing was most prevalent amongst patients with COPD, being reported in around 42% of patients, with bringing up phlegm, breathlessness, and wheezing also reported in around a third of patients [7] (Fig. 1b).
A comparison between symptoms and COPD Assessment Test (CAT) scores in patients with COPD from ASSESS showed that patients with symptoms throughout the whole 24-h day had the worst health status versus those with no symptoms or with symptoms only in one part of the day [7]. The difference in CAT scores between patients with symptoms in all three parts of the 24-h day compared with patients without symptoms surpassed two units, the proposed estimate for a minimal clinically important difference (MCID) [7, 11]. In addition, both anxiety and depression levels were highest in patients who had symptoms in all three parts of the 24-h day and lowest in patients with no symptoms, or symptoms during only one part of the day [7].
Morning Symptoms
Symptoms of COPD experienced in the morning are known to impact on the ability of patients to carry out daily activities, such as walking up and down stairs, washing, and getting dressed [8], with a potential knock-on effect on the time of taking first COPD medications: one study showed that 35% of patients took their medication either whilst still in bed or immediately after getting up to relieve their COPD symptoms [8]. Patients with morning symptoms have also been shown to have higher CAT scores and lower EuroQol five dimensions questionnaire scores than those without morning symptoms, indicating a more serious impact on quality of life [12, 13]; these patients are also at increased risk of experiencing exacerbations [13].
Nighttime Symptoms
Symptoms of COPD experienced during the night can contribute to sleep disturbance, including difficulty falling asleep, staying asleep, and waking feeling tired, with symptoms affecting patients regardless of COPD severity [10]. In the ASSESS study, one or more symptoms was associated with a greater sleep impairment score at all three points during the 24-h day [7]. Such impairment or disruption of sleep is associated with reduced quality of life, as indicated by the Pittsburgh Sleep Quality Index score which is a significant predictor of disease-specific quality of life (as assessed using the St George’s Respiratory Questionnaire [SGRQ]) [14]. It is worth noting, however, that, in some cases, sleep disturbance could also be attributed to other causes, such as a side effect of medication for heart failure or prostate hypertrophy [15, 16].
In terms of predicted outcomes for patients with COPD, it has been reported that sleep disturbances among patients with COPD are predictive of poorer survival and increased rates of exacerbations and hospital admissions [17–19]. It has also been documented that the level of dyspnea correlates significantly to the 5-year survival rate of patients, and was more discriminating than percentage of predicted forced expiratory volume in 1 s (FEV1) in predicting 5-year survival, suggesting that consideration of symptoms of breathlessness alongside airway obstruction may provide a better prognostic indicator of COPD mortality [18, 20].
Patient and Physician Perceptions of COPD Symptoms
While a substantial body of evidence demonstrates the importance and impact of symptoms to patients, patient and physician perceptions of this impact may not always correspond. Overall, patients appear to underestimate their morbidity, and are possibly undertreated as a result [21]. Based on an objective breathlessness scale, in patients classified as too breathless to leave the house, a third described their condition as mild to moderate [21]. In another study, while both physicians and their patients identified breathlessness, fatigue, and coughing as the main symptoms of COPD that had most effect on patients’ lives [22], within the other symptom categories, such as expectoration, dry mouth, despondency, wheezing, sleeping difficulties, and chest pain, there were varying perceptions (in terms of rank) of the impact of these symptoms [22]. There was a greater degree of physician-patient concordance in patients with more severe COPD. Another study observed good concordance between the frequency of nighttime symptoms reported by patients and physicians, but also found that physicians significantly underestimated the impact of COPD symptoms on patients’ lives [10].
As current treatment options still lack control over symptoms, there remains a need for additional therapies. The exploration of treatment options that target both airway obstruction and COPD symptoms throughout the 24-h day may therefore provide patients with relief from the substantial impact that these symptoms can have on their health status.
The Utility of Dual Bronchodilation in COPD
Most patients with COPD report slight-to-moderate breathlessness across all severities of the disease with either a LAMA or a LABA, which are the current first-line Global Initiative for Chronic Obstructive Lung Disease (GOLD)-recommended treatments for patients with COPD [5]. LAMAs and LABAs have two different but complementary mechanisms of action [23, 24]: muscarinic antagonists block M1 and M3 receptors at the parasympathetic ganglia and on smooth muscle cells which inhibits the contraction of airway smooth muscle, while β2 agonists stimulate β2 receptors on smooth muscle cells which leads to the relaxation of airway smooth muscle via an independent but linked mechanism. Combination therapy with a LAMA and a LABA therefore has the potential to improve bronchodilation and symptoms in those patients whose COPD is not sufficiently controlled by monotherapy. The currently available LAMA/LABA combinations are aclidinium/formoterol, indacaterol/glycopyrronium, tiotropium/olodaterol, and umeclidinium/vilanterol. In addition, glycopyrrolate/formoterol has recently been approved in the USA [25].
Dual Bronchodilator Therapy and Lung Function
The lung-function benefits of these LAMA/LABA combination therapies are well established, with several large phase III clinical studies demonstrating that dual therapy improves trough, peak, and post-dose FEV1 versus placebo [26–30]. Data from these studies also show rapid and sustained improvements in trough FEV1 with dual therapies versus monotherapies, with the improvements in the region of 45–85 mL with aclidinium/formoterol, 52–95 mL with umeclidinium/vilanterol, 12–88 mL with tiotropium/olodaterol, and 70–90 mL with indacaterol/glycopyrronium [26–30]. A comprehensive review of dual therapy and a meta-analysis of dual bronchodilation with LAMA/LABA for the treatment of stable COPD have both shown that these treatments are effective with regards to lung function [31, 32]. ACLIFORM [33] and AUGMENT [28] were two 24-week, randomized, double-blind studies assessing the efficacy and safety of the combined LAMA/LABA therapy, aclidinium/formoterol, in patients with moderate-to-severe COPD. Post hoc analyses from ACLIFORM and AUGMENT determined that dual therapy with a LAMA/LABA improved lung function irrespective of severity of airflow obstruction, patient age, or use of concomitant inhaled corticosteroid (ICS) [34–36].
Dual Bronchodilator Therapy and Breathlessness
The Transition Dyspnea Index (TDI) is an interviewer-administered tool which assesses deterioration or improvement in breathlessness [37]. The TDI has been utilized in several studies which have reported a reduction in breathlessness in patients with COPD following treatment with dual therapies versus placebo [26, 28–30, 38, 39]. The potential for interviewer bias associated with the TDI has been addressed following subsequent development of a validated self-administered computerized version [40–43]. Many studies consistently report improvements with dual therapies that exceed one unit, the MCID for TDI focal score [28, 29, 38, 39], whereas monotherapies are unable to consistently show the same improvements [44]. Furthermore, responder analysis has shown that a greater proportion of individuals achieve a response >1 unit with dual bronchodilatory therapy compared to monotherapies [29, 38]. Additionally, in two of these studies, the PRO Shortness of Breath with Daily Activities (SOBDA) questionnaire scoring system was utilized to assess changes in breathlessness in patients with COPD, and showed that umeclidinium/vilanterol treatment groups saw improvements in their SOBDA score versus placebo [29, 45]. The SOBDA questionnaire is a more recently developed outcome measure that has been validated and uses a patient daily diary to better capture the inherent variability of dyspnea that is not adequately accounted for by other dyspnea-related PROs [45, 46]. Moreover, it can be further differentiated from other dyspnea-related PROs in that it was specifically developed to support FDA recommendations.
Dual Bronchodilator Therapy and EXACT-Respiratory Symptoms (E-RS) Score
Since reducing the severity of respiratory symptoms is a key goal in the treatment of COPD, it is important to use standardized methods for quantifying daily respiratory symptoms in clinical trials. EXAcerbations of Chronic obstructive pulmonary disease Tool (EXACT)-Respiratory Symptoms (E-RS™Footnote 1) is a PRO designed to assess the effect of treatment on the severity of symptoms (breathlessness, cough and sputum, and chest pains) in patients with COPD in clinical trials [47–49]. The E-RS has several advantages over other COPD-specific health status questionnaires, including use of daily scores to reduce recall bias, capture of daily variability in symptoms, and simultaneous assessment of exacerbation data and respiratory symptoms [47]. In two studies, aclidinium/formoterol produced significantly greater improvements in E-RS total score versus both placebo and the monotherapies [28, 39].
Dual Bronchodilator Therapy and Nighttime and Morning Symptoms
Although nighttime symptoms are known to negatively impact on health status, sleep disturbances, and healthcare resource utilization, current monotherapies may not adequately control these symptoms.
The Nighttime Symptoms of COPD Instrument (NiSCI) is a reliable, validated self-completed electronic daily diary (measuring nighttime symptom occurrence and severity, nocturnal awakening due to COPD symptoms, and nighttime rescue medication use in patients with COPD) that was recently developed to support treatment benefit endpoints in global clinical trials [50, 51]. The use of a daily diary within the NiSCI is intended to better capture the variability of nighttime symptoms and minimize recall bias; however, research is ongoing to define responders and evaluate COPD treatment responsiveness. Dual therapy with aclidinium/formoterol has been shown to produce significant improvements in overall nighttime symptom severity (measured using the NiSCI score) versus placebo, which aclidinium and formoterol alone did not achieve [28]. Additionally, nighttime symptom severity has been shown to significantly improve with aclidinium/formoterol versus aclidinium, with numerical improvements reported with aclidinium/formoterol versus formoterol [28]. This improvement in nighttime symptom severity with dual therapy has also been mirrored in patients receiving indacaterol/glycopyrronium, who experienced a significantly higher percentage of nights without awakenings versus placebo [38].
The Early Morning Symptoms of COPD Instrument (EMSCI) was also recently developed to support treatment benefit endpoints in clinical research and has demonstrated both reliability and validity in evaluating early-morning symptoms in COPD [52]. Dual therapy was found to improve early-morning symptom severity. In a 24-week study of patients with stable COPD, aclidinium/formoterol produced significant improvements in EMSCI score versus placebo, a result that was not replicated following treatment with monotherapies [28]. The dual therapy also significantly improved early-morning symptom severity versus monotherapies at some of the time points assessed [28].
Dual Bronchodilator Therapy and Quality of Life
Dual LAMA/LABA bronchodilator therapy appears to have a positive outcome on quality of life as assessed by the SGRQ total score. When compared with placebo, aclidinium/formoterol, umeclidinium/vilanterol, and indacaterol/glycopyrronium have all been shown to improve SGRQ total scores [26–30]. AUGMENT and ACLIFORM compared patients whose improvement in SGRQ was equal to or greater than four units, the MCID for SGRQ. A statistically greater proportion of patients receiving aclidinium/formoterol achieved the MCID than patients receiving placebo [28, 39]. Additionally, improvements in SGRQ total score were reported for indacaterol/glycopyrronium versus tiotropium monotherapy, and with tiotropium/olodaterol versus tiotropium and olodaterol monotherapy [27, 30]. Although the SGRQ provides a comprehensive assessment of COPD health status and has been widely used in clinical trials, it is considered overly complex for routine use in clinical practice; alternatives such as the COPD Assessment Test and the COPD Control Questionnaire are considered more appropriate [5, 53].
Despite the existence of effective pharmacological treatments, patient adherence to therapy is often poor [54], and may be due to adverse events (AEs) associated with treatment. Encouragingly, the safety and tolerability profiles of the approved LAMA/LABA combinations aclidinium/formoterol, umeclidinium/vilanterol, tiotropium/olodaterol, and indacaterol/glycopyrronium appear to be similar to those of the individual monotherapy components, with nasopharyngitis, headache, dry mouth, cough, and oropharyngeal pain reported as the most common AEs [55–58].
In summary, when compared with monotherapy treatments, LAMA/LABA treatments may have the potential to offer superior bronchodilation across patient subgroups, with reduced symptom burden and relief-medication use, and with no increase in drug-related AEs [31]. The risks and benefits of each treatment option should be considered when deciding on optimal disease management for individual patients.
The Right Treatment for the Right Patient
Individual patients with COPD may require different treatment approaches at different stages of their disease [5]. In order for the most appropriate treatment to be selected, patients should be assessed and treatment decisions made on a case-by-case basis; the GOLD report outlines strategies for the pharmacological management of COPD [5].
Those patients who are most suited to treatment with dual bronchodilator therapy need to be identified and decisions made on whether treatment should be escalated and which drugs to use. In the case of a patient newly diagnosed with COPD, it would be appropriate to prescribe either a LAMA or a LABA as monotherapy. Indeed, LAMA and LABA bronchodilator monotherapy currently provide the mainstay for treatment-naïve, moderately symptomatic patients with little/no exacerbation history; these therapies are effective at increasing FEV1, reducing symptoms, and increasing quality of life versus placebo, with no significant difference between the two treatment options [59–61]. Therefore, when choosing a LAMA or LABA therapy in newly diagnosed, treatment-naïve patients, the focus may be on patient preference (if any is expressed), with the option to switch to the alternative therapy should any AEs be experienced.
However, should a patient remain symptomatic following a LABA or LAMA, then a decision must be made between initiating treatment with a LAMA/LABA or a LABA/ICS dual therapy (or indeed a LAMA/LABA/ICS triple therapy). When deciding whether to treat with an ICS, it would be prudent to consider the potential for AEs that are well documented with this class of therapy [62], including pneumonia, increased fractures, diabetes, and other steroid-related effects [10]. Therefore, it may be pertinent to avoid steroid-related AEs by prescribing a LAMA/LABA dual therapy instead, if it had equivalent efficacy to treatment with LABA/ICS.
LAMA/LABA or LABA/ICS?
Several studies have compared dual therapy with LAMA/LABA to that of LABA/ICS, including AFFIRM (aclidinium/formoterol versus salmeterol/fluticasone in patients with stable COPD [63, 64]), ILLUMINATE (indacaterol/glycopyrronium versus salmeterol/fluticasone in patients with stable COPD [65]), LANTERN (indacaterol/glycopyrronium versus salmeterol/fluticasone in patients with moderate to severe stable COPD [66]), a study which compared umeclidinium/vilanterol with fluticasone/salmeterol in patients with stable COPD [67], a study which compared umeclidinium/vilanterol with salmeterol/fluticasone [68], and ENERGITO (tiotropium/olodaterol versus salmeterol/fluticasone in patients with moderate to severe COPD) [69]. These six studies have all demonstrated that lung function was significantly improved with LAMA/LABA treatment compared with LAMA/ICS treatment [63–69]. Additionally, ILLUMINATE reported a significant increase in TDI focal score with LAMA/LABA versus LABA/ICS [65], while the other studies have comparable TDI focal score improvements for both treatment groups, all of which were clinically meaningful [63, 64, 66, 68, 70]. These studies were not performed using inclusion criteria to specifically only include patients with COPD with an exacerbation history in the previous year; this gap in knowledge has been filled by the FLAME study, showing that LAMA/LABA had a greater impact in exacerbation prevention than ICS/LABA in this specific COPD subgroup [71]. With studies showing LAMA/LABA treatment at least as effective as LABA/ICS in treating COPD, one must consider the question: when is it appropriate to prescribe ICS or LABA/ICS to patients with COPD?
Different therapies may be more appropriate than others for individual patients, and treatments should be chosen carefully, based on a thorough assessment of each patient. Several COPD phenotypes have been identified and validated against clinical outcomes or response to treatment, including: (1) alpha-1 antitrypsin deficiency that may respond to augmentation therapy; (2) emphysema/hyperinflation that is responsive to lung volume reduction surgery; and (3) frequent exacerbators (≥2 per year) who respond to therapies reducing exacerbation frequency [72]. Additional COPD phenotypes have been proposed including, but not limited to, a rapid lung function decline phenotype, persistent inflammation phenotype, and a chronic bronchitis phenotype [72].
There is evidence to suggest that patients with an elevated blood eosinophil count may achieve particular benefit from ICS therapy in terms of reducing exacerbations; however, an appropriate eosinophil count threshold to identify such a patient subgroup has yet to be established [73]. Further investigations into patient grouping, identifying patients with COPD who will respond more favorably to certain treatments, and measurable biomarkers are ongoing. For example, a 12-week, randomized, open-label, parallel-group study (NCT02546349) of LABA/ICS versus LAMA stratified by high and low exhaled nitric oxide levels (≥23.5 vs. <23.5 ppb), which is a surrogate marker for eosinophilic airway inflammation, is underway and findings are keenly anticipated [74].
It has been proposed that LAMA/LABA dual bronchodilation is an appropriate intervention in patients with persistent breathlessness and exercise impairment that remain troublesome despite LAMA monotherapy [73]; however, no recommendations have been made regarding prioritising use of one specific LAMA/LABA therapy over another. No LAMA/LABA is currently approved in any particular subgroup of COPD patients and further research via adequately powered prospective head-to-head clinical trials would be needed before advocating a specific LAMA/LABA in a specific patient subgroup. At present, physicians should assess their patients to evaluate the individual burden imposed by COPD on each patient and consider the available LAMA/LABA evidence base before selecting an appropriate therapeutic intervention that will maximize the likelihood of achieving clinical benefit.
In conclusion, it is well documented that the symptoms of COPD are troublesome, variable, can occur during all parts of the 24-h day, and have a substantial impact on patients’ health status and quality of life. In order to provide effective, patient-orientated care, patients with COPD should be evaluated on the basis of lung function, the frequency of symptoms, and patient-perceived impact of symptoms on their lives. Many studies demonstrate that dual bronchodilator therapy has greater efficacy in improving lung function and symptom management versus monotherapy, but with equivalent safety profiles. New analysis of completed studies also suggests that differing therapies may be more appropriate than others for individual patients and that treatments should be selected carefully based on patient-by-patient assessment.
Notes
The E-RS™ is owned by Evidera. Permission to use this instrument may be obtained from Evidera (exactpro@evidera.com).
References
Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med. 2006;3:e442.
World Health Organization. Chronic obstructive pulmonary disease. Available at: http://www.who.int/respiratory/copd/en/. Accessed 18 Aug 2016.
Pauwels RA, Rabe KF. Burden and clinical features of chronic obstructive pulmonary disease (COPD). Lancet. 2004;364:613–20.
Chan-Yeung M, Ait-Khaled N, White N, Ip MS, Tan WC. The burden and impact of COPD in Asia and Africa. Int J Tuberc Lung Dis. 2004;8:2–14.
Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management and prevention of chronic obstructive pulmonary disease. Available at: http://goldcopd.org/global-strategy-diagnosis-management-prevention-copd-2016/. Accessed 18 Aug 2016.
Kessler R, Partridge MR, Miravitlles M, et al. Symptom variability in patients with severe COPD: a pan-European cross-sectional study. Eur Respir J. 2011;37:264–72.
Miravitlles M, Worth H, Soler Cataluna JJ, et al. Observational study to characterise 24-hour COPD symptoms and their relationship with patient-reported outcomes: results from the ASSESS study. Respir Res. 2014;15:122.
Partridge MR, Karlsson N, Small IR. Patient insight into the impact of chronic obstructive pulmonary disease in the morning: an internet survey. Curr Med Res Opin. 2009;25:2043–8.
Soler-Cataluna JJ, Sauleda J, Valdes L, et al. Prevalence and perception of 24-hour symptom patterns in patients with stable chronic obstructive pulmonary disease in Spain. Arch Bronconeumol. 2016;52:308–15.
Price D, Small M, Milligan G, Higgins V, Garcia Gil E, Estruch J. Impact of night-time symptoms in COPD: a real-world study in five European countries. Int J Chron Obstruct Pulmon Dis. 2013;8:595–603.
Kon SS, Canavan JL, Jones SE, et al. Minimum clinically important difference for the COPD Assessment Test: a prospective analysis. Lancet Respir Med. 2014;2:195–203.
Stephenson JS, Cai Q, Mocarski M, Tan H, Doshi JA, Sullivan SD. Impact and factors associated with nighttime and early morning symptoms among patients with chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2015;10:577–86.
Roche N, Small M, Broomfield S, Higgins V, Pollard R. Real world COPD: association of morning symptoms with clinical and patient reported outcomes. COPD. 2013;10:679–86.
Scharf SM, Maimon N, Simon-Tuval T, Bernhard-Scharf BJ, Reuveni H, Tarasiuk A. Sleep quality predicts quality of life in chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2011;6:1–12.
Singam P, Hong GE, Ho C, et al. Nocturia in patients with benign prostatic hyperplasia: evaluating the significance of ageing, co-morbid illnesses, lifestyle and medical therapy in treatment outcome in real life practice. Aging Male. 2015;18:112–7.
Redeker NS, Adams L, Berkowitz R, et al. Nocturia, sleep and daytime function in stable heart failure. J Card Fail. 2012;18:569–75.
Omachi TA, Blanc PD, Claman DM, et al. Disturbed sleep among COPD patients is longitudinally associated with mortality and adverse COPD outcomes. Sleep Med. 2012;13:476–83.
Lange P, Marott JL, Vestbo J, Nordestgaard BG. Prevalence of night-time dyspnoea in COPD and its implications for prognosis. Eur Respir J. 2014;43:1590–8.
Geiger-Brown J, Lindberg S, Krachman S, et al. Self-reported sleep quality and acute exacerbations of chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2015;10:389–97.
Nishimura K, Izumi T, Tsukino M, Oga T. Dyspnea is a better predictor of 5-year survival than airway obstruction in patients with COPD. Chest. 2002;121:1434–40.
Rennard S, Decramer M, Calverley PM, et al. Impact of COPD in North America and Europe in 2000: subjects’ perspective of Confronting COPD International Survey. Eur Respir J. 2002;20:799–805.
Miravitlles M, Ferrer J, Baro E, Lleonart M, Galera J. Differences between physician and patient in the perception of symptoms and their severity in COPD. Respir Med. 2013;107:1977–85.
Cazzola M, Tashkin DP. Combination of formoterol and tiotropium in the treatment of COPD: effects on lung function. COPD. 2009;6:404–15.
Cazzola M, Molimard M. The scientific rationale for combining long-acting beta2-agonists and muscarinic antagonists in COPD. Pulm Pharmacol Ther. 2010;23:257–67.
Reisner C, Orevillo C, Fernandez C, et al. Pooled analyses of five phase 2b studies support dose selection of glycopyrrolate-formoterol (GFF) MDI (PT003) 18/9.6 ++g for phase III development. Eur Respir J. 2014;42(Suppl 57):P4153.
Bateman ED, Ferguson GT, Barnes N, et al. Dual bronchodilation with QVA149 versus single bronchodilator therapy: the SHINE study. Eur Respir J. 2013;42:1484–94.
Buhl R, Maltais F, Abrahams R, et al. Tiotropium and olodaterol fixed-dose combination versus mono-components in COPD (GOLD 2-4). Eur Respir J. 2015;45:969–79.
D’Urzo AD, Rennard SI, Kerwin EM, Mergel V, Leselbaum AR, Caracta CF. Efficacy and safety of fixed-dose combinations of aclidinium bromide/formoterol fumarate: the 24-week, randomized, placebo-controlled AUGMENT COPD study. Respir Res. 2014;15:123–41.
Donohue JF, Maleki-Yazdi MR, Kilbride S, Mehta R, Kalberg C, Church A. Efficacy and safety of once-daily umeclidinium/vilanterol 62.5/25 mcg in COPD. Respir Med. 2013;107:1538–46.
Singh D, Ferguson GT, Bolitschek J, et al. Tiotropium + olodaterol shows clinically meaningful improvements in quality of life. Respir Med. 2015;109:1312–9.
Tashkin DP, Ferguson GT. Combination bronchodilator therapy in the management of chronic obstructive pulmonary disease. Respir Res. 2013;14:49.
Calzetta L, Rogliani P, Matera MG, Cazzola M. A systematic review with meta-analysis of dual bronchodilation with LAMA/LABA for the treatment of stable COPD. Chest. 2016;149:1181–96.
Singh D, Jones PW, Bateman ED, et al. Efficacy and safety of aclidinium bromide/formoterol fumarate fixed-dose combinations compared with individual components and placebo in patients with COPD (ACLIFORM-COPD): a multicentre, randomised study. BMC Pulm Med. 2014;14:178–89.
D’Urzo A, Singh D, Kerwin E, Lakkis H, Chuecos F, de Miquel G. Efficacy and safety of aclidinium bromide/formoterol fumarate fixed-dose combination in patients with moderate to severe COPD, stratified by COPD severity. Poster P553 presented at the American Thoracic Society, 2015.
Mróz R, Scanlon PD, Donohue JF, Molins E, Lakkis H, de Miquel G. Efficacy and safety of aclidinium bromide/formoterol fumarate fixed-dose combination in a pooled population of patients with COPD, stratified by age. Poster P550 presented at the American Thoracic Society, 2015.
Bateman E, Chapman K, Rennard S, Lakkis H, Moy ML, Garcia Gil E. Efficacy and safety of aclidinium bromide/formoterol fumarate fixed-dose combination in patients with moderate to severe COPD, stratified by inhaled corticosteroid use. Poster P552 presented at the American Thoracic Society, 2015.
Mahler DA, Weinberg DH, Wells CK, Feinstein AR. The measurement of dyspnea. Contents, interobserver agreement, and physiologic correlates of two new clinical indexes. Chest. 1984;85:751–8.
Mahler DA, Decramer M, D’Urzo A, et al. Dual bronchodilation with QVA149 reduces patient-reported dyspnoea in COPD: the BLAZE study. Eur Respir J. 2014;43:1599–609.
Singh D, Pujol H, Ribera A, et al. A dose-ranging study of the bronchodilator effects of abediterol (LAS100977), a long-acting beta2-adrenergic agonist, in asthma; a Phase II, randomized study. BMC Pulm Med. 2014;14:176.
Mahler DA, Waterman LA, Ward J, McCusker C, ZuWallack R, Baird JC. Validity and responsiveness of the self-administered computerized versions of the baseline and transition dyspnea indexes. Chest. 2007;132:1283–90.
Mahler DA, Ward J, Waterman LA, McCusker C, ZuWallack R, Baird JC. Patient-reported dyspnea in COPD reliability and association with stage of disease. Chest. 2009;136:1473–9.
Tashkin DP, Littner M, Andrews CP, Tomlinson L, Rinehart M, Denis-Mize K. Concomitant treatment with nebulized formoterol and tiotropium in subjects with COPD: a placebo-controlled trial. Respir Med. 2008;102:479–87.
Mahler DA, Ward J, Fierro-Carrion G, et al. Development of self-administered versions of modified baseline and transition dyspnea indexes in COPD. COPD. 2004;1:165–72.
Singh D. New combination bronchodilators for chronic obstructive pulmonary disease: current evidence and future perspectives. Br J Clin Pharmacol. 2015;79:695–708.
Wilcox TK, Chen WH, Howard KA, et al. Item selection, reliability and validity of the Shortness of Breath with Daily Activities (SOBDA) questionnaire: a new outcome measure for evaluating dyspnea in chronic obstructive pulmonary disease. Health Qual Life Outcomes. 2013;11:1–10.
Tabberer M, Brooks J, Wilcox T. A meta-analysis of four randomized clinical trials to confirm the reliability and responsiveness of the Shortness of Breath with Daily Activities (SOBDA) questionnaire in chronic obstructive pulmonary disease. Health Qual Life Outcomes. 2015;13:177.
Leidy NK, Sexton CC, Jones PW, et al. Measuring respiratory symptoms in clinical trials of COPD: reliability and validity of a daily diary. Thorax. 2014;69:443–9.
Leidy NK, Murray LT, Monz BU, et al. Measuring respiratory symptoms of COPD: performance of the EXACT-Respiratory Symptoms Tool (E-RS) in three clinical trials. Respir Res. 2014;15:124.
Jones PW, Harding G, Berry P, Wiklund I, Chen WH, Kline Leidy N. Development and first validation of the COPD Assessment Test. Eur Respir J. 2009;34:648–54.
Hareendran A, Palsgrove AC, Mocarski M, et al. The development of a patient-reported outcome measure for assessing nighttime symptoms of chronic obstructive pulmonary disease. Health Qual Life Outcomes. 2013;11:104.
Mocarski M, Zaiser E, Trundell D, Make BJ, Hareendran A. Evaluation of the psychometric properties of the Nighttime Symptoms of COPD Instrument. Int J Chron Obstruct Pulmon Dis. 2015;10:475–87.
Mocarski M, Hareendran A, Jen MH, Zaiser E, Make BJ. Evaluation of the psychometric properties of the Early Morning Symptoms of COPD Instrument (EMSCI). Value Health. 2014;17(3):A179.
Ringbaek T, Martinez G, Lange P. A comparison of the assessment of quality of life with CAT, CCQ, and SGRQ in COPD patients participating in pulmonary rehabilitation. COPD. 2012;9:12–5.
Makela MJ, Backer V, Hedegaard M, Larsson K. Adherence to inhaled therapies, health outcomes and costs in patients with asthma and COPD. Respir Med. 2013;107:1481–90.
AstraZeneca PLC. Duaklir® Genuair™ 340 µg/12 µg inhalation powder Summary of Product Characteristics. Available at: http://www.medicines.org.uk/emc/medicine/29652. Accessed 18 Aug 2016.
Boehringer Ingelheim Limited. Spiolto Respimat® Summary of Product Characteristics. Available at: https://www.medicines.org.uk/emc/medicine/30495. Accessed 18 Aug 2016.
GlaxoSmithKline. Anoro® Ellipta® Summary of Product Characteristics. Available at: https://www.medicines.org.uk/emc/medicine/28949/. Accessed 18 Aug 2016.
Novartis Pharmaceuticals Ltd. Ultibro® Breezhaler® Summary of Product Characteristics. Available at: http://www.medicines.org.uk/emc/medicine/29533. Accessed 18 Aug 2016.
Decramer ML, Chapman KR, Dahl R, et al. Once-daily indacaterol versus tiotropium for patients with severe chronic obstructive pulmonary disease (INVIGORATE): a randomised, blinded, parallel-group study. Lancet Respir Med. 2013;1:524–33.
Troosters T, Celli B, Lystig T, et al. Tiotropium as a first maintenance drug in COPD: secondary analysis of the UPLIFT trial. Eur Respir J. 2010;36:65–73.
Jones PW, Lamarca R, Chuecos F, et al. Characterisation and impact of reported and unreported exacerbations: results from ATTAIN. Eur Respir J. 2014;44:1156–65.
Price D, Yawn B, Brusselle G, Rossi A. Risk-to-benefit ratio of inhaled corticosteroids in patients with COPD. Prim Care Respir J. 2013;22(1):92–100.
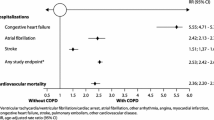
Beier J, Vogelmeier C, Mroz R, et al. Overall and cardiovascular safety of aclidinium/formoterol fixed-dose combination versus salmeterol/fluticasone in patients with COPD. Eur Respir J. 2015;46(Suppl 59).
Vogelmeier C, Paggiaro PL, Dorca J, et al. The Efficacy and Safety of Aclidinium/Formoterol Fixed-Dose Combination Compared with Salmeterol/Fluticasone in Patients with COPD: Results from a Phase III Study. In: C22. I FEEL FINE NOW: NEW TREATMENTS FOR COPD. Abstract presented at the ATS 2015 International Conference, Denver, Colorado, 15–20 May 2015.
Vogelmeier CF, Bateman ED, Pallante J, et al. Efficacy and safety of once-daily QVA149 compared with twice-daily salmeterol-fluticasone in patients with chronic obstructive pulmonary disease (ILLUMINATE): a randomised, double-blind, parallel group study. Lancet Respir Med. 2013;1:51–60.
Zhong N, Wang C, Zhou X, et al. LANTERN: a randomized study of QVA149 versus salmeterol/fluticasone combination in patients with COPD. Int J Chron Obstruct Pulmon Dis. 2015;10:1015–26.
Singh D, Worsley S, Zhu CQ, Hardaker L, Church A. Umeclidinium/vilanterol versus fluticasone propionate/salmeterol in COPD: a randomised trial. BMC Pulm Med. 2015;15:91.
Donohue JF, Worsley S, Zhu CQ, Hardaker L, Church A. Improvements in lung function with umeclidinium/vilanterol versus fluticasone propionate/salmeterol in patients with moderate-to-severe COPD and infrequent exacerbations. Respir Med. 2015;109:870–81.
Beeh KM, Derom E, Echave-Sustaeta J, et al. The lung function profile of once-daily tiotropium and olodaterol via Respimat® is superior to that of twice-daily salmeterol and fluticasone propionate via Accuhaler® (ENERGITO® study). Int J Chron Obstruct Pulmon Dis. 2016;11:193–205.
Mahler DA, Witek TJ Jr. The MCID of the transition dyspnea index is a total score of one unit. COPD. 2005;2:99–103.
Wedzicha JA, Banerji D, Chapman KR, et al. Indacaterol-Glycopyrronium versus Salmeterol-Fluticasone for COPD. N Engl J Med. 2016;374:2222–34.
Lange P, Halpin DM, O’Donnell DE, MacNee W. Diagnosis, assessment, and phenotyping of COPD: beyond FEV1. Int J Chron Obstruct Pulmon Dis. 2016;11(Spec Iss):3–12.
Calverley P, Vlies B. A rational approach to single, dual and triple therapy in COPD. Respirology. 2016;21:581–9.
Bethesda (MD): National Library of Medicine (US). Home—ClinicalTrials.gov. Available at: https://clinicaltrials.gov/ct2/home. Accessed 18 Aug 2016.
Price D, Small M, Sayers J. Characteristics of COPD patients experiencing night-time symptoms—results of a cross-sectional study in five European countries. Abstract presented at the 4th World Asthma and COPD forum, Paris, France, 30 April–3 May 2011.
O’Hagan P, Chavannes NH. The impact of morning symptoms on daily activities in chronic obstructive pulmonary disease. Curr Med Res Opin. 2014;30:301–14.
Acknowledgements
No funding or sponsorship was received for publication of this article. Medical writing assistance, funded by AstraZeneca, was provided by Nicole Jones and Siobhán Hoy on behalf of Complete Medical Communications. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval to the version to be published.
Disclosures
Dave Singh has received sponsorship to attend and speak at international meetings, honoraria for lecturing or attending advisory boards, and research grants from various pharmaceutical companies, including: Almirall, AstraZeneca, Boehringer Ingelheim, Chiesi, Genentech, GlaxoSmithKline, Glenmark, Johnson and Johnson, Merck, NAPP, Novartis, Pfizer, Skypharma, Takeda, Teva, Therevance, and Verona.
Marc Miravitlles has received speaker fees from Almirall, AstraZeneca, Boehringer Ingelheim, Gebro Pharma, Grifols, Menarini, Novartis, Pfizer, and Zambon, and consulting fees from Almirall, AstraZeneca, Boehringer Ingelheim, Chiesi, Cipla, GlaxoSmithKline, Grifols, Novartis, and Pfizer.
Claus Vogelmeier has given presentations at symposia and/or served on scientific advisory boards sponsored by Almirall, AstraZeneca, Boehringer Ingelheim, Chiesi, Cipla, GlaxoSmithKline, Grifols, Janssen, Mundipharma, Novartis, Omniamed, and Takeda. His institution has received unrestricted grants from GlaxoSmithKline and Grifols.
Compliance with Ethics Guidelines
This article is based on previously conducted studies, and does not involve any new studies of human or animal subjects performed by any of the authors.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced content
To view enhanced content for this article go to http://www.medengine.com/Redeem/1237F0604ED08BD4.
An erratum to this article is available at http://dx.doi.org/10.1007/s12325-017-0481-3.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Singh, D., Miravitlles, M. & Vogelmeier, C. Chronic Obstructive Pulmonary Disease Individualized Therapy: Tailored Approach to Symptom Management. Adv Ther 34, 281–299 (2017). https://doi.org/10.1007/s12325-016-0459-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-016-0459-6