Abstract
The progressive nature of type 2 diabetes (T2D) means that many patients will require basal insulin therapy at some point in the course of the disease due to β-cell failure. As basal insulin primarily targets fasting plasma glucose, patients may still experience considerable postprandial glucose excursions and therefore require an additional agent to achieve good glycemic control. Glucagon-like peptide-1 receptor agonists (GLP-1 RAs) provide an alternative to prandial insulin, with the benefits of fewer daily injections, and a lower risk of hypoglycemia and weight gain. Two fixed-ratio combinations (FRCs) of basal insulin and a GLP-1 RA are now available in the USA and the EU: insulin glargine + lixisenatide (iGlarLixi) and insulin degludec + liraglutide (IDegLira). Titratable FRCs are suitable for most patients with T2D and can help to simplify treatment regimens into one daily injection, potentially aiding in patient adherence. The complementary modes of action of the two components target seven of the many known pathophysiologic defects in T2D. FRCs have demonstrated enhanced glycemic control compared with their constituent components alone, comparable risk of hypoglycemia compared with basal insulin alone, and better tolerability compared with the GLP-1RA component alone due to the slower titration. In this article, we discuss the advantages of FRCs over multiple daily injections, present case studies of typical patients who could benefit from FRC therapy, and outline practical considerations for the initiation of FRC therapy in clinical practice.
Funding Sanofi.
Similar content being viewed by others
Introduction
Many patients with type 2 diabetes (T2D) will eventually require basal insuli, due to the progressive nature of the disease [1]. While lifestyle modification remains central in managing T2D, consideration of initiation of insulin therapy (possibly combined with other agents) is recommended in patients with T2D when they have glycated hemoglobin (A1C) levels ≥ 10%, and/or are symptomatic, and/or have blood glucose levels ≥ 300 mg/dL [1]. Furthermore, initiation of insulin therapy as part of dual therapy is a recommended option for patients with A1C > 9.0% [1, 2]. Real-world data have illustrated that the probability of patients achieving glycemic goals diminishes with time, with a substantial reduction if patients have not reached their A1C goals within 12 months of initiating basal insulin [3], underscoring the importance of early and timely intensification of therapy as needed. Early treatment with multiple drug combinations has been identified as key in prevention or slowing of β-cell failure, while also addressing other pathophysiologic abnormalities of T2D that have been shown to contribute to T2D progression [4].
Despite the improved pharmacodynamics of the newer basal insulin analogues, they are targeted and titrated to fasting plasma glucose (FPG) and, like other basal insulins, do not address postprandial glucose (PPG) excursions [5, 6]. Until recently, addition of one to three daily injections of prandial insulin was the most common option for targeting PPG excursions in patients with uncontrolled T2D [6]. The associated side effects of weight gain and increased hypoglycemia risk, as well as the increasing treatment complexity of multiple daily injections, contribute to potentially detrimental delays in advancement of therapy and can lead to years of unnecessary hyperglycemia for patients [6, 7]. The increased hypoglycemia risk arising from the use of prandial insulin may at least partly reflect the under-appreciated individual variation in rates of gastric emptying, which, if not taken into account, may lead to a mismatch in carbohydrate intake and insulin requirements [8]. The development of the first glucagon-like peptide 1 receptor agonist (GLP-1 RA) in 2005 provided an alternative option for control of PPG [9]. Recent trials have demonstrated that short-acting GLP-1 RAs (such as twice-daily exenatide or once-daily lixisenatide) when added to basal insulin are non-inferior to multi-dose prandial insulin glulisine for A1C reduction while achieving this with lower rates of hypoglycemia and less weight gain [1, 10,11,12]. The addition of a GLP-1 RA to basal insulin is currently recommended by the American Diabetes Association and the American Association of Clinical Endocrinologists/American College of Endocrinology guidelines as one of the treatment intensification options for patients with T2D uncontrolled on basal insulin [1, 13] as a result of these key trials.
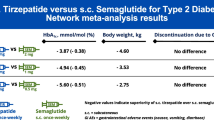
In addition to lifestyle modifications, including changes in diet and exercise, treatment guidelines generally recommend simplification of therapy to improve adherence [2, 14]. Titratable fixed-ratio combinations (FRCs) of basal insulin and a once-daily GLP-1 RA allow administration of both agents in a single daily injection, increasing convenience for the patient compared with the need for multiple injections per day. Two US Food and Drug Administration-approved, titratable FRCs are currently available: iGlarLixi, a combination of insulin glargine 100 units/mL and lixisenatide 33 µg/mL; and IDegLira, a combination of insulin degludec 100 units/mL and liraglutide 3.6 mg/mL. By combining the complementary antihyperglycemic effects of the component agents, these treatments improve glycemic control while minimizing the unwanted effects of each individual component—hypoglycemia and weight gain with basal insulin, and gastrointestinal (GI) effects with the GLP-1 RA. The reduced rate of GI effects is thought to be related to slower titration of the FRCs, which use the basal insulin dose to advance titration [15, 16]. Indirect comparisons suggest that IDegLira reduces A1C slightly more (< 0.5%) than iGlarLixi [17, 18], but this may reflect differences in the clinical trial designs or the relative effects of the two combinations on aspects of hyperglycemia. Additionally, when differences in baseline characteristics of included subjects were taken into account, the absolute difference in A1C change between the FRC and comparator arms was similar across the two trials. Although each FRC affects both FPG and PPG [19, 20], in general lixisenatide (the short-acting GLP-1 RA component in iGlarLixi) has a more pronounced effect on reduction of PPG excursions than liraglutide (the long-acting GLP-1 RA component in IDegLira), due to the more prominent effect of lixisenatide on slowing of gastric emptying, compared with liraglutide [21,22,23]. In contrast, greater effects on FPG and A1C have been observed with liraglutide than lixisenatide [24]. However, a similar efficacy was observed for a dose–response relationship in lixisenatide for once- and twice-daily regimens, with the once-daily dosing (at 20 μg) demonstrating the best efficacy-to-tolerability ratio [25]. The FRC iGlarLixi was designed as a once-daily product and twice-daily dosing has not been tested for this formulation.
In this article, we discuss the complementary modes of actions of the two components of FRCs, and their potential advantages over multi-injection treatments, with hypothetical case studies illustrating the type of patients who may gain the most from these therapies. This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Complementary Modes of Action of Combined Basal Insulin and GLP-1 RA Therapy
Many clinicians are still unaware of the potential benefits of combination therapies early in treatment [1, 13, 26, 27]. Titration of the basal insulin dose is often the only treatment-intensification option considered by clinicians, which can lead to “over-basalization”, increasing the risk of hypoglycemia and weight gain without gaining further benefits on glycemic control [28]. This can lead to postprandial glycemia remaining uncontrolled despite receiving high doses of basal insulin [6]. One advantage of combinations of two or more medications is that they can address multiple pathophysiologic defects through their different modes of action.
Together, basal insulin and GLP-1 RAs target seven of the many known pathophysiologic defects seen in T2D [4, 29]. Basal insulin aims to mimic the physiologic ongoing release of insulin, regulating FPG between meals and overnight [5]. This consistent background of insulin acts on fat cells and the liver, decreasing lipolysis in adipocytes, while inhibiting hepatic glucose production [29]. GLP-1 RAs have a complementary mode of action, acting primarily on the pancreas and liver, stimulating insulin secretion and suppressing glucagon secretion in a glucose-dependent manner [21, 29,30,31]. Secondly, they act on the brain and GI tract, enhancing satiety signals and slowing gastric emptying [21].
Advantages of Titratable FRCs of Basal Insulin and GLP-1 RAs
In clinical trials, FRCs have demonstrated enhanced glycemic control compared with their constituent components alone. For example, several studies report that, in both insulin-naïve and insulin-experienced patients with T2D not adequately controlled on their current treatment, iGlarLixi and IDegLira resulted in greater A1C reductions compared with the individual insulin and GLP-1 RA components, without an increase in risk of hypoglycemia; baseline A1C levels in these trials were ≥ 8.0% [15, 19, 32,33,34], and IDegLira was as effective as a basal-bolus regimen [35]. The benefits of FRCs versus comparators were evident regardless of patients’ baseline A1C or disease duration [36,37,38]. Key clinical outcomes in these trials are summarized in Table 1 [15, 19, 32, 33, 35, 39,40,41,42]. Overall, patients who received an FRC had greater improvement in A1C without an increase in hypoglycemia or weight gain compared with patients receiving optimized basal insulin, and lower rates of GI effects versus patients receiving a GLP-1 RA. In each of these trials, a greater percentage of patients in the iGlarLixi or IDegLira groups achieved a target A1C of < 7.0% compared with the basal insulin or GLP-1 RA groups. Additionally, the FRCs reduced glycemic fluctuations compared with their individual components, so patients spent more time within target range [43, 44].
Transient GI adverse events (AEs) including nausea, vomiting, and diarrhea are common in patients initiating GLP-1 RAs, and are often cited as the main reason for treatment discontinuation [45]. Clinical trial data indicate that rates of GI AEs are lower with FRCs than for individual GLP-1 RAs alone (Table 1) [11, 33]. In insulin-naïve patients, those receiving iGlarLixi had lower rates of GI AEs (21.7%) than did those receiving lixisenatide alone (36.9%) [19]; similar lower rates of GI AEs occurred with IDegLira than with liraglutide alone (Table 1) [33]. In insulin-naïve and insulin-experienced patients, GI AEs with FRCs were mostly mild to moderate, transient (occurring in the first 8–10 weeks of treatment), and led to few permanent treatment discontinuations (≤ 1.5% of patients discontinued FRC treatment due to GI AEs during the trials) [15, 19, 32, 33]. The lower rate of GI AEs may be in part due to the slower titration of the GLP-1 RA dose, compared with when administered alone [15, 16]. The effect of FRC use on cardiovascular outcomes has not been directly assessed. However, in randomized clinical trials of the GLP-1 RA components, use of lixisenatide and liraglutide did not increase the risk of major cardiovascular events, and liraglutide was associated with a reduction in risk compared with placebo [46, 47]. Further, insulin glargine [48] and insulin degludec [49] have both been shown to be cardiovascularly safe in their respective FDA-mandated CV outcome trials.
Compared with alternatives such as basal-bolus therapy or biphasic premixed insulins, titratable FRCs are associated with the need for less frequent blood glucose measurements using self-monitoring of blood glucose (SMBG) or continuous glucose monitoring due to their lower risk of hypoglycemia [50]. Additionally, compared with basal insulins alone, FRCs have demonstrated a weight-mitigating effect, resulting in weight neutrality or weight loss sustained through at least 1 year of treatment [15, 19, 32,33,34]. In the Lixilan trials, mean body weight decreased by 0.3–0.7 kg in iGlarLixi patients, compared with an increase of 0.7–1.1 kg in patients taking insulin glargine 100 U/mL alone [14, 19]. Similar findings were observed for IDegLira in the DUAL program, where studies directly comparing IDegLira with its components (DUAL I and II) showed a decrease in body weight of 0.5–2.7 kg, compared with a weight gain of 0–1.6 kg in patients on basal insulin alone (Table 1). These body weight changes were not a result of GI AEs. FRCs also have the practical advantages of being titrated only to the FPG, eliminating the need for multiple daily injections, and being administered using a pen device. This simplifies treatment, which may potentially aid in adherence [51,52,53], and can help reduce patients’ resistance to advancing treatment, which is often related to a fear of injections or the need for multiple daily injections [7]. However, FRCs are not suitable for all patients. For example, some patients may require a different ratio of basal insulin to GLP-1 RA, or doses of basal insulin that are not available in FRCs (see “Practical Considerations for FRC Therapy”). In these patients, separate injections of GLP-1 RA and basal insulin may be suitable instead, depending on the individual patient circumstances [52].
The potential for more effective A1C reduction without increased risk of hypoglycemia or weight gain when compared with basal insulin alone and fewer GI AEs compared with a GLP-1 RA alone makes FRCs a good option in people with T2D uncontrolled with their current therapy. In the following hypothetical case studies, we illustrate some of the types of patients who could benefit from treatment with FRCs.
Case Studies
Case Study 1
The patient is a 70-year-old female weighing 75 kg (165 lbs), with a body mass index (BMI) of 27 kg/m2, and a 12-year history of T2D. At diagnosis, her A1C was 9.4%, and she was started on metformin, with a personal A1C goal of < 7.0%. Despite being an older patient, a tight A1C goal was considered appropriate, based on her overall good health status and lack of known complications. She was also referred to a nutritionist and informed of appropriate ways to increase her physical activity level, such as participating in yoga classes or taking up running. Her best A1C on metformin was 8.3%, which was stable for several years. Approximately 4 years ago, her A1C had increased to 8.9%, and she was prescribed insulin glargine in addition to metformin. She achieved an A1C of 7.5%, which would not go down further. Analysis showed that her FPG levels (110 mg/dL) were within normal range, but she had large PPG excursions of up to 210 mg/dL. Her physician transitioned her treatment to insulin glargine (at bedtime) plus a once-daily GLP-1 RA (before breakfast), and her A1C levels are now stable at 7.0%, with PPG excursions below the recommended 180 mg/dL. The patient currently takes 40 units/day insulin and 20 µg of lixisenatide daily. She is generally accepting of this form of therapy but would like to simplify her treatment regimen.
-
This patient is a good candidate for use of an FRC to meet her goal of simplifying her treatment regimen. As she already takes insulin glargine and lixisenatide separately, converting her treatment to iGlarLixi would allow her to combine the two therapies into one daily injection using a familiar pen device. The doses of insulin and lixisenatide she is using are within the range supplied in the FRC pen (up to 60 units/day insulin glargine and 20 µg lixisenatide), and she is achieving her A1C goals with the combination of the two drugs.
-
To transition patients from insulin glargine to iGlarLixi, the patient’s current insulin dose is used to determine the initial dose of iGlarLixi; patients using 15 to < 30 units/day start iGlarLixi at 15 units/day and patients using 30–60 units/day start treatment at 30 units/day. Currently using 40 units/day of insulin, this patient would start the FRC at 30 units/day and then titrate upward or downward by 2–4 units (depending on the FPG) every week until she reaches the desired target range.
Case Study 2
The patient is a 55-year-old man weighing 95.5 kg (210 lbs), with a BMI of 30.1 kg/m2. He had a myocardial infarction at age 53 and was diagnosed with T2D 1 year ago, at which time his A1C level was 11.2%. He was prescribed insulin glargine plus metformin and given advice on the benefits of lifestyle changes in managing his T2D. At his most recent checkup, he complained about gaining weight, and his A1C level was still high at 8.4%, considerably above his individualized A1C goal of < 7.0%. Although this patient has cardiovascular disease, his individual A1C goal was set at < 7.0% given his relatively young age. He currently takes 50 units/day of insulin glargine, and although he has not experienced it, he is concerned about hypoglycemia because of its potential effects on his job as a delivery man. The patient was asked to record his SMBG results, which, upon review, revealed that his average FPG over 3 days was 191 mg/dL (with a range of 120–250 mg/dL) and that he had PPG values consistently exceeding 190 mg/dL after meals. As he works in a high-pressure job, he is very worried about managing a complex treatment schedule with multiple injections per day.
-
This patient has suboptimal glycemic control on basal insulin therapy alone. He is concerned about the number of injections that would be required with the addition of prandial insulin, as well as additional weight gain and increased hypoglycemia risk. Consistent with his SMBG glucose levels, his A1C levels are still markedly elevated, suggesting that he may require additional therapy.
-
At this point, a recommended option in treatment guidelines is the addition of a GLP-1 RA to improve glycemic control with lower risk of hypoglycemia or weight gain rather than the addition of bolus insulin. Using the once-daily FRC may address his concerns about additional injections, as well as allay concerns about hypoglycemia and weight gain, while helping him to achieve better glycemic control. In clinical trials, IDegLira provided significant reductions in FPG (62 mg/dL at 26 weeks) in patients already on basal insulin [30]. FPG reductions with iGlarLixi were smaller (7.2 mg/dL at 30 weeks) [15].
-
The maximum dose of insulin degludec possible with IDegLira is 50 units/day, and this patient may require a lower dose with combined treatment. To switch a patient from degludec 100 units/mL or another basal insulin to IDegLira, an initial daily dose of 16 units is used, and titrated upward or downward (based on FPG) every 3–4 days until FPG is within target.
-
Cardiovascular disease is a major contributor to morbidity and excess mortality in patients with T2D, making treatment effects on cardiovascular health an important consideration. The components of current FRCs have been shown to reduce (liraglutide) or have a neutral effect (lixisenatide) on cardiovascular risk in patients with T2D [46,47,48,49]. Given his established history of atherosclerotic cardiovascular disease, one may consider liraglutide as the chosen GLP-1 RA as it has a specific indication for reducing CV risk; however, IDegLira does not carry this specific indication.
Case Study 3
The patient is a 65-year-old man weighing 100.4 kg (221.3 lbs; BMI: 28.2 kg/m2). He was diagnosed with T2D 7 years ago, with an A1C of 8.2% at diagnosis. He was advised to introduce low-impact exercise into his weekly schedule and to review his diet with a nutritionist. He was initially treated with metformin and attained an A1C of 7.4% on 1200 mg/day, but could not tolerate a higher dose of metformin due to GI AEs. At that point, a dipeptidyl peptidase-4 (DPP-4) inhibitor was added to his treatment, and he attained his individualized A1C target of 7.0%. This target was considered suitable for this patient as he does not have any complications from his diabetes. Two years ago, his A1C reached 7.8%, and he admitted that he forgot to take one or more of his pills several times a week. At that point, his clinician added insulin glargine. His current regimen is insulin glargine 40 units/day, metformin, and a DPP-4 inhibitor (not as combined presentation), but his A1C remains elevated at 7.4%. SMBG reveals that his FPG is well controlled (107 mg/dL), but his PPG frequently reaches 250 mg/dL after midday meals. He complains about the number of pills he takes and does not want more injections to further complicate his treatment.
-
This patient currently needs to manage a complicated combination of medications for his diabetes, which has impacted his treatment adherence and led to poor glycemic control despite multiple effective medications. Almost all older adults have comorbid conditions, such as hypertension and dyslipidemia, and more than half are estimated to combine multiple oral treatments for these conditions, adding to their daily pill count and/or confusion [54, 55]. Polypharmacy due to multimorbidity should be a consideration in establishing or advancing a diabetes treatment regimen [1].
-
The patient would likely benefit from transitioning to an FRC, which would combine basal insulin (which he is already injecting once a day) and a GLP-1 RA. Because DPP-4 inhibitors and GLP-1 RAs both target the incretin response, he would discontinue the DPP-4 inhibitor, which would simplify his oral treatment regimen without sacrificing glycemic control. Using iGlarLixi would more effectively target his PPG excursions and improve glycemic control without incurring weight gain or an increased risk of hypoglycemia.
Case Study 4
The patient is a 55-year-old woman who weighs 71.2 kg (157 lbs) with a BMI of 23.2 kg/m2. She has a 4-year history of T2D. At diagnosis, her A1C was 10.1%, and she was started on metformin and insulin degludec and advised to stop smoking. Since starting on basal insulin, she has gained 2.5 kg (5.5 lbs), but was able to reduce her A1C to 6.9% (personalized A1C target: < 7.0%, based on the patient being active without co-existing complications) on 45 units/day of insulin degludec and 1500 mg/day of metformin. However, she experienced symptoms of hypoglycemia at night on several occasions (on one occasion, SMBG was 68 mg/dL) and decided to reduce her insulin dose on her own accord. At her most recent visit, her A1C level remained above target at 7.5%, and she admitted to taking less insulin—30 units/day instead of the initially prescribed 45 units/day. Therefore, her physician recommended that she intensify her treatment. The patient, a dancer, is concerned that this intensification of her treatment will lead to further weight gain and increased risk of hypoglycemia, which may compromise her career. Her physician recommended switching to an FRC of basal insulin combined with a GLP-1 RA, telling her that the addition of the GLP-1 RA will improve her glycemic control, but informed her about the potential for GLP-1 RAs to cause GI AEs. The patient is now concerned about whether she will still be able to perform if these side effects are severe or long-lasting.
-
This patient is a candidate for a titratable FRC, because she could benefit from the additional glycemic control and the simple, once-daily administration. Using an FRC would address her concerns regarding weight gain and a possible increased risk of hypoglycemia. In clinical trials, a higher percentage of patients achieved glycemic goals without experiencing hypoglycemia or weight gain with FRCs versus optimized basal insulin or a GLP-1 RA alone [15, 19, 32, 33] or versus a basal-bolus regimen [35].
-
FRCs have additionally demonstrated reduced risk for GI AEs compared with their component GLP-1 RA, while maintaining similar or improved levels of glycemic control [16], and are therefore particularly suitable for patients like this woman who are concerned about side effects.
Practical Considerations for FRC Therapy
Clinicians often delay treatment intensification when patients do not achieve glycemic targets, despite the demonstrated benefits of achieving glycemic control in the early stages or the decreasing likelihood of achieving glycemic control on inadequate therapy as time goes by [3, 4, 7, 56]. Post hoc analyses of the LixiLan-L trial indicated that, irrespective of the initial A1C levels, titratable FRCs can be an effective treatment option for achieving treatment goals more quickly, and for controlling A1C levels without increasing the risk of hypoglycemia [37, 57].
Although the components and available doses of titratable FRCs of basal insulin and GLP-1 RAs may not be suitable for all patients, FRCs are considered to be appropriate for approximately 80% of patients with T2D [58]. Patients making the transition from insulin glargine or insulin degludec to iGlarLixi or IDegLira can continue to use a similar, familiar pen. However, because the FRC pens have a maximum daily insulin dose of 60 units for iGlarLixi and 50 units for IDegLira, they are not suitable for patients requiring higher daily basal insulin doses (e.g., patients with severe insulin resistance). Additionally, since IDegLira is contraindicated in patients with a personal or family history of medullary thyroid carcinoma and neither FRC has been studied in patients with a history of pancreatitis, alternative therapies are advised. Each FRC is approved for use in patients with T2D uncontrolled on basal insulin or a GLP-1 RA, and existing basal insulin or GLP-1 RA treatment must be discontinued before transitioning to an FRC [59, 60]. Because the ratio of GLP-1 RA to basal insulin is fixed to the insulin dose, an FRC may not be suitable for patients who require a different GLP-1 RA to basal insulin ratio.
Conclusions
Overall, titratable FRCs are considered to have a better safety profile, with a lower risk of hypoglycemia and weight gain (with excellent likelihood of weight loss), when compared with basal insulin alone. FRCs are also consistently associated with reduced frequency of GI AEs when compared with the GLP-1 RA component alone, which is largely attributable to the slower rate of up-titration of dosage. FRCs provide effective glycemic control, with greater A1C reductions than typically observed when basal insulin or GLP-1 RAs are used alone, and reduced PPG excursions. While not suitable for all patients, FRCs provide an effective, safe, convenient, single daily-dose option for many patients with T2D, thereby simplifying the treatment regimen, and thus potentially improving long-term adherence to therapy.
References
American Diabetes Association (ADA). Standards of Medical Care in Diabetes—2018. Diabetes Care. 2018;41(Suppl 1):S1–159.
Garber AJ, Abrahamson MJ, Barzilay JI, et al. Consensus statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the comprehensive type 2 diabetes management algorithm—2018 executive summary. Endocr Pract. 2018;24:91–120.
Blonde L, Meneghini L, Peng XV, et al. Probability of achieving glycemic control with basal insulin in patients with type 2 diabetes in real-world practice in the USA. Diabetes Ther. 2018;9:1347–58.
DeFronzo RA. Banting Lecture. From the triumvirate to the ominous octet: a new paradigm for the treatment of type 2 diabetes. Diabetes. 2009;58:773–95.
Arnolds S, Kuglin B, Kapitza C, Heise T. How pharmacokinetic and pharmacodynamic principles pave the way for optimal basal insulin therapy in type 2 diabetes. Int J Clin Pract. 2010;64:1415–24.
Johnson EL, Frias JP, Trujillo JM. Anticipatory guidance in type 2 diabetes to improve disease management; next steps after basal insulin. Postgrad Med. 2018;130:365–74.
Khunti K, Millar-Jones D. Clinical inertia to insulin initiation and intensification in the UK: a focused literature review. Primary Care Diabetes. 2017;11:3–12.
Marathe CS, Rayner CK, Jones KL, Horowitz M. Relationships between gastric emptying, postprandial glycemia, and incretin hormones. Diabetes Care. 2013;36(5):1396–405.
Prasad-Reddy L, Isaacs D. A clinical review of GLP-1 receptor agonists: efficacy and safety in diabetes and beyond. Drugs Context. 2015;4:212283.
Diamant M, Nauck MA, Shaginian R, et al. Glucagon-like peptide 1 receptor agonist or bolus insulin with optimized basal insulin in type 2 diabetes. Diabetes Care. 2014;37:2763–73.
Rosenstock J, Fonseca VA, Gross JL, et al. Advancing basal insulin replacement in type 2 diabetes inadequately controlled with insulin glargine plus oral agents: a comparison of adding albiglutide, a weekly GLP-1 receptor agonist, versus thrice-daily prandial insulin lispro. Diabetes Care. 2014;37:2317–25.
Porcellati F, Lucidi P, Bolli GB, Fanelli CG. GLP-1 RAs as compared to prandial insulin after failure of basal insulin in type 2 diabetes: lessons from the 4B and Get-Goal DUO 2 trials. Diabetes Metab. 2015;41(6 Suppl 1):6S16–20.
AACE/ACE comprehensive type 2 diabetes management algorithm 2018; 2018. https://www.aace.com/publications/algorithm. Accessed 22 October 2018.
Handelsman Y, Bloomgarden ZT, Grunberger G, et al. American Association of Clinical Endocrinologists and American College of Endocrinology—clinical practice guidelines for developing a diabetes mellitus comprehensive care plan—2015. Endocr Pract. 2015;21(Suppl 1):1–87.
Aroda VR, Rosenstock J, Wysham C, et al. Efficacy and safety of LixiLan, a titratable fixed-ratio combination of insulin glargine plus lixisenatide in type 2 diabetes inadequately controlled on basal insulin and metformin: the LixiLan-L randomized trial. Diabetes Care. 2016;39:1972–80.
Trujillo JM, Roberts M, Dex T, Chao J, White J, LaSalle J. Low incidence of gastrointestinal adverse events over time with a fixed-ratio combination of insulin glargine and lixisenatide vs lixisenatide alone. Diabetes Obes Metab. 2018;20:2690–4.
Cai X, Gao X, Yang W, Ji L. Comparison between insulin degludec/liraglutide treatment and insulin glargine/lixisenatide treatment in type 2 diabetes: a systematic review and meta-analysis. Expert Opin Pharmacother. 2017;18:1789–98.
Evans M, Billings LK, Håkan-Bloch S, et al. An indirect treatment comparison of the efficacy of insulin degludec/liraglutide (IDegLira) and insulin glargine/lixisenatide (iGlarLixi) in patients with type 2 diabetes uncontrolled on basal insulin. J Med Econ. 2018;21:340–7.
Rosenstock J, Aronson R, Grunberger G, et al. Benefits of LixiLan, a titratable fixed-ratio combination of insulin glargine plus lixisenatide, versus insulin glargine and lixisenatide monocomponents in type 2 diabetes inadequately controlled on oral agents: the LixiLan-O randomized trial. Diabetes Care. 2016;39:2026–35.
Holst JJ, Buse JB, Rodbard HW, et al. IDegLira improves both fasting and postprandial glucose control as demonstrated using continuous glucose monitoring and a standardized meal test. J Diabetes Sci Technol. 2015;10:389–97.
Meier JJ. GLP-1 receptor agonists for individualized treatment of type 2 diabetes mellitus. Nat Rev Endocrinol. 2012;8:728–42.
Meier JJ, Rosenstock J, Hincelin-Méry A, et al. Contrasting effects of lixisenatide and liraglutide on postprandial glycemic control, gastric emptying, and safety parameters in patients with type 2 diabetes on optimized insulin glargine with or without metformin: a randomized, open-label trial. Diabetes Care. 2015;38:1263–73.
Nauck M, Rizzo M, Johnson A, Bosch-Traberg H, Madsen J, Cariou B. Once-daily liraglutide versus lixisenatide as add-on to metformin in type 2 diabetes: a 26-week randomized controlled clinical trial. Diabetes Care. 2016;39:1501–9.
Kapitza C, Forst T, Coester HV, Poitiers F, Ruus P, Hincelin-Méry A. Pharmacodynamic characteristics of lixisenatide once daily versus liraglutide once daily in patients with type 2 diabetes insufficiently controlled on metformin. Diabetes Obes Metab. 2013;15(7):642–9.
Ratner RE, Rosenstock J, Boka G; DRI6012 Study Investigators. Dose-dependent effects of the once-daily GLP-1 receptor agonist lixisenatide in patients with Type 2 diabetes inadequately controlled with metformin: a randomized, double-blind, placebo-controlled trial. Diabet Med. 2010;27(9):1024-32.
Abdul-Ghani MA, Puckett C, Triplitt C, et al. Initial combination therapy with metformin, pioglitazone and exenatide is more effective than sequential add-on therapy in subjects with new-onset diabetes. Results from the Efficacy and Durability of Initial Combination Therapy for Type 2 Diabetes (EDICT): a randomized trial. Diabetes Obes Metab. 2015;17:268–75.
Strain WD, Cos X, Hirst M, et al. Time to do more: addressing clinical inertia in the management of type 2 diabetes mellitus. Diabetes Res Clin Pract. 2014;105:302–12.
Reid T, Gao L, Gill J, et al. How much is too much? Outcomes in patients using high-dose insulin glargine. Int J Clin Pract. 2016;70:56–65.
Valentine V, Goldman J, Shubrook JH. Rationale for, initiation and titration of the basal insulin/GLP-1 RA fixed-ratio combination production IDegLira and iGlarLixi, for the management of type 2 diabetes. Diabetes Ther. 2017;8:739–52.
Kalra S, Baruah MP, Sahay RK, Unnikrishnan AG, Uppal S, Adetunji O. Glucagon-like peptide-1 receptor agonists in the treatment of type 2 diabetes: past, present, and future. Indian J Endocrinol Metab. 2016;20:254–67.
Nauck MA, Vilsbøll T, Gallwitz B, Garber A, Madsbad S. Incretin-based therapies: viewpoints on the way to consensus. Diabetes Care. 2009;32(Suppl 2):S223–31.
Buse JB, Vilsbøll T, Thurman J, et al. Contribution of liraglutide in the fixed-ratio combination of insulin degludec and liraglutide (IDegLira). Diabetes Care. 2014;37:2926–33.
Gough SC, Bode B, Woo V, et al. Efficacy and safety of a fixed-ratio combination of insulin degludec and liraglutide (IDegLira) compared with its components given alone: results of a phase 3, open-label, randomised, 26-week, treat-to-target trial in insulin-naive patients with type 2 diabetes. Lancet Diabetes Endocrinol. 2014;2:885–93.
Gough SC, Bode BW, Woo VC, et al. One-year efficacy and safety of a fixed combination of insulin degludec and liraglutide in patients with type 2 diabetes: results of a 26-week extension to a 26-week main trial. Diabetes Obes Metab. 2015;17:965–73.
Billings LK, Doshi A, Gouet D, et al. Efficacy and safety of IDegLira versus basal-bolus insulin therapy in patients with type 2 diabetes uncontrolled on metformin and basal insulin: the DUAL VII randomized clinical trial. Diabetes Care. 2018;41:1009–16.
Davies MJ, Leiter LA, Guerci B, et al. Impact of baseline glycated haemoglobin, diabetes duration, and body mass index on clinical outcomes in the LixiLan-O trial testing a titratable fixed-ratio combination of insulin glargine/lixisenatide (iGlarLixi) vs insulin glargine and lixisenatide monocomponents. Diabetes Obes Metab. 2017;19:1798–804.
Niemoeller E, Souhami E, Wu Y, Jensen KH. iGlarLixi reduces glycated hemoglobin to a greater extent than basal insulin regardless of levels at screening: post hoc analysis of LixiLan-L. Diabetes Ther. 2018;9:373–82.
Rodbard HW, Buse JB, Woo V, et al. Benefits of combination insulin degludec and liraglutide are independent of baseline glycated haemoglobin level and duration of type 2 diabetes. Diabetes Obes Metab. 2016;18:40–8.
Linjawi S, Bode BW, Chaykin LB, Courrèges JP, Handelsman Y, Lehmann LM, Mishra A, Simpson RW. The Efficacy of IDegLira (Insulin Degludec/Liraglutide Combination) in Adults with Type 2 Diabetes Inadequately Controlled with a GLP-1 Receptor Agonist and Oral Therapy: DUAL III Randomized Clinical Trial. Diabetes Ther. 2017;8(1):101–14.
Rodbard HW, Bode BW, Harris SB, Rose L, Lehmann L, Jarlov H, Thurman J; Dual Action of Liraglutide and insulin degludec (DUAL) IV trial investigators. Safety and efficacy of insulin degludec/liraglutide (IDegLira) added to sulphonylurea alone or to sulphonylurea and metformin in insulin-naïve people with Type 2 diabetes: the DUAL IV trial. Diabet Med. 2017;34(2):189-196.
Lingvay I, Harris S, Jaeckel E, Chandarana K, Ranthe MF, Jódar E. Insulin degludec/liraglutide (IDegLira) was effective across a range of dysglycaemia and body mass index categories in the DUAL V randomized trial. Diabetes Obes Metab. 2018;20(1):200–5.
Harris SB, Kocsis G, Prager R, Ridge T, Chandarana K, Halladin N, Jabbour S. Safety and efficacy of IDegLira titrated once weekly versus twice weekly in patients with type 2 diabetes uncontrolled on oral antidiabetic drugs: DUAL VI randomized clinical trial. Diabetes Obes Metab. 2017;19(6):858–65.
Aronson R, Umpierrez G, Stager W, Kovatchev B. Insulin glargine/lixisenatide fixed ratio combination improves glycemic variability in type 2 diabetes. Can J Diabetes. 2016;40:S45–6.
King AB, Philis-Tsimikas A, Kilpatrick ES, Langbakke IH, Begtrup K, Vilsbøll T. A fixed ratio combination of insulin degludec and liraglutide (IDegLira) reduces glycemic fluctuation and brings more patients with type 2 diabetes within blood glucose target ranges. Diabetes Technol Ther. 2017;19:255–64.
Sikirica MV, Martin AA, Wood R, Leith A, Piercy J, Higgins V. Reasons for discontinuation of GLP-1 receptor antagonists: data from a large cross-sectional survey of physicians and type 2 diabetic patients. Diabetes Metab Syndr Obes. 2017;10:403–12.
Pfeffer MA, Claggett B, Diaz R, et al. Lixisenatide in patients with type 2 diabetes and acute coronary syndrome. N Engl J Med. 2015;373:2247–57.
Marso SP, Daniels GH, Brown-Frandsen K, et al. Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2016;375:311–22.
ORIGIN Trial Investigators, Gerstein HC, Bosch J, et al. Basal insulin and cardiovascular and other outcomes in dysglycemia. N Engl J Med. 2012;367:319–28.
Marso SP, McGuire DK, Zinman B, et al. Efficacy and safety of degludec versus glargine in type 2 diabetes. N Engl J Med. 2017;377:723–32.
Anderson SL, Trujillo JM. Basal insulin use with GLP-1 receptor agonists. Diabetes Spectr. 2016;29:152–60.
Jenkins N, Hallowell N, Farmer AJ, Holman RR, Lawton J. Participants’ experiences of intensifying insulin therapy during the Treating to Target in Type 2 Diabetes (4-T) trial: qualitative interview study. Diabet Med. 2011;28:543–8.
Peyrot M, Rubin RR, Kruger DF, Travis LB. Correlates of insulin injection omission. Diabetes Care. 2010;33:240–5.
Peyrot M, Barnett AH, Meneghini LF, Schumm-Draeger PM. Factors associated with injection omission/non-adherence in the Global Attitudes of Patients and Physicians in Insulin Therapy study. Diabetes Obes Metab. 2012;14:1081–7.
Noale M, Veronese N, Cavallo Perin P, et al. Polypharmacy in elderly patients with type 2 diabetes using oral antidiabetic treatment. Acta Diabetol. 2016;53:323–30.
Iglay K, Hannachi H, Joseph Howie P, et al. Prevalence and co-prevalence of comorbidities among patients with type 2 diabetes mellitus. Curr Med Res Opin. 2016;32:1243–52.
Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359:1577–89.
Frias J, Puig Domingo M, Meneghini L, et al. More patients reach glycaemic control with a fixed-ratio combination of insulin glargine and lixisenatide (iGlarLixi) than with basal insulin at 12 weeks of treatment: a post hoc time-to-control analysis of LixiLan-O and LixiLan-L. Diabetes Obes Metab. 2018;20:2314–8.
Blumer I, Pettus JH, Santos Caviaola T. Fixed-ratio combination therapy for type 2 diabetes: the top ten things you should know about insulin and glucagon-like peptide-1 receptor agonist combinations. Postgrad Med. 2018;130(4):375–80.
Xultophy prescribing information; 2016. https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/208583s000lbl.pdf. Accessed 22 October 2018.
Soliqua 100/33 prescribing information; 2016. https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/208673s000lbl.pdf. Accessed 22 October 2018.
Acknowledgements
Funding
Development of the manuscript, Open Access fees and article processing charges were funded by Sanofi US, Inc. All authors had full access to all of the data in this study and take complete responsibility for the integrity of the data and accuracy of the data analysis.
Medical writing, Editorial, and Other Assistance
The authors received writing/editorial support in the preparation of this manuscript provided by Martina Fuchsberger, PhD, of Excerpta Medica, funded by Sanofi US, Inc.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Leigh Perreault has received personal fees for consulting and/or speaking from Astra Zeneca, Boheringer-Ingelheim, Janssen, Medscape, Merck, Novo Nordisk, Sanofi, UpToDate, and WebMD. Helena Rodbard has served as a principal investigator, consultant, speaker, and advisor to AstraZeneca, Boehringer Ingelheim, Eli Lilly, Janssen, Lexicon, Merck, Novo Nordisk, and Sanofi. Virginia Valentine is on advisory boards for Abbott Diabetes Care, AstraZeneca, Cequr, Eli Lilly, Intarcia, Janssen, and Novo Nordisk; a consultant for Abbott Diabetes Care, Adocia, Cequr, and Eli Lilly; and a speaker for Abbott Diabetes Care, AstraZeneca, Eli Lilly, Janssen, and Pamlab. Eric Johnson serves or has recently served at speaker’s bureaux for Medtronic and Novo Nordisk; and serves or has served on advisory panels for Novo Nordisk and Sanofi.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced digital features
To view enhanced digital features for this article go to https://doi.org/10.6084/m9.figshare.7491221.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Perreault, L., Rodbard, H., Valentine, V. et al. Optimizing Fixed-Ratio Combination Therapy in Type 2 Diabetes. Adv Ther 36, 265–277 (2019). https://doi.org/10.1007/s12325-018-0868-9
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-018-0868-9