Abstract
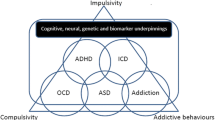
Obsessive compulsive disorder (OCD) and attention deficit hyperactivity disorder (ADHD) are two of the most common neuropsychiatric diseases in paediatric populations. The high comorbidity of ADHD and OCD with each other, especially of ADHD in paediatric OCD, is well described. OCD and ADHD often follow a chronic course with persistent rates of at least 40–50 %. Family studies showed high heritability in ADHD and OCD, and some genetic findings showed similar variants for both disorders of the same pathogenetic mechanisms, whereas other genetic findings may differentiate between ADHD and OCD. Neuropsychological and neuroimaging studies suggest that partly similar executive functions are affected in both disorders. The deficits in the corresponding brain networks may be responsible for the perseverative, compulsive symptoms in OCD but also for the disinhibited and impulsive symptoms characterizing ADHD. This article reviews the current literature of neuroimaging, neurochemical circuitry, neuropsychological and genetic findings considering similarities as well as differences between OCD and ADHD.
Similar content being viewed by others
Introduction
Obsessive compulsive disorders (OCD) are typically characterized by the presence of recurrent, intrusive, and disturbing thoughts (obsessions) which often elicit anxiety or emotional stress followed by repetitive stereotypic behaviour or thoughts (compulsions) in order to neutralize the negative affects (American Psychiatric Association 1994). According to ICD-10 diagnostic classification, OCD consists of recurrent and persistent thoughts, behavioural patterns, ideas, and impulses that impose themselves against internal resistance, experienced by the patient as excessive and distressing. According to ICD-10 (World Health Organization 1996), OCD can be divided into “predominantly obsessional thoughts”, “predominantly compulsive acts”, or in a subtype of combination of both “obsessions and compulsions”. Fear of contamination, sexual, hypochondriac, and excessive thoughts including scruples/guilt are the most commonly reported obsessions and washing, repeating, checking, and ordering are the most commonly reported compulsions (Geller et al. 2001). In the DSM-5 (American Psychiatric Association 2013), OCD is newly classified into the diagnostic categories: “obsessive compulsive and related disorders” including “obsessive compulsive disorder”, and as related disorders e.g.“body dysmorphic disorder”, “hoarding disorder”, “hair pulling disorder” (trichotillomania). In the previous DSM-IV, OCD was classified as a subcategory of anxiety disorders. Therefore, in DSM-5, the specificity of the symptomatology including obsessions and compulsions with or without concomitant anxiety comes more to the centre of attention.
In DSM-IV, the diagnostic criteria for children with OCD differs from adults with OCD in regard to not having always insight into the senselessness of the obsessive behaviour. For adults, “showing insight into the senselessness of the symptoms” was one of the key criteria to differentiate OCD from psychosis; see also ICD-10. In DSM-5, clinicians even have to specify the degree of insight into the symptomatology: good/fair, poor, or absent insight. The presence of insight is of clinical importance because insight not only correlates with age but also with severity and positive therapy response (Walitza 2014). Clinicians also have to specify whether the patient has a current or past history of a tic disorder, this will be classified as a tic-related obsessive compulsive disorder (American Psychiatric Association 2013; Thomsen 2013; Walitza 2014). In the overview presented here, nearly all studies have used ICD-10 or DSM-IV for the classification of OCD in children and adults. Therefore, we want to anticipate that questions of confounding variables of the degree of insight and of the influence of previous or present tic disorders could not be answered by most of the previous findings and should be addressed using the DSM-5 criteria in future studies.
From an epidemiological point of view, OCD is the world’s fourth most common psychiatric disorder with a lifetime prevalence of 2–3 % (Flament et al. 1988; Robins et al. 1984; Zohar 1999). Delorme et al. (2005) considered the disorder to have a bimodal age distribution, with a first peak at age 11 and a second in early adulthood. Up to 50 % of all OCD cases emerge during childhood or adolescence (Flament et al. 1988; Nestadt et al. 2000). The course and outcome show high persistence rates with at least 40 % in retrospective and prospective follow-up studies in OCD (Stewart et al. 2004; Zellmann et al. 2009) whereby patients in remission with OCD often developed other psychiatric disorders and other psychiatric symptoms, exacerbated by the decrease of OCD symptoms (Stewart et al. 2004).
Attention deficit hyperactivity disorder (ADHD) is characterized by a persistent pattern of inattention and/or hyperactivity and impulsivity (American Psychiatric Association 1994). The symptomatology of ADHD interferes with functioning or development and has persisted (for at least 6 months) to a degree that is inconsistent with expected developmental level and that negatively impacts directly on social and academic/occupational activities. Manifestations of the disorder must be present in more than one setting (e.g. school, home, with friends or relatives). The symptoms vary depending on context, the higher the structure of the context (e.g. school), the higher seems to be the deviation from the average of normal behaviours. But it has to be taken into account that some forms of structure of school and homework can also help the child to focus more on important topics. According to DSM-5 criteria, ADHD is now classified as a neurodevelopmental disorder, which is a group of conditions with onset in the developmental period. These disorders (also including autism spectrum disorders and learning disorders) typically manifest in early development, often before the child enters grade school, and are characterized by developmental deficits that produce impairments of a broad range of social functioning (American Psychiatric Association 2013). Several inattentive or hyperactive–impulsive symptoms must have been present prior to age of 12 years (previously in DSM-IV, the symptomatology has to be present before age of 7 years). Therefore, we can assume that ADHD has on average an earlier onset of symptoms in comparison with OCD. DSM-5 distinguishes three different presentations: a predominantly inattentive presentation, a predominantly hyperactive/impulsive, and a combined presentation, if criteria for both inattention and hyperactivity–impulsivity are met. Although the lists of 18 symptoms from the DSM-5 (American Psychiatric Association 2013) and the ICD-10 (World Health Organization 1996) for ADHD are similar, ICD-10 is more specific as some symptoms must be present in all of the three dimensions (inattention, hyperactivity, and impulsivity). And hyperkinetic disorder (the nomenclature used in the ICD-10 that corresponds to ADHD in the DSM-5) is excluded if depression and/or anxiety disorders are also identified. In DSM-5, autism spectrum disorders, too, are no exclusion criteria for ADHD anymore.
ADHD has a higher prevalence than OCD and is overall one of the most common psychiatric disorders, with a worldwide prevalence of 5.2 % among children and adolescents (Polanczyk et al. 2007) using DSM-IV and DSM-5 criteria. ADHD persists into adulthood in 60–70 % of cases either as a residual or as a full clinical disorder (Biederman et al. 2000; Kessler et al. 2005). The estimated prevalence of adult ADHD in USA, Europe, and the Middle East is 3.4 % (range 1.3–7.3 %) (Fayyad et al. 2007; Kessler et al. 2006).
A study concerning the relationship between OCD and ADHD in children and adolescents using familial risk analysis provided further evidence of a familial relationship, in addition to unique aetiological factors for both OCD and ADHD (Geller et al. 2007a, b). This is of special importance because of the high comorbidity for both OCD and ADHD disorders. Sheppard et al. (2010) ascertained in a recent study an ADHD prevalence of 11.8 % in OCD-affected individuals. Masi et al. reported 2006 and 2010 in two samples of consecutive referred paediatric OCD patients a prevalence for comorbid ADHD of 17.1 % and 25.5 % respectively (Masi et al. 2006, 2010). The estimated rate of comorbid OCD among children with ADHD is 8 % (Geller et al. 2000). In our studies, ADHD was the most common comorbidity in early-onset OCD, in which tic and Tourette syndrome were exclusion criteria (Walitza et al. 2008). In this study, comorbidity of ADHD in early-onset OCD seems also to predict a higher severity of OCD and a higher grade of persistence of OCD in a prospective follow-up period (Walitza et al. 2008).
This article aims to summarize and compare findings of structural and functional abnormalities, neuropsychological aspects, biochemical and genetic studies on OCD and ADHD. Despite the high comorbidity of both disorders, only very few studies have investigated both together or have directly compared both within the same study. This article shows in the following those rare studies investigating both disorders and also results of each disorder alone (focusing on meta-analyses, if possible) with a following contrast made by the authors of the present review. Some of the results showed shared aetiological factors and mechanisms for both disorders, whereas other findings differentiated between ADHD and OCD. The aim of this overview is to help to understand the aetiology of psychiatric disorders, in particular concerning ADHD and OCD.
Structural and functional abnormalities in OCD and ADHD
A major aim in recent years has been to shed light on the relationship between clinical symptoms of ADHD and OCD and the underlying brain structure, function, and connectivity. Extensive neuroimaging literature exists on the comparison of either disorders with matched healthy controls, and a variety of methods have been used to assess brain structure, metabolism, and the spatial and temporal organization of brain networks. The timing of information processing is commonly studied with brain imaging methods that exhibit a high temporal resolution in millisecond time range, such as electroencephalography (EEG) or alternatively by magnetoencephalography. Details about brain structure and the spatial activation pattern are best assessed by (functional) magnetic resonance imaging or positron emission tomography (PET). Here, we summarize the most consistent abnormalities found in brain structure and functional activation patterns revealed by structural magnetic resonance imaging, functional magnetic resonance imaging (fMRI), and event-related potentials (ERP) studies for both ADHD and OCD. We focused on similarities and differences of affected brain regions reported across these patient groups and specifically point to meta-analytic studies and their findings. Concluding this section, we summarize the results of the only study that directly compared functional neuroimaging data of paediatric patients with ADHD to patients with OCD (Rubia et al. 2010, 2011).
There is considerable evidence for structural differences in the brains of ADHD patients when compared to age-matched healthy controls. Most of these findings are relatively inconsistent and depend on age and/or medication with stimulants. Regarding age, it has been shown that patients with ADHD show a regional delay in the maturation of cortical thickness, especially in regions responsible for cognitive control such as attention, working memory, inhibition and evaluation of reward contingencies in the prefrontal cortex (Shaw et al. 2007), and a slightly earlier maturation of the primary motor cortex. The authors thus suggested that the abnormal development of cognitive control and motor areas may drive the poor control of motor activity (Shaw et al. 2007).
Recent meta-analyses summarized the most consistently replicated structural differences between ADHD patients and controls. They emphasize the reduced volume of the basal ganglia, especially the lentiform nucleus (globus pallidus and putamen) (Ellison-Wright et al. 2008; Nakao et al. 2011) and the caudate (Ellison-Wright et al. 2008; Frodl and Skokauskas 2012; Nakao et al. 2011; Valera et al. 2007) seen in ADHD patients. More specifically, the abnormal size of the caudate seems to depend on age and has been reported to be most prominent in prepubescents with ADHD (Carrey et al. 2012; Castellanos et al. 2002; Mahone et al. 2011). Furthermore, partial normalization of the basal ganglia volume was found when ADHD patients were treated with stimulant medication (Nakao et al. 2011). Apart from an increased volume of the posterior cingulate cortex, other often reported abnormalities in the form of reduced cortical thickness and/or volume of the total brain (Castellanos et al. 1996, 2002; Hill et al. 2003), corpus callosum (Giedd et al. 1994; Hill et al. 2003), prefrontal (Hill et al. 2003; Shaw et al. 2007; Sowell et al. 2003), temporal (Sowell et al. 2003), and cerebellar cortex (Castellanos et al. 1996, 2002) did not reach significance in the most recent meta-analysis of Nakao et al. (2011). Similarly to ADHD patients, OCD patients showed consistent deviations in the volume of the basal ganglia (Piras et al. 2013, Rotge et al. 2010). Older studies were inconsistent on whether this structure showed enlarged (Baxter et al. 1987, 1988; Scarone et al. 1992), decreased (Luxenberg et al. 1988; Robinson et al. 1995), or normal volume (Aylward et al. 1996; Jenike et al. 1996; Szeszko et al. 2008) in patients (for comprehensive reviews see: Saxena and Rauch 2000; Friedlander and Desrocher 2006; Huey et al. 2008). A review (Piras et al. 2013) and two meta-analyses (Radua and Mataix-Cols 2009, Rotge et al. 2010) pointed to relatively consistent patterns of increased basal ganglia volume in more recent studies. Besides alterations in basal ganglia, the meta-analyses of structural differences between OCD patients and healthy controls also detected reduced grey matter in the frontal eye fields, the dorsolateral prefrontal cortex, and the medial frontal cortex, including the anterior cingulate cortex (ACC) (Radua and Mataix-Cols 2009), the left and right orbito-frontal cortex (OFC), and the supramarginal gyrus (Rotge et al. 2009, 2010). An overview of the regions with altered grey matter volumes in patients, as reported in the above-mentioned meta-analyses (Ellison-Wright et al. 2008; Frodl and Skokauskas 2012; Nakao et al. 2011; Rotge et al. 2010; Radua and Mataix-Cols 2009), is given in Fig. 1.
The centres of the clusters that showed differences in grey matter volumes of patients with ADHD or OCD in five recent meta-analyses (Ellison-Wright et al. 2008; Frodl and Skokauskas 2012; Nakao et al. 2011; Rotge et al. 2010; Radua and Mataix-Cols 2009) are plotted as spheres (r = 4 mm) on sagittal (top) and axial slices (bottom) using MRICron (Rorden et al. 2007). Alterations in the grey matter volumes of patients with ADHD are shown in blue and of patients with OCD in red/yellow. Nicely visible are the differences in the volume of the basal ganglia in ADHD (reduced volume: light blue) and OCD (increased volume: yellow) as compared to controls
The structural abnormalities thus nicely converge with the neurobiological models, suggesting a failure of cortico-striato-thalamico-cortical (CST) circuit function in ADHD and OCD patients (van den Heuvel et al. 2010).
In line with structural findings, the results of a meta-analysis in adult OCD patients pointed to activation differences in corresponding functional brain networks (Brem et al. 2012; Menzies et al. 2008). Apart from clear support for abnormal activation in orbito-fronto-striatal regions, lateral frontal, anterior cingulate, middle occipital, and parietal cortices, the cerebellum also exhibited altered activation in cognitive tasks (Menzies et al. 2008). A preliminary meta-analysis in paediatric OCD patients largely converged with these findings, even though the direction of activation differences yielded partly opposing results (Brem et al. 2012). The alterations in the activation pattern of ADHD differed between children and adults as shown in a recent meta-analysis. Both adults and children yielded hypoactivation in fronto-parietal executive function networks that have been related to the well-known deficiencies in performing goal-directed executive processes and hyperactivation in the default network, suggesting a faulty interregulation between the networks activated during tasks and the default network (Cortese et al. 2012). Further alterations in activation have been detected in the ventral attention and the somatomotor networks in children and in the visual and dorsal attention systems in adults (Cortese et al. 2012).
The ACC converged in showing both structural and functional alterations in ADHD and OCD patients as compared to healthy controls. The ACC has an important role in attentional and emotional processes (Bush et al. 2000; van Veen and Carter 2002a) but, moreover, is also involved in conflict detection and evaluation (Botvinick et al. 1999; Carter et al. 2000; Durston et al. 2003a; Ridderinkhof et al. 2004; Ullsperger and von Cramon 2004) and performance monitoring (Albrecht et al. 2010, 2008; Maltby et al. 2005; Ridderinkhof et al. 2004; Ullsperger and von Cramon 2004, 2006; Ursu et al. 2003). The characteristic overactivation of this brain structure in OCD patients points to excessive activity in the action monitoring system when processing errors or correct responses in high-conflict trials (Maltby et al. 2005; Ursu et al. 2003) and has thus been suggested to reflect a neural correlate of the patients’ continuing sense that something is not quite “right” (review see: Aouizerate et al. 2004) and requires correction. In contrast, performance monitoring and error and conflict processing in ADHD patients seem to induce less activation in the ACC as demonstrated by fMRI (Durston et al. 2003b; Rubia et al. 2010, 2005; Tamm et al. 2004) and ERP studies (Albrecht et al. 2010, 2008; Groen et al. 2008; Liotti et al. 2005; McLoughlin et al. 2009; van Meel et al. 2007). The high time resolution of ERPs allows one to better disentangle conflict-related from actual error-related effects through response-locked averaging. An electrophysiological correlate of ACC activity which can be detected in the ERP is the response-locked error-related negativity (ERN, Ne) occurring at around 50–150 ms after error commission. Holroyd and Coles suggested that the Ne emerges when a phasic error signal originating from the mesolimbic dopamine system is processed in the ACC in order to modify performance and update behaviour (Holroyd and Coles 2002). The characteristic fronto-central negativity of this Ne in OCD and ADHD has shown to differ from controls. The more pronounced Ne amplitudes found in children (Endrass et al. 2008; Grundler et al. 2009; Johannes et al. 2001) as well as in adults with OCD (Hajcak et al. 2008; Santesso et al. 2006) are in line with the stronger ACC activity seen in fMRI studies. In contrast to OCD patients with their overactive response monitoring system, patients with ADHD show diminished Ne and ACC activity (Albrecht et al. 2010, 2008; Bush et al. 1999; Durston et al. 2003b; Groen et al. 2008; Liotti et al. 2005; McLoughlin et al. 2009; Rubia et al. 1999; Tamm et al. 2004; van Meel et al. 2007). A very recent meta-analysis of the Ne in adolescent and adult patients with ADHD clearly supported previous findings of Ne attenuation (Geburek et al. 2013) and provides further evidence for a deficit in cognitive control mechanisms.
Anterior cingulate cortex activity has not only been related to performance monitoring and conflict anticipation (Sohn et al. 2007) or processing but seems crucial for inhibition processes as well. Thus, ACC overactivity in OCD may, in addition to excessive performance monitoring, also indicate a failure in the inhibition of prepotent responses in OCD patients causing the repetitive behaviour of compulsions (Maltby et al. 2005). The neurobiological correlates of inhibitory deficits in ADHD contrast to the ones of OCD patients because deficient inhibition mainly emerged as ACC hypoactivation in STOP or flanker tasks (Konrad et al. 2006; Pliszka et al. 2006; Rubia et al. 1999). Hypoactivation and corresponding deficient inhibition in ADHD seem responsible for inappropriate higher-order motor control mechanisms (Rubia et al. 1999). On the other hand, and probably depending on the task, hyperactivation can occur in similar cortical and subcortical structures of ADHD patients (Durston et al. 2003b; Schulz et al. 2004).
ERPs associated with inhibition processes include the fronto-central N2 (or N200) negativity after 200–300 ms and a later (350–600 ms) fronto-central P3 (or P300) positivity. These ERPs have usually been studied with STOP and Go/Nogo tasks (Brandeis et al. 1998; Falkenstein et al. 1999; Kopp et al. 1996). More pronounced amplitudes characterize the N2 and the P3 in response to trials requiring behavioural inhibition, such as Nogo as compared to Go trials. Regarding the N2, the findings in OCD patients are inconsistent: depending on the task, authors reported comparable (Di Russo et al. 2000), enhanced (Ruchsow et al. 2007), or reduced amplitudes and different topographies (Kim et al. 2007) to Nogo trials in the N2. For ADHD, the deficits in the right frontal N2 seemed to dominate in STOP tasks with a high inhibition demand (Albrecht et al. 2005; Dimoska et al. 2003; Liotti et al. 2005; Pliszka et al. 2000). The N2, generated in the caudal region of the ACC, precedes the actual motor response during conflicting trials (van Veen and Carter 2002b). Even though the N2 has traditionally been associated with inhibitory processes, the modulation of its amplitude by conflict level indicated that the N2 primarily reflects conflict processing rather than motor inhibition (Donkers and van Boxtel 2004; Enriquez-Geppert et al. 2010; van Veen and Carter 2002a).
Accordingly, a recent study showed that the conflict-induced amplitude increase in the N2 was significantly reduced in children with ADHD. Furthermore, non-affected siblings exhibited intermediate amplitudes in between ADHD subjects and healthy peers (Albrecht et al. 2010, 2008). The subsequent P3 has been associated with phasic inhibitory motor control mechanisms emerging from the right frontal cortex (Strik et al. 1998). The Nogo P3 typically shows an anteriorisation (Nogo anteriorisation) of its central positivity in contrast to Go trials (Fallgatter and Strik 1999) which has been related to ACC activity and prefrontal response control (Fallgatter et al. 2005). Most often, the P3 in visual Go/Nogo tasks did not differ in amplitude between patients with OCD and controls, even though its latency (Johannes et al. 2001) and topography sometimes differed (Herrmann et al. 2003; Malloy et al. 1989). In contrast, studies on ADHD show quite consistent differences in the Nogo P3. Both children and adults with ADHD showed reduced amplitudes and diminished Nogo anteriorisation in the narrow time window preceding actual response inhibition in the P3 (Fallgatter et al. 2004, 2005).
A direct comparison of functional activation between ADHD and OCD patients is only available from a paediatric sample and for tasks concentrating on executive functions. The group of Rubia examined interference inhibition, selective attention (Rubia et al. 2011), motor response inhibition, and cognitive flexibility (Rubia et al. 2010) using event-related fMRI. Common dysfunction in paediatric patients with ADHD or OCD as compared to controls emerged as hypoactivation in mesial frontal areas: reduced activity in patients was found in the right orbito-frontal cortex and ACC for successful inhibition, in the left medial frontal cortex and ACC for failed inhibition, and finally in bilateral inferior frontal and insular cortices extending also to the left premotor cortex, right superior temporal areas, and putamen for cognitive switching processes (Rubia et al. 2010). Further interference inhibition and selective attention in a modified Simon task was associated with reduced activity in supplementary motor areas, the ACC and superior parietal cortices in both patient groups (Rubia et al. 2011).
Disorder-specific hypoactivation was predominantly found for ADHD patients and again was condition and task specific: activation in the left putamen, caudate, cingulate, and parietal cortex was reduced as compared to healthy controls and OCD patients during cognitive switching (Rubia et al. 2010) and in the Simon task (Rubia et al. 2011). The pattern of functional deficits in the basal ganglia thus corresponds to the consistent structural abnormalities reported for ADHD (Ellison-Wright et al. 2008; Nakao et al. 2011). Failed stop trials were furthermore associated with diminished right middle and inferior prefrontal activation in ADHD as compared to healthy controls and OCD patients (Rubia et al. 2010).
Disorder-specific alterations in brain activation of children with OCD were less pronounced. They differed from healthy controls and ADHD patients only in the oddball condition by showing reduced activation in the right superior and middle frontal gyri of the dorsolateral prefrontal cortex (Rubia et al. 2011). It however remains questionable whether this finding is confounded by effects of medication and symptom severity in the relatively small group of partly remitted OCD patients with only low symptom levels (Rubia et al. 2010).
In summary, deficits in the cortico-striato-thalamic circuits responsible for cognitive control and performance monitoring processes are characterized in both neuropsychiatric conditions: ADHD and OCD. According to the nature of their symptoms situated at the opposite ends of the impulsive–compulsive spectrum, they either exhibit hypo- or hyperactivation of affected brain structures such as basal ganglia or the mesial frontal cortex (Rubia et al. 2010; Carlsson 2000). Affected CST networks and the resulting deficits in cortical inhibition and/or disinhibition may thus, on the one hand, facilitate the perseverative, compulsive behaviours seen in OCD patients but, on the other hand, also explain the disinhibited, impulsive, inattentive behaviour of ADHD patients.
Neuropsychological aspects in OCD and ADHD
Neuropsychological deficits have been described for adults with OCD in the domain of executive functions, especially impaired inhibition, impaired control of interference/conflict, diminished cognitive flexibility in switching, and cognitive alternation tasks (Abbruzzese et al. 1997; Aycicegi et al. 2003; Chamberlain et al. 2006, 2007; Gu et al. 2008; Remijnse et al. 2006; Veale et al. 1996; Watkins et al. 2005), as well as impaired planning (Cavedini et al. 2001; Chamberlain et al. 2007; Mataix-Cols et al. 2002; Nielen and Den Boer 2003; van den Heuvel et al. 2005). Several studies report problems in visuo-spatial working memory (Moritz et al. 2011; Savage et al. 1996), implicit learning tasks (Goldman et al. 2008; Kathmann et al. 2005), and, less consistently, visuo-spatial learning (see Simpson et al. 2006; Penades et al. 2005; Savage et al. 1999; meta-analyses by Olley et al. 2007; Abramovitch et al. 2013; but see analysis by Harkin and Kessler 2011). Deficits in motor and processing speed have also been reported (Burdick et al. 2008) with slower responding in OCD compared to controls. Only few studies have investigated neuropsychological performances in paediatric OCD, which partly replicate findings from OCD in adults on impaired inhibition (Rosenberg et al. 1997; Woolley et al. 2008; but see Beers et al. 1999; Shin et al. 2008; Ornstein et al. 2010), cognitive flexibility (Shin et al. 2008; Ornstein et al. 2010; but see Beers et al. 1999), planning (Andres et al. 2007; Behar et al. 1984; Cox et al. 1989; but see Beers et al. 1999), and visual memory (Andres et al. 2007; but see Behar et al. 1984 ; Cox et al. 1989). Poor fine motor skills and visuo-spatial skills in paediatric OCD seem to predict the persistence of OCD into adulthood (Bloch et al. 2011). Neuropsychological deficits have also been found in remitted OCD (Chamberlain et al. 2007; Rao et al. 2008) or in close relatives (Chamberlain et al. 2008), which suggests that they are trait markers or endophenotypes of OCD. In ADHD research, a large number of studies have investigated neuropsychological functioning both in children and adults. There is agreement that neuropsychological deficits in ADHD are heterogeneous and that only about 30–50 % of ADHD patients present clinically relevant neuropsychological impairment when assessed by objective tests (Biederman et al. 2004; Lambek et al. 2011; Loo et al. 2007; Nigg et al. 2005). Meta-analyses report consistent deficits in the domains of response inhibition, vigilance, planning, and working memory (Huang-Pollock et al. 2012; Kasper et al. 2012; Willcutt et al. 2005) in children; verbal fluency, inhibition, set-shifting (Boonstra et al. 2005), and focused and sustained attention (Balint et al. 2009) in adults; and interference control and enhanced reaction time variability in both (Kofler et al. 2013; Lansbergen et al. 2007).
Cognitive style and error processing
Metacognition is impaired in OCD and the cognitive style of patients with OCD is marked by doubts about their own performance (Hermans et al. 2008; but see Moritz et al. 2011) and an overly cognitive self-consciousness which might interfere with effortful encoding (Exner et al. 2009; Kikul et al. 2011). The opposite phenomenon has been observed in a subgroup of children with ADHD (Hoza et al. 2002; Owens et al. 2007; Rizzo et al. 2010) and, to a lesser extent, in adults (Jiang and Johnston 2012; Knouse et al. 2005): they show a characteristic overestimation of competence and/or performance, which is known as “positive illusory bias”. Children with ADHD show impaired error monitoring and a lack of characteristic post-error slowing in inhibitory response tasks (Schachar et al. 2004). As mentioned above, in electrophysiological studies, this impairment is reflected by a diminished amplitude of the error-related negativity (Albrecht et al. 2008). In OCD patients, in contrast, error-related negativity is enhanced (Endrass et al. 2008).
Decision-making and reward-related processing
During the last years, neuropsychological OCD research has focussed on decision-making and reward-related learning, with inconsistent results for tasks with implicit or complex reward contingencies (Cavedini et al. 2002; Chamberlain et al. 2007; Dittrich and Johansen 2013; Lawrence et al. 2006; Nielen et al. 2002; Watkins et al. 2005). However, a recent study based on large groups indicates that impaired decision-making might be a key feature in OCD (da Rocha et al. 2011) and already present in childhood (Kodaira et al. 2012). More consistent deficits have been found in reversal learning and response cost paradigms: patients with OCD persist in their response strategy in spite of changed reward contingencies (Chamberlain et al. 2008; Remijnse et al. 2006), or with the risk of smaller gains (Chamberlain et al. 2007). It has been hypothesized that impaired learning from feedback (Nielen et al. 2009) might be at the origin of impaired cognitive flexibility or an overcautious cognitive style. However, learning from feedback seems intact when it leads to the avoidance of negative consequences (Endrass et al. 2011). Similarly, ADHD research on decision-making and learning from feedback has yielded mixed results, but there is agreement that sensitivity to reinforcement is altered (Luman et al. 2010; Modesto-Lowe et al. 2013). Children with ADHD may opt for a smaller reward when this helps them to avoid waiting time (“Delay Aversion” (DA)) (Bitsakou et al. 2009; Sonuga-Barke 2002), and they are more responsive to immediate than to delayed rewards (Sagvolden et al. 2005).
Contrasting OCD and ADHD
Vloet et al. (2010) directly compared neuropsychological performances in adolescents with OCD or ADHD using a serial reaction time task, developed to assess implicit sequence learning, and a DA task in order to assess abnormal motivational processes. Subjects with ADHD chose less frequently the larger, more delayed reward compared to those with OCD and controls. Subjects with OCD showed impaired implicit learning. In contrast, the ADHD group was unimpaired in their implicit learning behaviour and the OCD group was not characterized by a DA style. Within the OCD group, severity of obsessions was associated with implicit learning deficits and impulsive symptoms with DA in the ADHD group. In other tasks and domains, however, the differentiation of the two disorders is less evident: In a meta-analysis of the Stop-Task, Lipszyc and Schachar (2010) compared studies with different psychiatric populations and found medium effect sizes for deficits in stop signal reaction time for both ADHD (g = 0.62) and OCD (g = 0.77), reflecting the diminished speed of the inhibitory process. In a recent study comparing adults with ADHD and OCD, Abramovitch et al. (2012) found similar deficits of response inhibition in both disorders, but higher self-reported impulsivity in the ADHD group. These authors view executive function deficits in OCD as an epiphenomenon caused by the overflow of intrusive thoughts. According to their executive overload model, cognitive deficits in OCD patients result from the attempt to gain control over automatic processes in order to reduce impulsive behaviour and lapses of attention. This leads to increased consummation of cognitive resources and in return to diminished effective control.
Neuropsychological profiles of subgroups
In ADHD as in OCD, apparent inconsistencies in neuropsychological findings have been explained by the existence of disorder-specific subgroups with differing neuropsychological key deficits. In OCD, the paradox of concurrent findings of diminished inhibitory control and slow responding has been related to different symptom dimensions, e.g. contrasting obsessional plus “slow decision-making” symptoms vs. compulsive plus “inhibition deficit/rigid” symptoms (da Rocha et al. 2008; Friedlander and Desrocher 2006; Mataix-Cols et al. 2005). Differential neuropsychological profiles have been described e.g. in patients with obsessions related to checking, symmetry/ordering, or contamination (Hashimoto et al. 2011; Jang et al. 2010), in “checkers” compared to “washers” (Nedeljkovic et al. 2009) and in different types of compulsion (Fineberg et al. 2010). Similarly, contradicting neuropsychological findings in ADHD have been explained by different neurobiological origins and the ensuing heterogeneity of neuropsychological symptoms. Accordingly, neurocognitive problems in children with ADHD may be due to dysfunctional executive functions, to a dysfunctional motivational/reward system, or to a combination of both (Sonuga-Barke 2005). Recently, impaired time processing has been suggested as a possible third pathway (Sonuga-Barke et al. 2010).
Comorbidity and neuropsychological deficits
Comorbidity may attenuate or enhance neuropsychological symptoms. Compared to “pure” ADHD, comorbid ADHD with OCD seems to go along with attenuated neuropsychological impairment (Arnold et al. 2005). The impact of comorbid ADHD on neuropsychological deficits in OCD patients, compared to “pure” OCD, has not yet been systematically investigated. However, comorbid ADHD in childhood-onset OCD seems often to be associated with hoarding symptoms (Fullana et al. 2013; Sheppard et al. 2010), and the neuropsychological profile of patients with hoarding closely resembles that of ADHD inattentive subtype patients, with symptoms of diminished sustained attention (Tolin et al. 2011). Neuropsychological deficits have been found to be less pronounced in OCD with comorbid tics or Tourette disorder (Chang et al. 2007; Rankins et al. 2005; Watkins et al. 2005), or differentially affected in the presence of disorders from the autistic spectrum (Zandt et al. 2007, 2009). In childhood ADHD, comorbidity with tics/Tourette seems to result in a combination of neuropsychological problems associated with both disorders (Greimel et al. 2011; Shin et al. 2001). When ADHD symptoms are present in high-functioning autism or Asperger syndrome, neuropsychological deficits may correspond to a combination of characteristics from both disorders, with more severe deficits than in autism alone (Yerys et al. 2009), but attenuated compared to “pure” ADHD (Sinzig et al. 2008; but see van der Meer et al. 2012).
Functional neurochemistry of neurotransmitter circuitry systems in OCD and ADHD
Neurotransmitter interactions and homeostasis are essential features of normal behaviour. The seminal work of Albin et al. (1989), Alexander and Crutcher (1990), DeLong et al. (1985) and others implicated various “loop-systems” for the various phenotypes of human and animal behaviour. The CST circuitry and its subregional connections play a major role; hyperkinetic disturbances are based on reduced stimulation of the substantia nigra pars reticulata and the medial globus pallidus by the subthalamic nucleus (NST). This can be caused by a disturbance of the NST (ballism) or via reduced striatal inhibition of the lateral globus pallidus (choreatic movement) (Reiner et al. 1988). In both cases, the result is disinhibition of the thalamus which in consequence leads to reduced feedback on cortical areas (Crossman et al. 1985). Sensory impulses may be causal for the hyperkinetic movements. Healthy individuals are able to suppress such reactions (Albin et al. 1989). Striatal nerve cells, which are sensitive for such sensory stimuli (Crutcher and DeLong 1984), seem to play a key role in uncontrolled sensory inputs (Paloyelis et al. 2012).
In the past, electrophysiological studies formed the basis in the development of circuitry systems. More recent experimental work has aimed at elucidating the interaction of neurotransmitters in such “loops”. Such work has been reviewed in detail by Berger and Riederer (1992), Mehler-Wex et al. (2006), Rommelfanger and Wichmann (2010), Carlson et al. (2006), and many others. They all focus primarily on disturbances of circuitry systems in motor behaviour (hypo- and hyperkinetic syndromes such as Parkinson’s disease (PD), Huntington’s Chorea, ADHD) and less often on mood disorders, such as schizophrenia.
Due to seminal studies by the Viennese Oleh Hornykiewicz and Walther Birkmayer in the early 1960s, which found that a deficiency of dopamine in the striatum of patients with PD could be substituted by L-DOPA, thereby improving major symptoms of PD, akinesia, rigidity, and tremor substantially, most work in the past has concentrated on “dopamine” as a major neurotransmitter for “motoricity” and “reward”. There is a structural abnormality in children with ADHD supporting the hypothesis of a nigro-striatal defect (Romanos et al. 2010) underlying motor behavioural alterations in this disorder. Additionally, impulsivity, attention deficit, and mood changes seem to be related to modulating circuits involving other brain areas.
Not only dopaminergic drugs can influence impulsivity and compulsive behaviour. This is shown by recent experiments demonstrating that blockade of noradrenergic α2 receptors improves sustained attention and response inhibition while α1- and β1- and β2-adrenergic receptor blockade disrupted go performance and sustained attention (Bari and Robbins 2013). Such data clearly demonstrates noradrenergic neurotransmitter interactions within mood circuitries. This is substantiated by genetic models using dopamine transporter (DAT), norepinephrine transporter (NET), and serotonin transporter (SERT) knockout mice. These observations by Gallagher et al. (2013) correlate with behavioural studies indicating that SERT knockout mice display anxiety-like phenotypes, while NET knockouts and to a lesser extent DAT knockout mice display antidepressant-like phenotypic features (Gallagher et al. 2013).
The D4 receptor is enriched in the prefrontal cortex and thus has been implemented in mood disorders. Yuen et al. (2013) described the restoration of glutamatergic transmission by D4 receptors in stressed animals. It is of interest that attention deficits can be induced by blocking N-methyl D-aspartate (NMDA) receptors in the prefrontal cortex and this is associated with enhanced glutamate release and cyclic adenosine monophosphate response element binding phosphorylation (Pozzi et al. 2011). Increased concentrations of glutamate in the ACC of subjects with borderline personality disorder with and without comorbid ADHD have been detected in cross-sectional proton magnetic resonance spectroscopy studies (Hoerst et al. 2010; Rusch et al. 2010). The close relationship and interaction between dopaminergic and glutamatergic neurotransmission has been described in the late 1980s. From our own work, we concluded that limbic dopaminergic activity is associated with psychotic states, while the same behaviour can be seen with reduced NMDA receptor channel blockade (Berger and Riederer 1992). Quality, quantity, regional, and subregional occurrence of such interaction determines the phenotype of symptomology.
Another neurotransmitter of interest is serotonin. This neurotransmitter is a “modulator”, like a “fine tuning” system, that interacts with many other neurotransmitters such as dopamine and glutamate. Therefore, it is not unlikely to assume that serotonin is also involved e.g. in impulsivity (Dalley and Roiser 2012). As summarized by Hunt et al. (1982) the aminergic neurotransmitter hypotheses for ADHD have been developed in particular in the 1980s. These studies included the measurement of serotonin in blood (Haslam and Dalby 1983) as well as measurements of total, free, and bound tryptophan (Ferguson et al. 1981; Hoshino et al. 1985; Irwin et al. 1981) with in part discrepant results. More recent studies demonstrate an inverse relationship between trait impulsivity and the acute tryptophan depletion effect on reactive aggression after low provocation in patients with adolescent and adult ADHD (Kotting et al. 2013; Zimmermann et al. 2012). While there seems to be a relationship between acute tryptophan depletion and attentional performance in adult patients with ADHD (Mette et al. 2013), there is no such effect on verbal declarative memory in young patients with ADHD (Zepf et al. 2013) and on processing affective prosody in male adults with ADHD (Grabemann et al. 2013).
As already elaborated in chapter 2, the fronto-striatal loop plays a major although not exclusive role in OCD symptomology. This correlates with findings of e.g. Gonçalves et al. (2011) and the fact that frontal-subcortical circuits are involved in behavioural aspects (Cummings 1995).
Furthermore, an OFC pathological neural substrate underlying olfactory identification impairment, impulsivity, and OCD has been described by Bersani et al. (2013). In contrast, deficits in visual memory, executive functions, and attention indicate that regions outside of the OFC may be involved in OCD (Bersani et al. 2013). The specific involvement of the NST in emotional processes in humans has been further described by Buot et al. (2012). These authors showed that the ventral part of the NST processes the emotional violence of stimuli independently of the motor context and that dopamine enhances the processing of pleasant information (Buot et al. 2012). In addition, experimental work in monkeys suggest that overactivity of the ventral anterior and medial dorsal nuclei of the thalamus provokes compulsive-like behaviours and neurovegetative manifestations including anxiety in patients with OCD (Rotge et al. 2012).
While plasma catecholamines and metabolites are not changed in OCD (Benkelfat et al. 1991) concurring with no change in cerebrospinal fluid (CSF) concentrations of biogenic amines and metabolites (Leckman et al. 1995), supersensitive beta-adrenergic receptors are measured by detecting adenylate cyclase activity in platelets of OCD patients (Marazziti et al. 2009).
The role of dopamine in OCD is becoming more significant especially since the augmentation of dopaminergic receptor antagonists shows positive treatment responses (Koo et al. 2010). In fact, PET-studies labelling D1 receptors have demonstrated down regulation in the striatum (Olver et al. 2009) and ACC (Olver et al. 2010). Imaging studies also show a reduction of D2 binding (Nikolaus et al. 2010). Increased dopaminergic activity might contribute to these findings. This corresponds to the findings that metabolism via catecholamine-O-methyltransferase (COMT) and monoamine-oxidase-A (MAO-A) demonstrates polymorphisms in both these genes in males as shown by a meta-analysis by Taylor (2013), while DAT1- and DRD3-polymorphisms could not be identified so far.
As with disturbances in the glutamatergic system, there is evidence for significant increases of both glutamate and glycine in the CSF of OCD patients (Bhattacharyya et al. 2009). As indicated by a multivariate analysis of variance, CSF glycine concentrations were even higher in those OCD patients who had autoantibodies compared with those without (Bhattacharyya et al. 2009).
Using proton magnetic resonance spectroscopy (MRS), female OCD patients had a significantly reduced concentration of glutamate–glutamine in subareas of the ACC. In addition, male and female OCD patients had higher concentrations of myoinositol-containing compounds in their right rostral and dorsal ACC (Yucel et al. 2008). However, in the medial prefrontal cortex (MPFC), voxel-based imaging including the pregenual ACC (Simpson et al. 2012) could not detect glutamate–glutamine abnormalities in unmedicated OCD adults, while MPFC gamma-aminobutyric acid (GABA) levels were decreased. MRS studies measuring N-acetylaspartate showed significantly lower concentrations in the left head of the caudate nucleus (HOC) in non-medicated patients with OCD compared to medicated ones, while preliminary data suggest a correlation of behaviour therapy with a decrease in glutamate–glutamine in the right HOC (Whiteside et al. 2012).
It remains to be clarified in further studies whether OCD is a hyperglutamatergic and ADHD a hypoglutamatergic condition with prefrontal brain regions being especially affected as hypothesized by Carlsson (2001). Although there is ample evidence for an involvement of glutamatergic perturbations in OCD, it is the resulting treatment strategy that proves or disproves this concept. Therefore, it is an interesting notion that lamotrigine augmentation of selective serotonin re-uptake inhibitor (SSRI) treatment has been regarded as an effective therapeutic strategy (Bruno et al. 2012). Memantine add-on to fluvoxamine significantly improved short-term outcomes in patients with moderate to severe OCD (Ghaleiha et al. 2013; Hezel et al. 2009; Stewart et al. 2010).
Adjunctive glycine treatment (a NMDA receptor agonist) approached efficacy in OCD patients (Greenberg et al. 2009) while ketamine, a potent non-competitive NMDA receptor antagonist, has been studied in treatment-refractory OCD. Ketamine effects on OCD symptoms, in contrast to depressive symptoms, did not seem to persist or progress after the acute effects of ketamine had dissipated (Bloch et al. 2012).
The “serotonin hypothesis” of OCD has been developed in the 1980s (March et al. 1989) and was based on CSF concentrations of 5-HIAA, which were significantly increased in OCD (Insel et al. 1985). Pharmacological strategies with zimelidine, a 5-HT uptake inhibitor, reduced CSF-5-HIAA concentrations but were clinically ineffective (Insel et al. 1985). Moreover, the behavioural responses of OCD patients to m-chlorophenylpiperazine (MCPP) and tryptophan treatment had no effects on OCD symptoms (Charney et al. 1988). However, clomipramine improved symptoms worsened with metergoline, a 5-HT antagonist, in patients who had improved with clomipramine, a semiselective 5-HT uptake inhibitor (Murphy et al. 1989). MCPP, a 5-HT receptor agonist, increased anxiety, depression, and dysphoria in untreated OCD patients (Murphy et al. 1989). Regarding Cochrane analyses and meta-analyses, SSRIs are the first choice of medication for OCD in children and adults and are able to alleviate OCD symptoms significantly (Westenberg et al. 2007). Serotonin-norepinephrine re-uptake inhibitors are less effective and only third choice, but have been described as showing fewer side effects (Sansone and Sansone 2011).
All in all, SSRIs lack efficiency in ADHD while they are highly efficient in OCD. In contrast, dopaminergic and noradrenergic interventions are effective in many although not all patients with ADHD. If we summarize the involvement of various neurotransmitters in ADHD, the following rank order is envisaged: dopamine–noradrenaline–glutamate–serotonin, while for OCD, the following rank order is envisaged: serotonin–glutamate = dopamine–noradrenaline.
Genetic aspects in OCD and ADHD
Twin and family studies
OCD and ADHD twin and family studies indicate high familiality in both disorders (Walitza et al. 2010; Franke et al. 2012). The heritability of obsessive compulsive symptoms ranges from 0.45 to 0.65 in children and from 0.27 to 0.47 in adults (van Grootheest et al. 2005). For ADHD, the heritability was estimated to be around 70–80 % (Faraone et al. 2005). However, more recent quantitative systematic approaches, which took into account possible biases of previous twin studies (such as lack of power to detect sibling interactions and the correction used for contrast effects), concluded that genetic factors explained 60 % of the variance of ADHD (Wood and Neale 2010). Recently, it was reviewed that many twin studies vary in several phenotypic and measurement aspects, thereby strongly influencing heritability estimates, in turn indicating that one should be cautious regarding the interpretation of these results (Freitag et al. 2010). In addition, the strong evidence supporting the notion that ADHD is an extreme of a continuous trait lead Larsson et al. (2012) to investigate the genetic links in twins between the extreme and the subthreshold range of ADHD symptoms. They found a strong genetic link between the extreme and the subthreshold variation, with almost identical group heritability estimates of around 0.60 for the diagnostic (prevalence 1.78 %) and screening (prevalence 9.75 %) criteria of ADHD (Larsson et al. 2012). Moreover, Larsson et al. (2013) described high heritability of ADHD (0.88, 95 % CI 0.83–0.93) for the entire twin sample composed of over 50,000 twins, while shared environmental effects were non-significant. Similarly, in OCD, a more recent twin study (van Grootheest et al. 2008) indicated that genetic factors contributed significantly to variations in obsessive compulsive symptom liability that were dependant on age: only 27 % at the age of 12 years, but 57 % at the age of 14 years, and 54 % at the age of 16 years. There were no sex differences in heritability, while gender difference did influence prevalence (higher prevalence in girls at age 14 and 16). Only at age 12 did environmental factors shared by children from the same family contribute significantly (16 %) to individual differences in obsessive compulsive symptom scores.
Family studies showed that first-degree relatives of patients with OCD were affected by OCD considerably more frequently than relatives of healthy control subjects (Bellodi et al. 1992; Pauls et al. 1995; Nestadt et al. 2000; Hanna et al. 2005a, b; do Rosario-Campos et al. 2005). However, in a representative recent study of Steinhausen et al. (2013) no effect of age of onset on heritability was found. Family studies showed that there is a type of OCD which might be more familial and another type which is probably more de-novo and perhaps triggered more by environmental factors. Furthermore, the studies showed that early-onset OCD seems to be a more genetic and neurobiological condition. Similarly, familial studies have shown that the risk of ADHD among parents and siblings of children who had ADHD is increased starting at two-up to eightfold higher (Wilens et al. 2005). Adoption and twin studies can help to separate, although not completely, genetic from environmental factors observed in family studies (Wood and Neale 2010). Adoption studies have unequivocally found that biological relatives of children with ADHD are more likely to be hyperactive compared to adoptive relatives (Faraone and Khan 2006).
Linkage studies
Many linkage analysis studies have been conducted in ADHD samples including child as well as adult patients with ADHD (Franke et al. 2012). Several chromosome regions have been suggested to be significantly linked to ADHD (see Table 1). A meta-analysis including 7/9 independent studies showed that the distal part of chromosome 16q is linked to ADHD (contains e.g. the CDH13 genes) (Zhou et al. 2008). This has been also shown in genome-wide association studies (GWAS, Lesch et al. 2008).
Similarly, several linkage studies (Arcos-Burgos et al. 2004; Hebebrand et al. 2006; Romanos et al. 2008) as well as one meta-analysis (Ogdie et al. 2006) indicate a significant linkage on chromosome 5 in a region containing the dopamine D1 receptor as well as the dopamine transporter genes (DAT1, SLC6A3). These candidate genes have also been found in many association studies to be significantly associated with ADHD (Nemoda et al. 2011). Therefore, we assume that these two dopaminergic genes seem to contribute to ADHD.
In comparison with ADHD, only five genome-wide linkage (GWL) studies of OCD have been published so far (see Table 1). In all five studies, no significant genome-wide evidence for linkage was detected according to standard guidelines for linkage studies (Lander and Kruglyak 1995). However, several loci displayed suggestive evidence for linkage findings. In particular, chromosome 1 seems to repeatedly show evidence for linkage with OCD (Hanna et al. 2007; Shugart et al. 2006; Ross et al. 2011; Mathews et al. 2012). Another frequent finding is from Hanna et al. (2002) who found in a second GWL scan the maximum linkage signal on chromosome 10p15. Concordantly, Mathews et al. (2012) also found a linkage signal in a nearby region (10p13). Chromosome 10 seems to show a more specific contribution to OCD since no findings were reported in ADHD (see Table 1).
Association studies
To date, although several GWAS as well as meta-analyses for association studies in ADHD have been conducted, no single single-nucleotide polymorphisms (SNP) or polymorphism has been found to be affected in ADHD (see Table 2; Zhang et al. 2012). Furthermore, similar as in ADHD, no single SNP or polymorphism has been found to be affected in OCD, as found in the only GWAS published to date (Stewart et al. 2013b), in which no SNP reached genome-wide significance, as well as from the meta-analysis conducted by Taylor (2013). Nevertheless, it seems that dopaminergic, serotonergic, noradrenergic, synaptic, and growth factor genes are involved in ADHD, while in OCD, the serotonergic and glutamatergic genes seem to play a greater role (see Table 2).
Dopaminergic genes
Although SSRIs are the first-line treatment for OCD, in cases of non-response, augmentation of low-dose neuroleptics is sometimes effective (Komossa et al. 2010). This implies that there is involvement of dopamine-related genes in OCD. Nevertheless, only COMT showed some significant association in OCD after an extensive meta-analysis (Taylor (2013); Table 2). Clinical studies with responders and non-responders to drug treatment were stratified according to dopamine D2 Taq/A and COMT Val158Met genotypes (Vulink et al. 2012). There was no significant difference in genotype distribution or allele frequencies of the COMT or dopamine receptor D2 (DRD2) between responders and non-responders to citalopram with quetiapine. However, OCD patients with the Met/Met genotype (48 %) of the COMT polymorphisms showed a treatment response to 10-week citalopram in drug-free/drug-naive OCD patients (Vulink et al. 2012). This is in line with some clinical findings showing that lower activity of COMT associated with the Met allele lead to poorer executive function in OCD (Tukel et al. 2013). Recently, COMT mRNA was shown to be expressed significantly lower in patients with OCD compared to controls in peripheral blood samples (Wang et al. 2009). Influence of variations in the DAT1 and COMT genes on neural activation during response inhibition with different activation during inhibition have been described. Inhibitory control seems therefore associated with variation of dopamine function (Congdon et al. 2009). But recent studies, genome-wide linkage scans and GWAS, are contradictory considering the “classic” dopaminergic genes like COMT. That resulted in no significant association with ADHD after meta-analysis (Sun et al. 2013; Zhang et al. 2012). While the COMT-SNP rs4680 (Val158Met) Met allele reduces COMT enzyme activity and is associated with impulsiveness and substance abuse in ADHD, Soeiro-De-Souza et al. (2013) compared the Met/Met genotype with the Val/Val genotype in healthy individuals. These authors demonstrated that the rs4680 Met/Met genotype was associated with higher impulsivity on the BIS-11 s-order factor Non-planning scale. Therefore, such data are in line with the suggestion that increased dopamine concentration induces impulsivity and substance abuse depending on the sensitivity of motor- and limbic circuitry systems (Soeiro-De-Souza et al. 2013). Involvement of dopamine systems in the pathology of ADHD is also evident from PET-studies with 11C-altropane. It could be shown that both ADHD and the 3′-UTR (SLC6A3) DAT1 polymorphism had additive effects on 11C-altropane DAT binding (Spencer et al. 2013). Similarly, a single-photon emission computed tomography meta-analysis in healthy controls could show nominal higher levels of striatal DAT in the 9-repeat allele carriers (Costa et al. 2011). According to many association studies followed by meta-analysis, it has been shown that the 10-repeat allele of the DAT1 is a risk allele for ADHD in childhood (Gizer et al. 2009; Table 2), while persistent ADHD in adults was associated with the 9-repeat allele (Franke et al. 2010), findings that might point to a regulatory effect of DAT in brain development. Nevertheless, such association could not be confirmed in a recent meta-analysis for OCD (Taylor 2013; Table 2), pointing to a unique effect in ADHD.
Dopaminergic receptors (D1–D5) are essential in modulating behaviour. The high risk of D2, D4, and D5 receptor polymorphisms in ADHD has been reviewed by Wu et al. (2012). Disruption of D2 signalling in the ventral striatum impairs motivation. In contrast, postsynaptic overexpression in the nucleus accumbens increases in animals the willingness to expend efforts to obtain a goal (Trifilieff et al. 2013). Furthermore, DRD4 and tyrosine hydroxylase (TH) polymorphisms are associated with activity–impulsivity-related traits in dogs (Wan et al. 2013). Several studies suggest that the length of the DRD4 repeat affects the activation of the receptor as well as the mRNA expression of the gene (Nemoda et al. 2011). Meta-analysis in ADHD revealed a significant association between the 7-repeat allele of the DRD4 exon 3 VNTR (OR 1.33, 95 % CI 1.15–1.54) and the disorder (Gizer et al. 2009), while association of the DRD4 4-repeat allele and OCD was indicated by a case–control study (Camarena et al. 2007) and by a family-based study (Walitza et al. 2008), whereas an increased frequency of the DRD4 7-repeat allele was shown in a late-onset OCD group (Hemmings et al. 2004), and in a subgroup of OCD patients with comorbid tics (Cruz et al. 1997). Nevertheless, in a recent meta-analysis, this association to OCD could not be confirmed (Taylor 2013; Table 2). Signalling properties and regulation of DRD4 as well as the interaction of DRD4 in modulating GABAergic transmission has been reviewed by Furth et al. (2013). As the adenosine A2A receptor (ADORA2A) is linked to dopaminergic transmission, Molero et al. (2013) studied the relationship between ADORA2A gene polymorphisms and ADHD traits in 1,747 twins. One of the SNPs, rs35320474, showed a significant correlation to ADHD traits (Molero et al. 2013).
In conclusion, it seems that dopamine-related genes are much more associated with ADHD than with OCD (see Table 2).
Serotonergic genes
Selective serotonin re-uptake inhibitors block the SERT and represent the most effective pharmacological treatment of early and late OCD. Most association studies in OCD have therefore investigated serotonergic genes (see Table 2). This is in contrast to ADHD where pharmacotherapy is focused on the regulation of dopaminergic and noradrenergic dysfunction. The most frequently studied gene in OCD is SERT [SLC6A4], with its functional polymorphism in the upstream region termed 5-HTTLPR, which involves an insertion (L-[long] allele)/deletion (S-[short] allele) polymorphism. In comparison with the S-allele, the L-allele has been reported to exert an increased transcriptional activity and an increased basal re-uptake of 5-HT in vitro (Heils et al. 1996; Lesch et al. 1996; Murphy and Lesch 2008). The L-allele is therefore referred to as the gain-of-function variant of the serotonin transporter. In contrast to anxiety disorders, it has been observed in OCD that the L-allele is associated with the disorder, in particular in early onset (Bloch et al. 2008; Taylor 2013; Walitza et al. 2005). Similarly as for OCD, the L-allele of the SERT was found to be significantly associated with ADHD (OR 1.17 95 % CI 1.02–1.33) (Gizer et al. 2009). This might imply the similarity in dysfunction of impulse control in both disorders, caused by dysfunctions of the serotonergic pathways. Nevertheless, some contradicting results were reported in which no significant association between 5-HTTLPR and ADHD was found in a meta-analysis (Forero et al. 2009).
In line with the serotonergic hypothesis, a significant association with the rs6311 A-allele carriers of the serotonin 2A receptor (HTR2A) with OCD was confirmed by a meta-analysis (Taylor 2013; Table 2). However, this gene seems to be specific to OCD as no positive findings were reported for ADHD (see Table 2).
Another gene related to the serotonergic system is the brain-specific tryptophan hydroxylase-2 (TPH2), the rate-limiting enzyme in 5-HT synthesis in the brain, that was studied for the first time for its association in early-onset OCD (Mossner et al. 2006) and in ADHD by our groups (Walitza et al. 2005). This gene, according to a meta-analysis by Gizer et al. (2009), showed a significant association with ADHD, while it failed to associate with OCD after meta-analysis (Taylor 2013), probably because the numbers of studies with OCD are still too low.
In conclusion, it seems that the serotonin-related genes have some common gene associated with OCD and ADHD (e.g. SERT), although some genes seem to be unique to one disorder (e.g. HTR2A for OCD; HTR1B, TPH2 and MAOA for ADHD).
Noradrenergic genes
Since one of the therapeutic targets of medication (such as atomoxetine) in ADHD is the norepinephrine transporter (NET), this gene and related genes have been studied. Yet, only the dopamine beta hydroxylase (DBH), the enzyme that synthesizes norepinephrine from dopamine, was found to be associated with ADHD after a meta-analysis (Gizer et al. 2009). While neither NET nor other noradrenergic genes were found to be associated with ADHD or with OCD (see Table 2).
Glutamatergic genes
The neuronal glutamate transporter (SLC1A1) gene on 9p24 is one of the few candidate genes for OCD that was investigated due to its localization within a linkage peak by Hanna et al. (2002). The role of this glutamate transporter gene in OCD is also supported by the observation that the anti-glutamatergic drug riluzole can be beneficial in the treatment of OCD and by the finding of elevated glutamate levels in the CSF of OCD patients (Pittenger et al. 2011). Further studies of glutamatergic neurons and SLC1A1 in particular are therefore warranted in early- and adult-onset OCD (Wu et al. 2013a, b). Identification and characterization of three alternative SLC1A1/EAAC1 (excitatory amino-acid transporter 1) mRNAs, P2, ex2skip, and ex11skip (Porton et al. 2013), gave evidence that all isoforms inhibit glutamate uptake from the full-length EAAC1 transporter (Porton et al. 2013). While Wang et al. (2010) did find the variant T164A in one family, these authors did not find statistical differences in genotype and allele frequencies of common SNPs in SLC1A1. All in all, however, the results on SLC1A1 in OCD are at discrepancy. Samuels et al. (2011) genotyped 111 SNPs in or near SLC1A1 and conducted family-based association analyses in 1,576 participants in 377 families. None of the surrounding markers were in linkage disequilibrium with rs301443 (SNP 7.5 kb downstream of the SLC1A1 gene) nor were any associated with OCD. These authors, however, found that rs4740788 was associated with OCD in all families and in families with affected males. A three-SNP haplotype (rs4740788–rs10491734–rs10491733) was associated with OCD in the total sample (Samuels et al. 2011). SLC1A1 rs3056 variant could be shown to be associated with increased total, left, and right thalamic volume in OCD (Arnold et al. 2009). Also, there might be a common locus for OCD and autism spectrum disorders at rs301443 residing between SLC1A1 and JMJD2C (Lysine-specific demethylase 4C/KDM4C) at 9p24 (Kantojarvi et al. 2010). Non-significant trends were identified by Taylor’s meta-analysis report (2013) for the glutamate-related polymorphism rs3087879. In agreement, a much less optimistic message regarding an association between OCD and the 3′-region of SLC1A1 is based on a recent meta-analysis (Stewart et al. 2013a). Nevertheless, the glutamatergic-related genes seem to be unique for OCD, since no significant association has to date been found in ADHD (see Table 2).
Synaptic genes
In regard to the synaptic genes, these have come to attention after GWAS findings in ADHD (Lasky-Su et al. 2008; Neale et al. 2010a; Neale et al. 2010b; Lesch et al. 2008). In particular the genes coding to synaptosomal-associated protein 25 (SNAP25), cadherin 13 H-cadherin (CDH13), and catenin (cadherin-associated protein) alpha-2 (CTNNA2) but also others (see Table 2). Indeed, SNAP25 has been further investigated in independent studies and meta-analyses showing significant association with ADHD (Gizer et al. 2009; Galvez et al. 2013). Furthermore, in a recent study, the variant rs362990 on the SNAP25 gene was associated with ADHD in which the risk A-allele was also associated with additive decrease in the expression of the SNAP25 transcript in the inferior frontal gyrus of 89 unaffected adult post-mortem tissue (Hawi et al. 2013). Moreover, reduced SNAP25 levels in developing glutamatergic synapses alter short-term plasticity, in which glutamatergic neurotransmission is enhanced (Antonucci et al. 2013). Still, the synaptic-related genes should be further investigated in more depth in order to confirm GWAS and other association studies in ADHD. In contrast, in OCD, such studies have not yet been conducted, and therefore, no conclusion in regard to their involvement in the disorder can be conveyed.
Conclusions
OCD and ADHD are frequent psychiatric disorders which are highly comorbid with each other and with other psychiatric symptomatology. In early-onset OCD, ADHD is one of the most common comorbidities. Structural and functional imaging findings have shown abnormalities converging with a failure of CST circuit function responsible for cognitive control and performance monitoring processes in both ADHD and OCD patients.
Neuropsychological tests and corresponding brain activation studies showed, for example, deficits in response inhibition common to both disorders. According to the nature of their symptoms situated at the opposite ends of the impulsive–compulsive spectrum, either hypo- or hyperactivation of affected brain structures such as basal ganglia or the mesial frontal cortex was reported. Nevertheless, the causes of the deficits may be different. In the case of OCD, they could be caused by the overflow of intrusive thoughts, whereas in ADHD, it might be due to a lack of inhibitory control and to an impulsive response style. Abnormal inhibitory processes e.g. may therefore be responsible for both, the perseverative, compulsive symptoms characterizing patients with OCD and the disinhibited, impulsive behaviours seen in patients with ADHD. Neurochemically ADHD and OCD are varied in particular in their pathobiochemical and pathogenetic involvement of dopamine (ADHD) and serotonin (OCD). Fronto-striatal- and orbito-frontal circuitries reflect significant differences from a morphological and neurochemical point of view. The ACC and MPFC have recently received major interest especially in OCD. The molecular genetic findings correspond well to the neurochemical and imaging perspective. Linkage studies show for ADHD, regions of significant linkage on chromosome 16q, containing the CDH13 gene and for chromosome 5 containing the DRD1 and the DAT1 genes, supporting the strong evidence for the involvement of the dopaminergic system in the aetiology of ADHD. In regard to OCD, no significant genome-wide evidence for linkage has been so far detected; however, there is some evidence for linkage on chromosome 1 and 10. In contrast to ADHD, especially association studies in OCD supported the contribution of serotonergic and also glutamatergic genes with the disorder. For some OCD phenotypes, augmentation of SSRIs with dopaminergic-based treatments is recommended. In the case of ADHD so far, dopaminergic- and noradrenergic-based medication remains the first choice medication. In summary, multimodal studies investigating the aetiological factors of psychiatric disorders and phenotypes have the potential to contribute to the ongoing development of more effective and specific treatment strategies not only for the different disorders but also for clinical presentations of broader phenotypes.
Abbreviations
- (f)MRI:
-
(functional) Magnetic resonance imaging
- ACC:
-
Anterior cingulate cortex
- ADHD:
-
Attention deficit hyperactivity disorder
- ADORA2A:
-
Adenosine A2A receptor
- BDNF:
-
Brain derived neurotrophic factor
- cAMP:
-
Cyclic adenosine monophosphate
- COMT:
-
Catecholamine-O-methyltransferase
- CSF:
-
Cerebrospinal fluid
- CST:
-
Cortico-striato-thalamico-cortical
- DA:
-
Delay aversion
- DAT:
-
Dopamine transporter
- DAT1 (SLC6A3):
-
Dopamine transporter gene
- DRD2:
-
Dopamine receptor D2
- DRD4:
-
Dopamine receptor D4
- EAAC1:
-
Excitatory amino-acid transporter 1
- EEG:
-
Electroencephalography
- ERN/Ne:
-
Error-related negativity
- ERP:
-
Event-related potentials
- GABA:
-
Gamma-aminobutyric acid
- GWAS:
-
Genome-wide association studies
- HTR2A:
-
Serotonin 2A receptor
- MAO-A:
-
Monoamine-oxidase-A
- MCPP:
-
M-chlorophenylpiperazine
- MEG:
-
Magnetoencephalography
- MPFC:
-
Medial prefrontal cortex
- MRS:
-
Proton magnetic resonance spectroscopy
- NAA:
-
N-acetylaspartate
- NET:
-
Norepinephrine transporter
- NGA:
-
Nogo anteriorisation
- NMDA:
-
N-methyl D-aspartate
- NST:
-
Subthalamic nucleus
- NTRK2:
-
Neurotrophic tyrosine kinase receptor type 2
- OCD:
-
Obsessive compulsive disorder
- OFC:
-
Orbito-frontal cortex
- PD:
-
Parkinson’s disease
- PET:
-
Positron emission tomography
- PFC:
-
Prefrontal cortex
- SERT (SLC6A4):
-
Serotonin transporter
- SLC1A1:
-
Glutamate transporter gene
- SMA:
-
Supplementary motor areas
- SNP:
-
Single-nucleotide polymorphism
- SPECT:
-
Single-photon emission computed tomography
- SRT:
-
Serial reaction time
- SSRI:
-
Selective serotonin re-uptake inhibitors
- SSRT:
-
Stop signal reaction time
- TH:
-
Tyrosine hydroxylase
- TPH2:
-
Tryptophan hydroxylase-2
- VNTR:
-
Variable number tandem repeat
References
Abbruzzese M, Ferri S, Scarone S (1997) The selective breakdown of frontal functions in patients with obsessive-compulsive disorder and in patients with schizophrenia: a double dissociation experimental finding. Neuropsychologia 35(6):907–912
Abramovitch A, Dar R, Hermesh H, Schweiger A (2012) Comparative neuropsychology of adult obsessive-compulsive disorder and attention deficit/hyperactivity disorder: implications for a novel executive overload model of OCD. J Neuropsychol 6(2):161–191. doi:10.1111/j.1748-6653.2011.02021.x
Abramovitch A, Abramowitz JS, Mittelman A (2013) The neuropsychology of adult obsessive-compulsive disorder: a meta-analysis. Clin Psychol Rev 33(8):1163–1171. doi:10.1016/j.cpr.2013.09.004
Albin RL, Young AB, Penney JB (1989) The functional anatomy of basal ganglia disorders. Trends Neurosci 12(10):366–375
Albrecht B, Banaschewski T, Brandeis D, Heinrich H, Rothenberger A (2005) Response inhibition deficits in externalizing child psychiatric disorders: an ERP-study with the Stop-task. Behav Brain Funct 1:22. doi:10.1186/1744-9081-1-22
Albrecht B, Brandeis D, Uebel H, Heinrich H, Mueller UC, Hasselhorn M, Steinhausen HC, Rothenberger A, Banaschewski T (2008) Action monitoring in boys with attention-deficit/hyperactivity disorder, their nonaffected siblings, and normal control subjects: evidence for an endophenotype. Biol Psychiatry 64(7):615–625. doi:10.1016/j.biopsych.2007.12.016
Albrecht B, Brandeis D, Uebel H, Heinrich H, Heise A, Hasselhorn M, Rothenberger A, Banaschewski T (2010) Action monitoring in children with or without a family history of ADHD—effects of gender on an endophenotype parameter. Neuropsychologia 48(4):1171–1177. doi:10.1016/j.neuropsychologia.2009.12.018
Alexander GE, Crutcher MD (1990) Functional architecture of basal ganglia circuits: neural substrates of parallel processing. Trends Neurosci 13(7):266–271
American Psychiatric Association (1994) Diagnostic and statistical manual of mental disorders, fourth edition (DSM-IV). American Psychiatric Association, Washington
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders, fifth edition (DSM-5). Available via http://worldcat.org. http://dsm.psychiatryonline.org/book.aspx?bookid=556
Andres S, Boget T, Lazaro L, Penades R, Morer A, Salamero M, Castro-Fornieles J (2007) Neuropsychological performance in children and adolescents with obsessive-compulsive disorder and influence of clinical variables. Biol Psychiatry 61(8):946–951. doi:10.1016/j.biopsych.2006.07.027
Antonucci F, Corradini I, Morini R, Fossati G, Menna E, Pozzi D, Pacioni S, Verderio C, Bacci A, Matteoli M (2013) Reduced SNAP-25 alters short-term plasticity at developing glutamatergic synapses. EMBO Rep 14(7):645–651. doi:10.1038/embor.2013.75
Aouizerate B, Guehl D, Cuny E, Rougier A, Bioulac B, Tignol J, Burbaud P (2004) Pathophysiology of obsessive-compulsive disorder: a necessary link between phenomenology, neuropsychology, imagery and physiology. Prog Neurobiol 72(3):195–221. doi:10.1016/j.pneurobio.2004.02.004
Arcos-Burgos M, Castellanos FX, Pineda D, Lopera F, Palacio JD, Palacio LG, Rapoport JL, Berg K, Bailey-Wilson JE, Muenke M (2004) Attention-deficit/hyperactivity disorder in a population isolate: linkage to loci at 4q13.2, 5q33.3, 11q22, and 17p11. Am J Hum Genet 75(6):998–1014. doi:10.1086/426154
Arnold PD, Ickowicz A, Chen S, Schachar R (2005) Attention-deficit hyperactivity disorder with and without obsessive-compulsive behaviours: clinical characteristics, cognitive assessment, and risk factors. Can J Psychiatry 50(1):59–66
Arnold PD, Macmaster FP, Hanna GL, Richter MA, Sicard T, Burroughs E, Mirza Y, Easter PC, Rose M, Kennedy JL, Rosenberg DR (2009) Glutamate system genes associated with ventral prefrontal and thalamic volume in pediatric obsessive-compulsive disorder. Brain Imaging Behav 3(1):64–76. doi:10.1007/s11682-008-9050-3
Aycicegi A, Dinn WM, Harris CL, Erkmen H (2003) Neuropsychological function in obsessive-compulsive disorder: effects of comorbid conditions on task performance. Eur Psychiatry 18(5):241–248
Aylward EH, Harris GJ, Hoehn-Saric R, Barta PE, Machlin SR, Pearlson GD (1996) Normal caudate nucleus in obsessive-compulsive disorder assessed by quantitative neuroimaging. Arch Gen Psychiatry 53(7):577–584
Balint S, Czobor P, Komlosi S, Meszaros A, Simon V, Bitter I (2009) Attention deficit hyperactivity disorder (ADHD): gender- and age-related differences in neurocognition. Psychol Med 39(8):1337–1345. doi:10.1017/S0033291708004236
Bari A, Robbins TW (2013) Noradrenergic versus dopaminergic modulation of impulsivity, attention and monitoring behaviour in rats performing the stop-signal task : possible relevance to ADHD. Psychopharmacology 230(1):89–111. doi:10.1007/s00213-013-3141-6
Baxter LR Jr, Phelps ME, Mazziotta JC, Guze BH, Schwartz JM, Selin CE (1987) Local cerebral glucose metabolic rates in obsessive-compulsive disorder. A comparison with rates in unipolar depression and in normal controls. Arch Gen Psychiatry 44(3):211–218
Baxter LR Jr, Schwartz JM, Mazziotta JC, Phelps ME, Pahl JJ, Guze BH, Fairbanks L (1988) Cerebral glucose metabolic rates in nondepressed patients with obsessive-compulsive disorder. Am J Psychiatry 145(12):1560–1563
Beers SR, Rosenberg DR, Dick EL, Williams T, O’Hearn KM, Birmaher B, Ryan CM (1999) Neuropsychological study of frontal lobe function in psychotropic-naive children with obsessive-compulsive disorder. Am J Psychiatry 156(5):777–779
Behar D, Rapoport JL, Berg CJ, Denckla MB, Mann L, Cox C, Fedio P, Zahn T, Wolfman MG (1984) Computerized tomography and neuropsychological test measures in adolescents with obsessive-compulsive disorder. Am J Psychiatry 141(3):363–369
Bellodi L, Sciuto G, Diaferia G, Ronchi P, Smeraldi E (1992) Psychiatric disorders in the families of patients with obsessive-compulsive disorder. Psychiatr Res 42(2):111–120
Benkelfat C, Mefford IN, Masters CF, Nordahl TE, King AC, Cohen RM, Murphy DL (1991) Plasma catecholamines and their metabolites in obsessive-compulsive disorder. Psychiatr Res 37(3):321–331
Berger W, Riederer P (1992) Neurotransmitter regelkreise. In: Riederer P, Laux G, Pöldinger W (eds) Neuro-psychopharmaka Bd.1. Springer, Wien, pp 225–271
Bersani G, Quartini A, Ratti F, Pagliuca G, Gallo A (2013) Olfactory identification deficits and associated response inhibition in obsessive-compulsive disorder: on the scent of the orbitofronto-striatal model. Psychiatr Res. doi:10.1016/j.psychres.2013.05.032
Bhattacharyya S, Khanna S, Chakrabarty K, Mahadevan A, Christopher R, Shankar SK (2009) Anti-brain autoantibodies and altered excitatory neurotransmitters in obsessive-compulsive disorder. Neuropsychopharmacology 34(12):2489–2496. doi:10.1038/npp.2009.77
Biederman J, Mick E, Faraone SV (2000) Age-dependent decline of symptoms of attention deficit hyperactivity disorder: impact of remission definition and symptom type. Am J Psychiatry 157(5):816–818
Biederman J, Monuteaux MC, Doyle AE, Seidman LJ, Wilens TE, Ferrero F, Morgan CL, Faraone SV (2004) Impact of executive function deficits and attention-deficit/hyperactivity disorder (ADHD) on academic outcomes in children. J Consult Clin Psychol 72(5):757–766. doi:10.1037/0022-006X.72.5.757
Bitsakou P, Psychogiou L, Thompson M, Sonuga-Barke EJ (2009) Delay aversion in attention deficit/hyperactivity disorder: an empirical investigation of the broader phenotype. Neuropsychologia 47(2):446–456. doi:10.1016/j.neuropsychologia.2008.09.015
Bloch MH, Landeros-Weisenberger A, Sen S, Dombrowski P, Kelmendi B, Coric V, Pittenger C, Leckman JF (2008) Association of the serotonin transporter polymorphism and obsessive-compulsive disorder: systematic review. Am J Med Genet B Neuropsychiatr Genet 147B(6):850–858. doi:10.1002/ajmg.b.30699
Bloch MH, Sukhodolsky DG, Dombrowski PA, Panza KE, Craiglow BG, Landeros-Weisenberger A, Leckman JF, Peterson BS, Schultz RT (2011) Poor fine-motor and visuospatial skills predict persistence of pediatric-onset obsessive-compulsive disorder into adulthood. J Child Psychol Psychiatry 52(9):974–983. doi:10.1111/j.1469-7610.2010.02366.x
Bloch MH, Wasylink S, Landeros-Weisenberger A, Panza KE, Billingslea E, Leckman JF, Krystal JH, Bhagwagar Z, Sanacora G, Pittenger C (2012) Effects of ketamine in treatment-refractory obsessive-compulsive disorder. Biol Psychiatry 72(11):964–970. doi:10.1016/j.biopsych.2012.05.028
Boonstra AM, Oosterlaan J, Sergeant JA, Buitelaar JK (2005) Executive functioning in adult ADHD: a meta-analytic review. Psychol Med 35(8):1097–1108
Botvinick M, Nystrom LE, Fissell K, Carter CS, Cohen JD (1999) Conflict monitoring versus selection-for-action in anterior cingulate cortex. Nature 402(6758):179–181. doi:10.1038/46035
Brandeis D, van Leeuwen TH, Rubia K, Vitacco D, Steger J, Pascual-Marqui RD, Steinhausen HC (1998) Neuroelectric mapping reveals precursor of stop failures in children with attention deficits. Behav Brain Res 94(1):111–125
Brem S, Hauser TU, Iannaccone R, Brandeis D, Drechsler R, Walitza S (2012) Neuroimaging of cognitive brain function in paediatric obsessive compulsive disorder: a review of literature and preliminary meta-analysis. J Neural Transm 119(11):1425–1448. doi:10.1007/s00702-012-0813-z
Bruno A, Mico U, Pandolfo G, Mallamace D, Abenavoli E, Di Nardo F, D’Arrigo C, Spina E, Zoccali RA, Muscatello MR (2012) Lamotrigine augmentation of serotonin reuptake inhibitors in treatment-resistant obsessive-compulsive disorder: a double-blind, placebo-controlled study. J Psychopharmacol 26(11):1456–1462. doi:10.1177/0269881111431751
Buot A, Welter ML, Karachi C, Pochon JB, Bardinet E, Yelnik J, Mallet L (2012) Processing of emotional information in the human subthalamic nucleus. J Neurol Neurosurg Psychiatry. doi:10.1136/jnnp-2011-302158
Burdick KE, Robinson DG, Malhotra AK, Szeszko PR (2008) Neurocognitive profile analysis in obsessive-compulsive disorder. J Int Neuropsychol Soc 14(4):640–645. doi:10.1017/S1355617708080727
Bush G, Frazier JA, Rauch SL, Seidman LJ, Whalen PJ, Jenike MA, Rosen BR, Biederman J (1999) Anterior cingulate cortex dysfunction in attention-deficit/hyperactivity disorder revealed by fMRI and the counting stroop. Biol Psychiatry 45(12):1542–1552
Bush G, Luu P, Posner MI (2000) Cognitive and emotional influences in anterior cingulate cortex. Trends Cogn Sci 4(6):215–222
Camarena B, Loyzaga C, Aguilar A, Weissbecker K, Nicolini H (2007) Association study between the dopamine receptor D(4) gene and obsessive-compulsive disorder. Eur Neuropsychopharmacol 17(6–7):406–409. doi:10.1016/j.euroneuro.2006.08.001
Carlson PJ, Singh JB, Zarate CA Jr, Drevets WC, Manji HK (2006) Neural circuitry and neuroplasticity in mood disorders: insights for novel therapeutic targets. NeuroRx 3(1):22–41. doi:10.1016/j.nurx.2005.12.009
Carlsson ML (2000) On the role of cortical glutamate in obsessive-compulsive disorder and attention-deficit hyperactivity disorder, two phenomenologically antithetical conditions. Acta Psychiatr Scand 102(6):401–413
Carlsson ML (2001) On the role of prefrontal cortex glutamate for the antithetical phenomenology of obsessive compulsive disorder and attention deficit hyperactivity disorder. Prog Neuropsychopharmacol Biol Psychiatry 25(1):5–26
Carrey N, Bernier D, Emms M, Gunde E, Sparkes S, Macmaster FP, Rusak B (2012) Smaller volumes of caudate nuclei in prepubertal children with ADHD: impact of age. J Psychiatr Res 46(8):1066–1072. doi:10.1016/j.jpsychires.2012.04.025
Carter CS, Macdonald AM, Botvinick M, Ross LL, Stenger VA, Noll D, Cohen JD (2000) Parsing executive processes: strategic vs. evaluative functions of the anterior cingulate cortex. Proc Natl Acad Sci USA 97(4):1944–1948
Castellanos FX, Giedd JN, Marsh WL, Hamburger SD, Vaituzis AC, Dickstein DP, Sarfatti SE, Vauss YC, Snell JW, Lange N, Kaysen D, Krain AL, Ritchie GF, Rajapakse JC, Rapoport JL (1996) Quantitative brain magnetic resonance imaging in attention-deficit hyperactivity disorder. Arch Gen Psychiatry 53(7):607–616
Castellanos FX, Lee PP, Sharp W, Jeffries NO, Greenstein DK, Clasen LS, Blumenthal JD, James RS, Ebens CL, Walter JM, Zijdenbos A, Evans AC, Giedd JN, Rapoport JL (2002) Developmental trajectories of brain volume abnormalities in children and adolescents with attention-deficit/hyperactivity disorder. JAMA: J Am Med Assoc 288(14):1740–1748
Cavedini P, Cisima M, Riboldi G, D’Annucci A, Bellodi L (2001) A neuropsychological study of dissociation in cortical and subcortical functioning in obsessive-compulsive disorder by tower of Hanoi task. Brain Cogn 46(3):357–363. doi:10.1006/brcg.2001.1293
Cavedini P, Riboldi G, D’Annucci A, Belotti P, Cisima M, Bellodi L (2002) Decision-making heterogeneity in obsessive-compulsive disorder: ventromedial prefrontal cortex function predicts different treatment outcomes. Neuropsychologia 40(2):205–211
Chamberlain SR, Fineberg NA, Blackwell AD, Robbins TW, Sahakian BJ (2006) Motor inhibition and cognitive flexibility in obsessive-compulsive disorder and trichotillomania. Am J Psychiatry 163(7):1282–1284. doi:10.1176/appi.ajp.163.7.1282
Chamberlain SR, Fineberg NA, Blackwell AD, Clark L, Robbins TW, Sahakian BJ (2007) A neuropsychological comparison of obsessive-compulsive disorder and trichotillomania. Neuropsychologia 45(4):654–662. doi:10.1016/j.neuropsychologia.2006.07.016
Chamberlain SR, Menzies L, Hampshire A, Suckling J, Fineberg NA, del Campo N, Aitken M, Craig K, Owen AM, Bullmore ET, Robbins TW, Sahakian BJ (2008) Orbitofrontal dysfunction in patients with obsessive-compulsive disorder and their unaffected relatives. Science 321(5887):421–422. doi:10.1126/science.1154433
Chang SW, McCracken JT, Piacentini JC (2007) Neurocognitive correlates of child obsessive compulsive disorder and Tourette syndrome. J Clin Exp Neuropsychol 29(7):724–733. doi:10.1080/13825580600966383
Charney DS, Goodman WK, Price LH, Woods SW, Rasmussen SA, Heninger GR (1988) Serotonin function in obsessive-compulsive disorder. A comparison of the effects of tryptophan and m-chlorophenylpiperazine in patients and healthy subjects. Arch Gen Psychiatry 45(2):177–185
Congdon E, Constable RT, Lesch KP, Canli T (2009) Influence of SLC6A3 and COMT variation on neural activation during response inhibition. Biol Psychol 81(3):144–152. doi:10.1016/j.biopsycho.2009.03.005
Cortese S, Kelly C, Chabernaud C, Proal E, Di Martino A, Milham MP, Castellanos FX (2012) Toward systems neuroscience of ADHD: a meta-analysis of 55 fMRI studies. Am J Psychiatry 169(10):1038–1055. doi:10.1176/appi.ajp.2012.11101521
Costa A, Riedel M, Muller U, Moller HJ, Ettinger U (2011) Relationship between SLC6A3 genotype and striatal dopamine transporter availability: a meta-analysis of human single photon emission computed tomography studies. Synapse 65(10):998–1005. doi:10.1002/syn.20927
Cox C, Fedio P, Rapoport J (1989) Neuropsychological testing of obsessive-compulsive adolescents. In: Rapoport J (ed) Obsessive-compulsive disorder in children and adolescents. American Psychiatric Press, Washington, pp 73–85
Crossman AR, Mitchell IJ, Sambrook MA (1985) Regional brain uptake of 2-deoxyglucose in N-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP)-induced parkinsonism in the macaque monkey. Neuropharmacology 24(6):587–591
Crutcher MD, DeLong MR (1984) Single cell studies of the primate putamen I Functional organization. Exp Brain Res 53(2):233–243
Cruz C, Camarena B, King N, Paez F, Sidenberg D, de la Fuente JR, Nicolini H (1997) Increased prevalence of the seven-repeat variant of the dopamine D4 receptor gene in patients with obsessive-compulsive disorder with tics. Neurosci Lett 231(1):1–4
Cummings JL (1995) Anatomic and behavioral aspects of frontal-subcortical circuits. Ann N Y Acad Sci 769:1–13
da Rocha FF, Malloy-Diniz L, Lage NV, Romano-Silva MA, de Marco LA, Correa H (2008) Decision-making impairment is related to serotonin transporter promoter polymorphism in a sample of patients with obsessive-compulsive disorder. Behav Brain Res 195(1):159–163. doi:10.1016/j.bbr.2008.05.015
da Rocha FF, Alvarenga NB, Malloy-Diniz L, Correa H (2011) Decision-making impairment in obsessive-compulsive disorder as measured by the Iowa gambling task. Arq Neuropsiquiatr 69(4):642–647
Dalley JW, Roiser JP (2012) Dopamine, serotonin and impulsivity. Neuroscience 215:42–58. doi:10.1016/j.neuroscience.2012.03.065
DeLong MR, Crutcher MD, Georgopoulos AP (1985) Primate globus pallidus and subthalamic nucleus: functional organization. J Neurophysiol 53(2):530–543
Delorme R, Golmard JL, Chabane N, Millet B, Krebs MO, Mouren-Simeoni MC, Leboyer M (2005) Admixture analysis of age at onset in obsessive-compulsive disorder. Psychol Med 35(2):237–243
Di Russo F, Zaccara G, Ragazzoni A, Pallanti S (2000) Abnormal visual event-related potentials in obsessive-compulsive disorder without panic disorder or depression comorbidity. J Psychiatr Res 34(1):75–82
Dimoska A, Johnstone SJ, Barry RJ, Clarke AR (2003) Inhibitory motor control in children with attention-deficit/hyperactivity disorder: event-related potentials in the stop-signal paradigm. Biol Psychiatry 54(12):1345–1354
Dittrich WH, Johansen T (2013) Cognitive deficits of executive functions and decision-making in obsessive-compulsive disorder. Scand J Psychol 54(5):393–400. doi:10.1111/sjop.12066
do Rosario-Campos MC, Leckman JF, Curi M, Quatrano S, Katsovitch L, Miguel EC, Pauls DL (2005) A family study of early-onset obsessive-compulsive disorder. Am J Med Genet B Neuropsychiatr Genet 136B(1):92–97. doi:10.1002/ajmg.b.30149
Donkers FC, van Boxtel GJ (2004) The N2 in go/no-go tasks reflects conflict monitoring not response inhibition. Brain Cogn 56(2):165–176. doi:10.1016/j.bandc.2004.04.005
Durston S, Davidson MC, Thomas KM, Worden MS, Tottenham N, Martinez A, Watts R, Ulug AM, Casey BJ (2003a) Parametric manipulation of conflict and response competition using rapid mixed-trial event-related fMRI. NeuroImage 20(4):2135–2141
Durston S, Tottenham NT, Thomas KM, Davidson MC, Eigsti IM, Yang Y, Ulug AM, Casey BJ (2003b) Differential patterns of striatal activation in young children with and without ADHD. Biol Psychiatry 53(10):871–878
Ellison-Wright I, Ellison-Wright Z, Bullmore E (2008) Structural brain change in attention deficit hyperactivity disorder identified by meta-analysis. BMC psychiatry 8:51. doi:10.1186/1471-244X-8-51
Endrass T, Klawohn J, Schuster F, Kathmann N (2008) Overactive performance monitoring in obsessive-compulsive disorder: ERP evidence from correct and erroneous reactions. Neuropsychologia 46(7):1877–1887. doi:10.1016/j.neuropsychologia.2007.12.001
Endrass T, Kloft L, Kaufmann C, Kathmann N (2011) Approach and avoidance learning in obsessive-compulsive disorder. Depress Anxiety 28(2):166–172. doi:10.1002/da.20772
Enriquez-Geppert S, Konrad C, Pantev C, Huster RJ (2010) Conflict and inhibition differentially affect the N200/P300 complex in a combined go/nogo and stop-signal task. NeuroImage 51(2):877–887. doi:10.1016/j.neuroimage.2010.02.043
Exner C, Kohl A, Zaudig M, Langs G, Lincoln TM, Rief W (2009) Metacognition and episodic memory in obsessive-compulsive disorder. J Anxiety Disord 23(5):624–631. doi:10.1016/j.janxdis.2009.01.010
Falkenstein M, Hoormann J, Hohnsbein J (1999) ERP components in Go/Nogo tasks and their relation to inhibition. Acta Psychol 101(2–3):267–291
Fallgatter AJ, Strik WK (1999) The NoGo-anteriorization as a neurophysiological standard-index for cognitive response control. Int J Psychophysiol 32(3):233–238
Fallgatter AJ, Ehlis AC, Seifert J, Strik WK, Scheuerpflug P, Zillessen KE, Herrmann MJ, Warnke A (2004) Altered response control and anterior cingulate function in attention-deficit/hyperactivity disorder boys. Clin Neurophysiol 115(4):973–981. doi:10.1016/j.clinph.2003.11.036
Fallgatter AJ, Ehlis AC, Rosler M, Strik WK, Blocher D, Herrmann MJ (2005) Diminished prefrontal brain function in adults with psychopathology in childhood related to attention deficit hyperactivity disorder. Psychiatry Res 138(2):157–169. doi:10.1016/j.pscychresns.2004.12.002
Faraone SV, Khan SA (2006) Candidate gene studies of attention-deficit/hyperactivity disorder. J Clin Psychiatry 67(Suppl 8):13–20
Faraone SV, Perlis RH, Doyle AE, Smoller JW, Goralnick JJ, Holmgren MA, Sklar P (2005) Molecular genetics of attention-deficit/hyperactivity disorder. Biol Psychiatry 57(11):1313–1323. doi:10.1016/j.biopsych.2004.11.024
Fayyad J, De Graaf R, Kessler R, Alonso J, Angermeyer M, Demyttenaere K, De Girolamo G, Haro JM, Karam EG, Lara C, Lepine JP, Ormel J, Posada-Villa J, Zaslavsky AM, Jin R (2007) Cross-national prevalence and correlates of adult attention-deficit hyperactivity disorder. Br J Psychiatry 190:402–409. doi:10.1192/bjp.bp.106.034389
Ferguson HB, Pappas BA, Trites RL, Peters DA, Taub H (1981) Plasma free and total tryptophan, blood serotonin, and the hyperactivity syndrome: no evidence for the serotonin deficiency hypothesis. Biol Psychiatry 16(3):231–238
Fineberg NA, Potenza MN, Chamberlain SR, Berlin HA, Menzies L, Bechara A, Sahakian BJ, Robbins TW, Bullmore ET, Hollander E (2010) Probing compulsive and impulsive behaviors, from animal models to endophenotypes: a narrative review. Neuropsychopharmacology 35(3):591–604. doi:10.1038/npp.2009.185
Flament MF, Whitaker A, Rapoport JL, Davies M, Berg CZ, Kalikow K, Sceery W, Shaffer D (1988) Obsessive compulsive disorder in adolescence: an epidemiological study. J Am Acad Child Adolesc Psychiatry 27(6):764–771. doi:10.1097/00004583-198811000-00018
Forero DA, Arboleda GH, Vasquez R, Arboleda H (2009) Candidate genes involved in neural plasticity and the risk for attention-deficit hyperactivity disorder: a meta-analysis of 8 common variants. J Psychiatry Neurosci 34(5):361–366
Franke B, Vasquez AA, Johansson S, Hoogman M, Romanos J, Boreatti-Hummer A, Heine M, Jacob CP, Lesch KP, Casas M, Ribases M, Bosch R, Sanchez-Mora C, Gomez-Barros N, Fernandez-Castillo N, Bayes M, Halmoy A, Halleland H, Landaas ET, Fasmer OB, Knappskog PM, Heister AJ, Kiemeney LA, Kooij JJ, Boonstra AM, Kan CC, Asherson P, Faraone SV, Buitelaar JK, Haavik J, Cormand B, Ramos-Quiroga JA, Reif A (2010) Multicenter analysis of the SLC6A3/DAT1 VNTR haplotype in persistent ADHD suggests differential involvement of the gene in childhood and persistent ADHD. Neuropsychopharmacology 35(3):656–664. doi:10.1038/npp.2009.170
Franke B, Faraone SV, Asherson P, Buitelaar J, Bau CH, Ramos-Quiroga JA, Mick E, Grevet EH, Johansson S, Haavik J, Lesch KP, Cormand B, Reif A, International Multicentre persistent AC (2012) The genetics of attention deficit/hyperactivity disorder in adults, a review. Mol Psychiatry 17(10):960–987. doi:10.1038/mp.2011.138
Freitag CM, Rohde LA, Lempp T, Romanos M (2010) Phenotypic and measurement influences on heritability estimates in childhood ADHD. Eur Child Adolesc Psychiatry 19(3):311–323. doi:10.1007/s00787-010-0097-5
Friedel S, Saar K, Sauer S, Dempfle A, Walitza S, Renner T, Romanos M, Freitag C, Seitz C, Palmason H, Scherag A, Windemuth-Kieselbach C, Schimmelmann BG, Wewetzer C, Meyer J, Warnke A, Lesch KP, Reinhardt R, Herpertz-Dahlmann B, Linder M, Hinney A, Remschmidt H, Schafer H, Konrad K, Hubner N, Hebebrand J (2007) Association and linkage of allelic variants of the dopamine transporter gene in ADHD. Mol Psychiatry 12(10):923–933. doi:10.1038/sj.mp.4001986
Friedlander L, Desrocher M (2006) Neuroimaging studies of obsessive-compulsive disorder in adults and children. Clin Psychol Rev 26(1):32–49. doi:10.1016/j.cpr.2005.06.010
Frodl T, Skokauskas N (2012) Meta-analysis of structural MRI studies in children and adults with attention deficit hyperactivity disorder indicates treatment effects. Acta Psychiatr Scand 125(2):114–126. doi:10.1111/j.1600-0447.2011.01786.x
Fullana MA, Vilagut G, Mataix-Cols D, Adroher ND, Bruffaerts R, Bunting B, de Almeida JM, Florescu S, de Girolamo G, de Graaf R, Haro JM, Kovess V, Alonso J (2013) Is ADHD in childhood associated with lifetime hoarding symptoms? An epidemiological study. Depress Anxiety 30(8):741–748. doi:10.1002/da.22123
Furth KE, Mastwal S, Wang KH, Buonanno A, Vullhorst D (2013) Dopamine, cognitive function, and gamma oscillations: role of D4 receptors. Front Cell Neurosci 7:102. doi:10.3389/fncel.2013.00102
Gallagher JJ, Zhang X, Hall FS, Uhl GR, Bearer EL, Jacobs RE (2013) Altered reward circuitry in the norepinephrine transporter knockout mouse. PLoS ONE 8(3):e57597. doi:10.1371/journal.pone.0057597
Galvez JM, Forero DA, Fonseca DJ, Mateus HE, Talero-Gutierrez C, Velez-van-Meerbeke A (2013) Evidence of association between SNAP25 gene and attention deficit hyperactivity disorder in a Latin American sample. Atten Defic Hyperact Disord. doi:10.1007/s12402-013-0123-9
Geburek AJ, Rist F, Gediga G, Stroux D, Pedersen A (2013) Electrophysiological indices of error monitoring in juvenile and adult attention deficit hyperactivity disorder (ADHD)—a meta-analytic appraisal. Int J Psychophysiol 87(3):349–362. doi:10.1016/j.ijpsycho.2012.08.006
Geller D, Biederman J, Faraone SV, Frazier J, Coffey BJ, Kim G, Bellordre CA (2000) Clinical correlates of obsessive compulsive disorder in children and adolescents referred to specialized and non-specialized clinical settings. Depress Anxiety 11(4):163–168. doi:10.1002/1520-6394(2000)11:4<163:AID-DA3>3.0.CO;2-3
Geller DA, Biederman J, Faraone S, Agranat A, Cradock K, Hagermoser L, Kim G, Frazier J, Coffey BJ (2001) Developmental aspects of obsessive compulsive disorder: findings in children, adolescents, and adults. J Nerv Ment Dis 189(7):471–477
Geller D, Petty C, Vivas F, Johnson J, Pauls D, Biederman J (2007a) Examining the relationship between obsessive-compulsive disorder and attention-deficit/hyperactivity disorder in children and adolescents: a familial risk analysis. Biol Psychiatry 61(3):316–321. doi:10.1016/j.biopsych.2006.03.083
Geller D, Petty C, Vivas F, Johnson J, Pauls D, Biederman J (2007b) Further evidence for co-segregation between pediatric obsessive compulsive disorder and attention deficit hyperactivity disorder: a familial risk analysis. Biol Psychiatry 61(12):1388–1394. doi:10.1016/j.biopsych.2006.09.026
Ghaleiha A, Entezari N, Modabbernia A, Najand B, Askari N, Tabrizi M, Ashrafi M, Hajiaghaee R, Akhondzadeh S (2013) Memantine add-on in moderate to severe obsessive-compulsive disorder: randomized double-blind placebo-controlled study. J Psychiatr Res 47(2):175–180. doi:10.1016/j.jpsychires.2012.09.015
Giedd JN, Castellanos FX, Casey BJ, Kozuch P, King AC, Hamburger SD, Rapoport JL (1994) Quantitative morphology of the corpus callosum in attention deficit hyperactivity disorder. Am J Psychiatry 151(5):665–669
Gizer IR, Ficks C, Waldman ID (2009) Candidate gene studies of ADHD: a meta-analytic review. Hum Genet 126(1):51–90. doi:10.1007/s00439-009-0694-x
Goldman BL, Martin ED, Calamari JE, Woodard JL, Chik HM, Messina MG, Pontarelli NK, Marker CD, Riemann BC, Wiegartz PS (2008) Implicit learning, thought-focused attention and obsessive-compulsive disorder: a replication and extension. Behav Res Ther 46(1):48–61. doi:10.1016/j.brat.2007.10.004
Gonçalves ÓF, Carvalho S, Leite J, Pocinho F, Relvas J, Fregni F (2011) Obsessive Compulsive Disorder as a functional interhemispheric imbalance at the thalamic level. Med Hypotheses 77(3):445–447. doi:10.1016/j.mehy.2011.06.004
Grabemann M, Mette C, Zimmermann M, Heinrich V, Uekermann J, Wiltfang J, Abdel-Hamid M, Zepf FD, Kis B (2013) No clear effects of acute tryptophan depletion on processing affective prosody in male adults with ADHD. Acta Psychiatr Scand 128(2):142–148. doi:10.1111/acps.12130
Greenberg WM, Benedict MM, Doerfer J, Perrin M, Panek L, Cleveland WL, Javitt DC (2009) Adjunctive glycine in the treatment of obsessive-compulsive disorder in adults. J Psychiatr Res 43(6):664–670. doi:10.1016/j.jpsychires.2008.10.007
Greimel E, Wanderer S, Rothenberger A, Herpertz-Dahlmann B, Konrad K, Roessner V (2011) Attentional performance in children and adolescents with tic disorder and co-occurring attention-deficit/hyperactivity disorder: new insights from a 2 × 2 factorial design study. J Abnorm Child Psychol 39(6):819–828. doi:10.1007/s10802-011-9493-7
Groen Y, Wijers AA, Mulder LJ, Waggeveld B, Minderaa RB, Althaus M (2008) Error and feedback processing in children with ADHD and children with Autistic Spectrum Disorder: an EEG event-related potential study. Clin Neurophysiol 119(11):2476–2493. doi:10.1016/j.clinph.2008.08.004
Grundler TO, Cavanagh JF, Figueroa CM, Frank MJ, Allen JJ (2009) Task-related dissociation in ERN amplitude as a function of obsessive-compulsive symptoms. Neuropsychologia 47(8–9):1978–1987. doi:10.1016/j.neuropsychologia.2009.03.010
Gu BM, Park JY, Kang DH, Lee SJ, Yoo SY, Jo HJ, Choi CH, Lee JM, Kwon JS (2008) Neural correlates of cognitive inflexibility during task-switching in obsessive-compulsive disorder. J Neurol 131(Pt 1):155–164. doi:10.1093/brain/awm277
Hajcak G, Franklin ME, Foa EB, Simons RF (2008) Increased error-related brain activity in pediatric obsessive-compulsive disorder before and after treatment. Am J Psychiatry 165(1):116–123. doi:10.1176/appi.ajp.2007.07010143
Hanna GL, Veenstra-VanderWeele J, Cox NJ, Boehnke M, Himle JA, Curtis GC, Leventhal BL, Cook EH Jr (2002) Genome-wide linkage analysis of families with obsessive-compulsive disorder ascertained through pediatric probands. Am J Med Genet 114(5):541–552. doi:10.1002/ajmg.10519
Hanna GL, Fischer DJ, Chadha KR, Himle JA, Van Etten M (2005a) Familial and sporadic subtypes of early-onset obsessive-compulsive disorder. Biol Psychiatry 57(8):895–900. doi:10.1016/j.biopsych.2004.12.022
Hanna GL, Himle JA, Curtis GC, Gillespie BW (2005b) A family study of obsessive-compulsive disorder with pediatric probands. Am J Med Genet B Neuropsychiatr Genet 134B(1):13–19. doi:10.1002/ajmg.b.30138
Hanna GL, Veenstra-Vanderweele J, Cox NJ, Van Etten M, Fischer DJ, Himle JA, Bivens NC, Wu X, Roe CA, Hennessy KA, Dickel DE, Leventhal BL, Cook EH Jr (2007) Evidence for a susceptibility locus on chromosome 10p15 in early-onset obsessive-compulsive disorder. Biol Psychiatry 62(8):856–862. doi:10.1016/j.biopsych.2007.01.008
Harkin B, Kessler K (2011) The role of working memory in compulsive checking and OCD: a systematic classification of 58 experimental findings. Clin Psychol Rev 31(6):1004–1021. doi:10.1016/j.cpr.2011.06.004
Hashimoto N, Nakaaki S, Omori IM, Fujioi J, Noguchi Y, Murata Y, Sato J, Tatsumi H, Torii K, Mimura M, Furukawa TA (2011) Distinct neuropsychological profiles of three major symptom dimensions in obsessive-compulsive disorder. Psychiatry Res 187(1–2):166–173. doi:10.1016/j.psychres.2010.08.001
Haslam RH, Dalby JT (1983) Blood serotonin levels in the attention-deficit disorder. N Engl J Med 309(21):1328–1329
Hawi Z, Matthews N, Wagner J, Wallace RH, Butler TJ, Vance A, Kent L, Gill M, Bellgrove MA (2013) DNA variation in the SNAP25 gene confers risk to ADHD and is associated with reduced expression in prefrontal cortex. PLoS ONE 8(4):e60274. doi:10.1371/journal.pone.0060274
Hebebrand J, Dempfle A, Saar K, Thiele H, Herpertz-Dahlmann B, Linder M, Kiefl H, Remschmidt H, Hemminger U, Warnke A, Knolker U, Heiser P, Friedel S, Hinney A, Schafer H, Nurnberg P, Konrad K (2006) A genome-wide scan for attention-deficit/hyperactivity disorder in 155 German sib-pairs. Mol Psychiatry 11(2):196–205. doi:10.1038/sj.mp.4001761
Heils A, Teufel A, Petri S, Stober G, Riederer P, Bengel D, Lesch KP (1996) Allelic variation of human serotonin transporter gene expression. J Neurochem 66(6):2621–2624
Hemmings SM, Kinnear CJ, Lochner C, Niehaus DJ, Knowles JA, Moolman-Smook JC, Corfield VA, Stein DJ (2004) Early- versus late-onset obsessive-compulsive disorder: investigating genetic and clinical correlates. Psychiatr Res 128(2):175–182. doi:10.1016/j.psychres.2004.05.007
Hermans D, Engelen U, Grouwels L, Joos E, Lemmens J, Pieters G (2008) Cognitive confidence in obsessive-compulsive disorder: distrusting perception, attention and memory. Behav Res Ther 46(1):98–113. doi:10.1016/j.brat.2007.11.001
Herrmann MJ, Jacob C, Unterecker S, Fallgatter AJ (2003) Reduced response-inhibition in obsessive-compulsive disorder measured with topographic evoked potential mapping. Psychiatr Res 120(3):265–271
Hezel DM, Beattie K, Stewart SE (2009) Memantine as an augmenting agent for severe pediatric OCD. Am J Psychiatry 166(2):237. doi:10.1176/appi.ajp.2008.08091427
Hill DE, Yeo RA, Campbell RA, Hart B, Vigil J, Brooks W (2003) Magnetic resonance imaging correlates of attention-deficit/hyperactivity disorder in children. Neuropsychology 17(3):496–506
Hoerst M, Weber-Fahr W, Tunc-Skarka N, Ruf M, Bohus M, Schmahl C, Ende G (2010) Correlation of glutamate levels in the anterior cingulate cortex with self-reported impulsivity in patients with borderline personality disorder and healthy controls. Arch Gen Psychiatry 67(9):946–954. doi:10.1001/archgenpsychiatry.2010.93
Holroyd CB, Coles MG (2002) The neural basis of human error processing: reinforcement learning, dopamine, and the error-related negativity. Psychol Rev 109(4):679–709
Hoshino Y, Ohno Y, Yamamoto T, Kaneko M, Kumashiro H (1985) Plasma free tryptophan concentration in children with attention deficit disorder. Folia Psychiatr Neurol Jpn 39(4):531–535
Hoza B, Pelham WE Jr, Dobbs J, Owens JS, Pillow DR (2002) Do boys with attention-deficit/hyperactivity disorder have positive illusory self-concepts? J Abnorm Psychol 111(2):268–278
Huang-Pollock CL, Karalunas SL, Tam H, Moore AN (2012) Evaluating vigilance deficits in ADHD: a meta-analysis of CPT performance. J Abnorm Psychol 121(2):360–371. doi:10.1037/a0027205
Huey ED, Zahn R, Krueger F, Moll J, Kapogiannis D, Wassermann EM, Grafman J (2008) A psychological and neuroanatomical model of obsessive-compulsive disorder. J Neuropsychiatry Clin Neurosci 20(4):390–408. doi:10.1176/appi.neuropsych.20.4.390
Hunt RD, Cohen DJ, Shaywitz SE, Shaywitz BA (1982) Strategies for study of the neurochemistry of attention deficit disorder in children. Schizophr Bull 8(2):236–252
Insel TR, Mueller EA, Alterman I, Linnoila M, Murphy DL (1985) Obsessive-compulsive disorder and serotonin: is there a connection? Biol Psychiatry 20(11):1174–1188
Irwin M, Belendiuk K, McCloskey K, Freedman DX (1981) Tryptophan metabolism in children with attentional deficit disorder. Am J Psychiatry 138(8):1082–1085
Jang JH, Kim HS, Ha TH, Shin NY, Kang DH, Choi JS, Ha K, Kwon JS (2010) Nonverbal memory and organizational dysfunctions are related with distinct symptom dimensions in obsessive-compulsive disorder. Psychiatr Res 180(2–3):93–98. doi:10.1016/j.psychres.2010.04.016
Jenike MA, Breiter HC, Baer L, Kennedy DN, Savage CR, Olivares MJ, O’Sullivan RL, Shera DM, Rauch SL, Keuthen N, Rosen BR, Caviness VS, Filipek PA (1996) Cerebral structural abnormalities in obsessive-compulsive disorder. A quantitative morphometric magnetic resonance imaging study. Arch Gen Psychiatry 53(7):625–632
Jiang Y, Johnston C (2012) The relationship between ADHD symptoms and competence as reported by both self and others. J Atten Disord 16(5):418–426. doi:10.1177/1087054710392541
Johannes S, Wieringa BM, Nager W, Rada D, Dengler R, Emrich HM, Munte TF, Dietrich DE (2001) Discrepant target detection and action monitoring in obsessive-compulsive disorder. Psychiatr Res 108(2):101–110
Kantojarvi K, Onkamo P, Vanhala R, Alen R, Hedman M, Sajantila A, Nieminen-von Wendt T, Jarvela I (2010) Analysis of 9p24 and 11p12-13 regions in autism spectrum disorders: rs1340513 in the JMJD2C gene is associated with ASDs in Finnish sample. Psychiatr Genet 20(3):102–108. doi:10.1097/YPG.0b013e32833a2080
Kasper LJ, Alderson RM, Hudec KL (2012) Moderators of working memory deficits in children with attention-deficit/hyperactivity disorder (ADHD): a meta-analytic review. Clin Psychol Rev 32(7):605–617. doi:10.1016/j.cpr.2012.07.001
Kathmann N, Rupertseder C, Hauke W, Zaudig M (2005) Implicit sequence learning in obsessive-compulsive disorder: further support for the fronto-striatal dysfunction model. Biol Psychiatry 58(3):239–244. doi:10.1016/j.biopsych.2005.03.045
Kessler RC, Adler LA, Barkley R, Biederman J, Conners CK, Faraone SV, Greenhill LL, Jaeger S, Secnik K, Spencer T, Ustun TB, Zaslavsky AM (2005) Patterns and predictors of attention-deficit/hyperactivity disorder persistence into adulthood: results from the national comorbidity survey replication. Biol Psychiatry 57(11):1442–1451. doi:10.1016/j.biopsych.2005.04.001
Kessler RC, Adler L, Barkley R, Biederman J, Conners CK, Demler O, Faraone SV, Greenhill LL, Howes MJ, Secnik K, Spencer T, Ustun TB, Walters EE, Zaslavsky AM (2006) The prevalence and correlates of adult ADHD in the United States: results from the national comorbidity survey replication. Am J Psychiatry 163(4):716–723. doi:10.1176/appi.ajp.163.4.716
Kikul J, Vetter J, Lincoln TM, Exner C (2011) Effects of cognitive self-consciousness on visual memory in obsessive-compulsive disorder. J Anxiety Disord 25(4):490–497. doi:10.1016/j.janxdis.2010.12.002
Kim MS, Kim YY, Yoo SY, Kwon JS (2007) Electrophysiological correlates of behavioral response inhibition in patients with obsessive-compulsive disorder. Depress Anxiety 24(1):22–31. doi:10.1002/da.20195
Knouse LE, Bagwell CL, Barkley RA, Murphy KR (2005) Accuracy of self-evaluation in adults with ADHD: evidence from a driving study. J Atten Disord 8(4):221–234. doi:10.1177/1087054705280159
Kodaira M, Iwadare Y, Ushijima H, Oiji A, Kato M, Sugiyama N, Sasayama D, Usami M, Watanabe K, Saito K (2012) Poor performance on the Iowa gambling task in children with obsessive-compulsive disorder. Ann Gen Psychiatry 11(1):25. doi:10.1186/1744-859X-11-25
Kofler MJ, Rapport MD, Sarver DE, Raiker JS, Orban SA, Friedman LM, Kolomeyer EG (2013) Reaction time variability in ADHD: a meta-analytic review of 319 studies. Clin Psychol Rev 33(6):795–811. doi:10.1016/j.cpr.2013.06.001
Komossa K, Depping AM, Meyer M, Kissling W, Leucht S (2010) Second-generation antipsychotics for obsessive compulsive disorder. Cochrane Database Syst Rev (12):CD008141. doi:10.1002/14651858.CD008141.pub2
Konrad K, Neufang S, Hanisch C, Fink GR, Herpertz-Dahlmann B (2006) Dysfunctional attentional networks in children with attention deficit/hyperactivity disorder: evidence from an event-related functional magnetic resonance imaging study. Biol Psychiatry 59(7):643–651. doi:10.1016/j.biopsych.2005.08.013
Koo MS, Kim EJ, Roh D, Kim CH (2010) Role of dopamine in the pathophysiology and treatment of obsessive-compulsive disorder. Expert Rev Neurother 10(2):275–290. doi:10.1586/ern.09.148
Kopp B, Mattler U, Goertz R, Rist F (1996) N2, P3 and the lateralized readiness potential in a nogo task involving selective response priming. Electroencephalogr Clin Neurophysiol 99(1):19–27
Kotting WF, Bubenzer S, Helmbold K, Eisert A, Gaber TJ, Zepf FD (2013) Effects of tryptophan depletion on reactive aggression and aggressive decision-making in young people with ADHD. Acta Psychiatr Scand 128(2):114–123. doi:10.1111/acps.12001
Lambek R, Tannock R, Dalsgaard S, Trillingsgaard A, Damm D, Thomsen PH (2011) Executive dysfunction in school-age children with ADHD. J Atten Disord 15(8):646–655. doi:10.1177/1087054710370935
Lander E, Kruglyak L (1995) Genetic dissection of complex traits: guidelines for interpreting and reporting linkage results. Nat Genet 11(3):241–247. doi:10.1038/ng1195-241
Lansbergen MM, Kenemans JL, van Engeland H (2007) Stroop interference and attention-deficit/hyperactivity disorder: a review and meta-analysis. Neuropsychology 21(2):251–262. doi:10.1037/0894-4105.21.2.251
Larsson H, Anckarsater H, Rastam M, Chang Z, Lichtenstein P (2012) Childhood attention-deficit hyperactivity disorder as an extreme of a continuous trait: a quantitative genetic study of 8,500 twin pairs. J Child Psychol Psychiatry 53(1):73–80. doi:10.1111/j.1469-7610.2011.02467.x
Larsson H, Asherson P, Chang Z, Ljung T, Friedrichs B, Larsson JO, Lichtenstein P (2013) Genetic and environmental influences on adult attention deficit hyperactivity disorder symptoms: a large Swedish population-based study of twins. Psychol Med 43(1):197–207. doi:10.1017/S0033291712001067
Lasky-Su J, Neale BM, Franke B, Anney RJ, Zhou K, Maller JB, Vasquez AA, Chen W, Asherson P, Buitelaar J, Banaschewski T, Ebstein R, Gill M, Miranda A, Mulas F, Oades RD, Roeyers H, Rothenberger A, Sergeant J, Sonuga-Barke E, Steinhausen HC, Taylor E, Daly M, Laird N, Lange C, Faraone SV (2008) Genome-wide association scan of quantitative traits for attention deficit hyperactivity disorder identifies novel associations and confirms candidate gene associations. Am J Med Genet B Neuropsychiatr Genet 147B(8):1345–1354. doi:10.1002/ajmg.b.30867
Lawrence NS, Wooderson S, Mataix-Cols D, David R, Speckens A, Phillips ML (2006) Decision making and set shifting impairments are associated with distinct symptom dimensions in obsessive-compulsive disorder. Neuropsychology 20(4):409–419. doi:10.1037/0894-4105.20.4.409
Leckman JF, Goodman WK, Anderson GM, Riddle MA, Chappell PB, McSwiggan-Hardin MT, McDougle CJ, Scahill LD, Ort SI, Pauls DL et al (1995) Cerebrospinal fluid biogenic amines in obsessive compulsive disorder, Tourette’s syndrome, and healthy controls. Neuropsychopharmacology 12(1):73–86. doi:10.1016/0893-133X(94)00070-G
Lesch KP, Bengel D, Heils A, Sabol SZ, Greenberg BD, Petri S, Benjamin J, Muller CR, Hamer DH, Murphy DL (1996) Association of anxiety-related traits with a polymorphism in the serotonin transporter gene regulatory region. Science 274(5292):1527–1531
Lesch KP, Timmesfeld N, Renner TJ, Halperin R, Roser C, Nguyen TT, Craig DW, Romanos J, Heine M, Meyer J, Freitag C, Warnke A, Romanos M, Schafer H, Walitza S, Reif A, Stephan DA, Jacob C (2008) Molecular genetics of adult ADHD: converging evidence from genome-wide association and extended pedigree linkage studies. J Neural Transm 115(11):1573–1585. doi:10.1007/s00702-008-0119-3
Liotti M, Pliszka SR, Perez R, Kothmann D, Woldorff MG (2005) Abnormal brain activity related to performance monitoring and error detection in children with ADHD. Cortex 41(3):377–388
Lipszyc J, Schachar R (2010) Inhibitory control and psychopathology: a meta-analysis of studies using the stop signal task. J Int Neuropsychol Soc 16(6):1064–1076. doi:10.1017/S1355617710000895
Loo SK, Humphrey LA, Tapio T, Moilanen IK, McGough JJ, McCracken JT, Yang MH, Dang J, Taanila A, Ebeling H, Jarvelin MR, Smalley SL (2007) Executive functioning among Finnish adolescents with attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 46(12):1594–1604. doi:10.1097/chi.0b013e3181575014
Luman M, Tripp G, Scheres A (2010) Identifying the neurobiology of altered reinforcement sensitivity in ADHD: a review and research agenda. Neurosci Biobehav Rev 34(5):744–754. doi:10.1016/j.neubiorev.2009.11.021
Luxenberg JS, Swedo SE, Flament MF, Friedland RP, Rapoport J, Rapoport SI (1988) Neuroanatomical abnormalities in obsessive-compulsive disorder detected with quantitative X-ray computed tomography. Am J Psychiatry 145(9):1089–1093
Mahone EM, Crocetti D, Ranta ME, Gaddis A, Cataldo M, Slifer KJ, Denckla MB, Mostofsky SH (2011) A preliminary neuroimaging study of preschool children with ADHD. Clin Neuropsychol 25(6):1009–1028. doi:10.1080/13854046.2011.580784
Malloy P, Rasmussen S, Braden W, Haier RJ (1989) Topographic evoked potential mapping in obsessive-compulsive disorder: evidence of frontal lobe dysfunction. Psychiatry Res 28(1):63–71
Maltby N, Tolin DF, Worhunsky P, O’Keefe TM, Kiehl KA (2005) Dysfunctional action monitoring hyperactivates frontal-striatal circuits in obsessive-compulsive disorder: an event-related fMRI study. NeuroImage 24(2):495–503. doi:10.1016/j.neuroimage.2004.08.041
Marazziti D, Baroni S, Palego L, Masala I, Consoli G, Catena Dell’osso M, Giannaccini G, Lucacchini A (2009) Adenylate-cyclase activity in platelets of patients with obsessive-compulsive disorder. Neuropsychiatr Dis Treat 5:363–367
March JS, Gutzman LD, Jefferson JW, Greist JH (1989) Serotonin and treatment in obsessive-compulsive disorder. Psychiatr Dev 7(1):1–18
Masi G, Millepiedi S, Mucci M, Bertini N, Pfanner C, Arcangeli F (2006) Comorbidity of obsessive-compulsive disorder and attention-deficit/hyperactivity disorder in referred children and adolescents. Compr Psychiatry 47(1):42–47. doi:10.1016/j.comppsych.2005.04.008
Masi G, Millepiedi S, Perugi G, Pfanner C, Berloffa S, Pari C, Mucci M, Akiskal HS (2010) A naturalistic exploratory study of the impact of demographic, phenotypic and comorbid features in pediatric obsessive-compulsive disorder. Psychopathology 43(2):69–78. doi:10.1159/000274175
Mataix-Cols D, Alonso P, Pifarre J, Menchon JM, Vallejo J (2002) Neuropsychological performance in medicated vs. unmedicated patients with obsessive-compulsive disorder. Psychiatr Res 109(3):255–264
Mataix-Cols D, Rosario-Campos MC, Leckman JF (2005) A multidimensional model of obsessive-compulsive disorder. Am J Psychiatry 162(2):228–238. doi:10.1176/appi.ajp.162.2.228
Mathews CA, Badner JA, Andresen JM, Sheppard B, Himle JA, Grant JE, Williams KA, Chavira DA, Azzam A, Schwartz M, Reus VI, Kim SW, Cook EH, Hanna GL (2012) Genome-wide linkage analysis of obsessive-compulsive disorder implicates chromosome 1p36. Biol Psychiatry 72(8):629–636. doi:10.1016/j.biopsych.2012.03.037
McLoughlin G, Albrecht B, Banaschewski T, Rothenberger A, Brandeis D, Asherson P, Kuntsi J (2009) Performance monitoring is altered in adult ADHD: a familial event-related potential investigation. Neuropsychologia 47(14):3134–3142. doi:10.1016/j.neuropsychologia.2009.07.013
Mehler-Wex C, Riederer P, Gerlach M (2006) Dopaminergic dysbalance in distinct basal ganglia neurocircuits: implications for the pathophysiology of Parkinson’s disease, schizophrenia and attention deficit hyperactivity disorder. Neurotox Res 10(3–4):167–179
Menzies L, Chamberlain SR, Laird AR, Thelen SM, Sahakian BJ, Bullmore ET (2008) Integrating evidence from neuroimaging and neuropsychological studies of obsessive-compulsive disorder: the orbitofronto-striatal model revisited. Neurosci Biobehav Rev 32(3):525–549. doi:10.1016/j.neubiorev.2007.09.005
Mette C, Zimmermann M, Grabemann M, Abdel-Hamid M, Uekermann J, Biskup CS, Wiltfang J, Zepf FD, Kis B (2013) The impact of acute tryptophan depletion on attentional performance in adult patients with ADHD. Acta Psychiatr Scand 128(2):124–132. doi:10.1111/acps.12090
Modesto-Lowe V, Chaplin M, Soovajian V, Meyer A (2013) Are motivation deficits underestimated in patients with ADHD? A review of the literature. Postgrad Med 125(4):47–52. doi:10.3810/pgm.2013.07.2677
Molero Y, Gumpert C, Serlachius E, Lichtenstein P, Walum H, Johansson D, Anckarsater H, Westberg L, Eriksson E, Halldner L (2013) A study of the possible association between adenosine A2A receptor gene polymorphisms and attention-deficit hyperactivity disorder traits. Genes Brain Behav 12(3):305–310. doi:10.1111/gbb.12015
Moritz S, Rietschel L, Jelinek L, Bauml KH (2011) Are patients with obsessive-compulsive disorder generally more doubtful? Doubt is warranted! Psychiatr Res 189(2):265–269. doi:10.1016/j.psychres.2011.07.023
Mossner R, Walitza S, Geller F, Scherag A, Gutknecht L, Jacob C, Bogusch L, Remschmidt H, Simons M, Herpertz-Dahlmann B, Fleischhaker C, Schulz E, Warnke A, Hinney A, Wewetzer C, Lesch KP (2006) Transmission disequilibrium of polymorphic variants in the tryptophan hydroxylase-2 gene in children and adolescents with obsessive-compulsive disorder. Int J Neuropsychopharmacol 9(4):437–442. doi:10.1017/S1461145705005997
Murphy DL, Lesch KP (2008) Targeting the murine serotonin transporter: insights into human neurobiology. Nat Rev Neurosci 9(2):85–96. doi:10.1038/nrn2284
Murphy DL, Zohar J, Benkelfat C, Pato MT, Pigott TA, Insel TR (1989) Obsessive-compulsive disorder as a 5-HT subsystem-related behavioural disorder. Br J Psychiatry Suppl 8:15–24
Nakao T, Radua J, Rubia K, Mataix-Cols D (2011) Gray matter volume abnormalities in ADHD: voxel-based meta-analysis exploring the effects of age and stimulant medication. Am Journal Psychiatry 168(11):1154–1163. doi:10.1176/appi.ajp.2011.11020281
Neale BM, Medland S, Ripke S, Anney RJ, Asherson P, Buitelaar J, Franke B, Gill M, Kent L, Holmans P, Middleton F, Thapar A, Lesch KP, Faraone SV, Daly M, Nguyen TT, Schafer H, Steinhausen HC, Reif A, Renner TJ, Romanos M, Romanos J, Warnke A, Walitza S, Freitag C, Meyer J, Palmason H, Rothenberger A, Hawi Z, Sergeant J, Roeyers H, Mick E, Biederman J, Group IIC (2010a) Case-control genome-wide association study of attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 49(9):906–920. doi:10.1016/j.jaac.2010.06.007
Neale BM, Medland SE, Ripke S, Asherson P, Franke B, Lesch KP, Faraone SV, Nguyen TT, Schafer H, Holmans P, Daly M, Steinhausen HC, Freitag C, Reif A, Renner TJ, Romanos M, Romanos J, Walitza S, Warnke A, Meyer J, Palmason H, Buitelaar J, Vasquez AA, Lambregts-Rommelse N, Gill M, Anney RJ, Langely K, O’Donovan M, Williams N, Owen M, Thapar A, Kent L, Sergeant J, Roeyers H, Mick E, Biederman J, Doyle A, Smalley S, Loo S, Hakonarson H, Elia J, Todorov A, Miranda A, Mulas F, Ebstein RP, Rothenberger A, Banaschewski T, Oades RD, Sonuga-Barke E, McGough J, Nisenbaum L, Middleton F, Hu X, Nelson S (2010b) Meta-analysis of genome-wide association studies of attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 49(9):884–897. doi:10.1016/j.jaac.2010.06.008
Nedeljkovic M, Kyrios M, Moulding R, Doron G, Wainwright K, Pantelis C, Purcell R, Maruff P (2009) Differences in neuropsychological performance between subtypes of obsessive-compulsive disorder. Aust N Z J Psychiatry 43(3):216–226. doi:10.1080/00048670802653273
Nemoda Z, Szekely A, Sasvari-Szekely M (2011) Psychopathological aspects of dopaminergic gene polymorphisms in adolescence and young adulthood. Neurosci Biobehav Rev 35(8):1665–1686. doi:10.1016/j.neubiorev.2011.04.002
Nestadt G, Samuels J, Riddle M, Bienvenu OJ 3rd, Liang KY, LaBuda M, Walkup J, Grados M, Hoehn-Saric R (2000) A family study of obsessive-compulsive disorder. Arch Gen Psychiatry 57(4):358–363
Nestadt G, Grados M, Samuels JF (2010) Genetics of obsessive-compulsive disorder. Psychiatr Clin North Am 33(1):141–158. doi:10.1016/j.psc.2009.11.001
Nicolini H, Arnold P, Nestadt G, Lanzagorta N, Kennedy JL (2009) Overview of genetics and obsessive-compulsive disorder. Psychiatr Res 170(1):7–14. doi:10.1016/j.psychres.2008.10.011
Nielen MM, Den Boer JA (2003) Neuropsychological performance of OCD patients before and after treatment with fluoxetine: evidence for persistent cognitive deficits. Psychol Med 33(5):917–925
Nielen MM, Veltman DJ, de Jong R, Mulder G, den Boer JA (2002) Decision making performance in obsessive compulsive disorder. J Affect Disord 69(1–3):257–260
Nielen MM, den Boer JA, Smid HG (2009) Patients with obsessive-compulsive disorder are impaired in associative learning based on external feedback. Psychol Med 39(9):1519–1526. doi:10.1017/S0033291709005297
Nigg JT, Willcutt EG, Doyle AE, Sonuga-Barke EJ (2005) Causal heterogeneity in attention-deficit/hyperactivity disorder: do we need neuropsychologically impaired subtypes? Biol Psychiatry 57(11):1224–1230. doi:10.1016/j.biopsych.2004.08.025
Nikolaus S, Antke C, Beu M, Muller HW (2010) Cortical GABA, striatal dopamine and midbrain serotonin as the key players in compulsive and anxiety disorders–results from in vivo imaging studies. Rev Neurosci 21(2):119–139
Ogdie MN, Macphie IL, Minassian SL, Yang M, Fisher SE, Francks C, Cantor RM, McCracken JT, McGough JJ, Nelson SF, Monaco AP, Smalley SL (2003) A genomewide scan for attention-deficit/hyperactivity disorder in an extended sample: suggestive linkage on 17p11. Am J Hum Genet 72(5):1268–1279. doi:10.1086/375139
Ogdie MN, Bakker SC, Fisher SE, Francks C, Yang MH, Cantor RM, Loo SK, van der Meulen E, Pearson P, Buitelaar J, Monaco A, Nelson SF, Sinke RJ, Smalley SL (2006) Pooled genome-wide linkage data on 424 ADHD ASPs suggests genetic heterogeneity and a common risk locus at 5p13. Mol Psychiatry 11(1):5–8. doi:10.1038/sj.mp.4001760
Olley A, Malhi G, Sachdev P (2007) Memory and executive functioning in obsessive-compulsive disorder: a selective review. J Affect Disord 104(1–3):15–23. doi:10.1016/j.jad.2007.02.023
Olver JS, O’Keefe G, Jones GR, Burrows GD, Tochon-Danguy HJ, Ackermann U, Scott A, Norman TR (2009) Dopamine D1 receptor binding in the striatum of patients with obsessive-compulsive disorder. J Affect Disord 114(1–3):321–326. doi:10.1016/j.jad.2008.06.020
Olver JS, O’Keefe G, Jones GR, Burrows GD, Tochon-Danguy HJ, Ackermann U, Scott AM, Norman TR (2010) Dopamine D(1) receptor binding in the anterior cingulate cortex of patients with obsessive-compulsive disorder. Psychiatr Res 183(1):85–88. doi:10.1016/j.pscychresns.2010.04.004
Ornstein TJ, Arnold P, Manassis K, Mendlowitz S, Schachar R (2010) Neuropsychological performance in childhood OCD: a preliminary study. Depress Anxiety 27(4):372–380. doi:10.1002/da.20638
Owens JS, Goldfine ME, Evangelista NM, Hoza B, Kaiser NM (2007) A critical review of self-perceptions and the positive illusory bias in children with ADHD. Clin Child Fam Psychol Rev 10(4):335–351. doi:10.1007/s10567-007-0027-3
Paloyelis Y, Mehta MA, Faraone SV, Asherson P, Kuntsi J (2012) Striatal sensitivity during reward processing in attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 51 (7):722–732 e729. doi:10.1016/j.jaac.2012.05.006
Pauls DL (2010) The genetics of obsessive-compulsive disorder: a review. Dialogues Clin Neurosci 12(2):149–163
Pauls DL, Alsobrook JP 2nd, Goodman W, Rasmussen S, Leckman JF (1995) A family study of obsessive-compulsive disorder. Am J Psychiatry 152(1):76–84
Penades R, Catalan R, Andres S, Salamero M, Gasto C (2005) Executive function and nonverbal memory in obsessive-compulsive disorder. Psychiatr Res 133(1):81–90. doi:10.1016/j.psychres.2004.09.005
Piras F, Piras F, Chiapponi C, Girardi P, Caltagirone C, Spalletta G (2013) Widespread structural brain changes in OCD: a systematic review of voxel-based morphometry studies. Cortex. doi:10.1016/j.cortex.2013.01.016
Pittenger C, Bloch MH, Williams K (2011) Glutamate abnormalities in obsessive compulsive disorder: neurobiology, pathophysiology, and treatment. Pharmacol Ther 132(3):314–332. doi:10.1016/j.pharmthera.2011.09.006
Pliszka SR, Liotti M, Woldorff MG (2000) Inhibitory control in children with attention-deficit/hyperactivity disorder: event-related potentials identify the processing component and timing of an impaired right-frontal response-inhibition mechanism. Biol Psychiatry 48(3):238–246
Pliszka SR, Glahn DC, Semrud-Clikeman M, Franklin C, Perez R 3rd, Xiong J, Liotti M (2006) Neuroimaging of inhibitory control areas in children with attention deficit hyperactivity disorder who were treatment naive or in long-term treatment. Am J Psychiatry 163(6):1052–1060. doi:10.1176/appi.ajp.163.6.1052
Polanczyk G, de Lima MS, Horta BL, Biederman J, Rohde LA (2007) The worldwide prevalence of ADHD: a systematic review and metaregression analysis. Am J Psychiatry 164(6):942–948. doi:10.1176/appi.ajp.164.6.942
Porton B, Greenberg BD, Askland K, Serra LM, Gesmonde J, Rudnick G, Rasmussen SA, Kao HT (2013) Isoforms of the neuronal glutamate transporter gene, SLC1A1/EAAC1, negatively modulate glutamate uptake: relevance to obsessive-compulsive disorder. Transl Psychiatry 3:e259. doi:10.1038/tp.2013.35
Pozzi L, Baviera M, Sacchetti G, Calcagno E, Balducci C, Invernizzi RW, Carli M (2011) Attention deficit induced by blockade of N-methyl D-aspartate receptors in the prefrontal cortex is associated with enhanced glutamate release and cAMP response element binding protein phosphorylation: role of metabotropic glutamate receptors 2/3. Neuroscience 176:336–348. doi:10.1016/j.neuroscience.2010.11.060
Radua J, Mataix-Cols D (2009) Voxel-wise meta-analysis of grey matter changes in obsessive-compulsive disorder. Br J Psychiatry 195(5):393–402. doi:10.1192/bjp.bp.108.055046
Rankins D, Bradshaw JL, Georgiou-Karistianis N (2005) Local-global processing in obsessive-compulsive disorder and comorbid Tourette’s syndrome. Brain Cogn 59(1):43–51. doi:10.1016/j.bandc.2005.04.003
Rao NP, Reddy YC, Kumar KJ, Kandavel T, Chandrashekar CR (2008) Are neuropsychological deficits trait markers in OCD? Prog Neuropsychopharmacol Biol Psychiatry 32(6):1574–1579. doi:10.1016/j.pnpbp.2008.05.026
Reiner A, Albin RL, Anderson KD, D’Amato CJ, Penney JB, Young AB (1988) Differential loss of striatal projection neurons in Huntington disease. Proc Natl Acad Sci USA 85(15):5733–5737
Remijnse PL, Nielen MM, van Balkom AJ, Cath DC, van Oppen P, Uylings HB, Veltman DJ (2006) Reduced orbitofrontal-striatal activity on a reversal learning task in obsessive-compulsive disorder. Arch Gen Psychiatry 63(11):1225–1236. doi:10.1001/archpsyc.63.11.1225
Ridderinkhof KR, Ullsperger M, Crone EA, Nieuwenhuis S (2004) The role of the medial frontal cortex in cognitive control. Science 306(5695):443–447. doi:10.1126/science.1100301
Rizzo P, Steinhausen HC, Drechsler R (2010) Self-perception of self-regulatory skills in children with attention-deficit/hyperactivity disorder aged 8-10 years. Atten Defic Hyperact Disord 2(4):171–183. doi:10.1007/s12402-010-0043-x
Robins LN, Helzer JE, Weissman MM, Orvaschel H, Gruenberg E, Burke JD Jr, Regier DA (1984) Lifetime prevalence of specific psychiatric disorders in three sites. Arch Gen Psychiatry 41(10):949–958
Robinson D, Wu H, Munne RA, Ashtari M, Alvir JM, Lerner G, Koreen A, Cole K, Bogerts B (1995) Reduced caudate nucleus volume in obsessive-compulsive disorder. Arch Gen Psychiatry 52(5):393–398
Romanos M, Freitag C, Jacob C, Craig DW, Dempfle A, Nguyen TT, Halperin R, Walitza S, Renner TJ, Seitz C, Romanos J, Palmason H, Reif A, Heine M, Windemuth-Kieselbach C, Vogler C, Sigmund J, Warnke A, Schafer H, Meyer J, Stephan DA, Lesch KP (2008) Genome-wide linkage analysis of ADHD using high-density SNP arrays: novel loci at 5q13.1 and 14q12. Mol Psychiatry 13(5):522–530. doi:10.1038/mp.2008.12
Romanos M, Weise D, Schliesser M, Schecklmann M, Loffler J, Warnke A, Gerlach M, Classen J, Mehler-Wex C (2010) Structural abnormality of the substantia nigra in children with attention-deficit hyperactivity disorder. J Psychiatry Neurosci 35(1):55–58
Rommelfanger KS, Wichmann T (2010) Extrastriatal dopaminergic circuits of the Basal Ganglia. Front Neuroanat 4:139. doi:10.3389/fnana.2010.00139
Rommelse NN, Arias-Vasquez A, Altink ME, Buschgens CJ, Fliers E, Asherson P, Faraone SV, Buitelaar JK, Sergeant JA, Oosterlaan J, Franke B (2008) Neuropsychological endophenotype approach to genome-wide linkage analysis identifies susceptibility loci for ADHD on 2q21.1 and 13q12.11. Am J Hum Genet 83(1):99–105. doi:10.1016/j.ajhg.2008.06.006
Rorden C, Karnath HO, Bonilha L (2007) Improving lesion-symptom mapping. J Cogn Neurosci 19(7):1081–1088
Rosenberg DR, Dick EL, O’Hearn KM, Sweeney JA (1997) Response-inhibition deficits in obsessive-compulsive disorder: an indicator of dysfunction in frontostriatal circuits. J Psychiatry Neurosci 22(1):29–38
Ross J, Badner J, Garrido H, Sheppard B, Chavira DA, Grados M, Woo JM, Doo P, Umana P, Fournier E, Murray SS, Mathews CA (2011) Genomewide linkage analysis in Costa Rican families implicates chromosome 15q14 as a candidate region for OCD. Hum Genet 130(6):795–805. doi:10.1007/s00439-011-1033-6
Rotge JY, Guehl D, Dilharreguy B, Tignol J, Bioulac B, Allard M, Burbaud P, Aouizerate B (2009) Meta-analysis of brain volume changes in obsessive-compulsive disorder. Biol Psychiatry 65(1):75–83. doi:10.1016/j.biopsych.2008.06.019
Rotge JY, Guehl D, Langbour N, Guehl D, Bioulac B, Jaafari N, Allard M, Aouizerate B, Burbaud P (2010) Grey matter alterations in obsessive-compulsive disorder: an anatomic likelihood estimation meta-analysis. Neuropsychopharamacology 35(3):686–691. doi:10.1038/npp.2009.175
Rotge JY, Aouizerate B, Amestoy V, Lambrecq V, Langbour N, Nguyen TH, Dovero S, Cardoit L, Tignol J, Bioulac B, Burbaud P, Guehl D (2012) The associative and limbic thalamus in the pathophysiology of obsessive-compulsive disorder: an experimental study in the monkey. Transl Psychiatry 2:e161. doi:10.1038/tp.2012.88
Rubia K, Overmeyer S, Taylor E, Brammer M, Williams SC, Simmons A, Bullmore ET (1999) Hypofrontality in attention deficit hyperactivity disorder during higher-order motor control: a study with functional MRI. Am J Psychiatry 156(6):891–896
Rubia K, Smith AB, Brammer MJ, Toone B, Taylor E (2005) Abnormal brain activation during inhibition and error detection in medication-naive adolescents with ADHD. Am J Psychiatry 162(6):1067–1075. doi:10.1176/appi.ajp.162.6.1067
Rubia K, Cubillo A, Smith AB, Woolley J, Heyman I, Brammer MJ (2010) Disorder-specific dysfunction in right inferior prefrontal cortex during two inhibition tasks in boys with attention-deficit hyperactivity disorder compared to boys with obsessive-compulsive disorder. Hum Brain Mapp 31(2):287–299. doi:10.1002/hbm.20864
Rubia K, Cubillo A, Woolley J, Brammer MJ, Smith A (2011) Disorder-specific dysfunctions in patients with attention-deficit/hyperactivity disorder compared to patients with obsessive-compulsive disorder during interference inhibition and attention allocation. Hum Brain Mapp 32(4):601–611. doi:10.1002/hbm.21048
Ruchsow M, Reuter K, Hermle L, Ebert D, Kiefer M, Falkenstein M (2007) Executive control in obsessive-compulsive disorder: event-related potentials in a Go/Nogo task. J Neural Transm 114(12):1595–1601. doi:10.1007/s00702-007-0779-4
Rusch N, Boeker M, Buchert M, Glauche V, Bohrmann C, Ebert D, Lieb K, Hennig J, Tebartz Van Elst L (2010) Neurochemical alterations in women with borderline personality disorder and comorbid attention-deficit hyperactivity disorder. World J Biol Psychiatry 11(2 Pt 2):372–381. doi:10.3109/15622970801958331
Sagvolden T, Johansen EB, Aase H, Russell VA (2005) A dynamic developmental theory of attention-deficit/hyperactivity disorder (ADHD) predominantly hyperactive/impulsive and combined subtypes. Behav Brain Sci 28 (3):397–419; discussion 419–368. doi:10.1017/S0140525X05000075
Samuels J, Wang Y, Riddle MA, Greenberg BD, Fyer AJ, McCracken JT, Rauch SL, Murphy DL, Grados MA, Knowles JA, Piacentini J, Cullen B, Bienvenu OJ 3rd, Rasmussen SA, Geller D, Pauls DL, Liang KY, Shugart YY, Nestadt G (2011) Comprehensive family-based association study of the glutamate transporter gene SLC1A1 in obsessive-compulsive disorder. Am J Med Genet B Neuropsychiatr Genet 156B(4):472–477. doi:10.1002/ajmg.b.31184
Sansone RA, Sansone LA (2011) SNRIs pharmacological alternatives for the treatment of obsessive compulsive disorder? Innov Clin Neurosci 8(6):10–14
Santesso DL, Segalowitz SJ, Schmidt LA (2006) Error-related electrocortical responses are enhanced in children with obsessive-compulsive behaviors. Dev Neuropsychol 29(3):431–445. doi:10.1207/s15326942dn2903_3
Savage CR, Keuthen NJ, Jenike MA, Brown HD, Baer L, Kendrick AD, Miguel EC, Rauch SL, Albert MS (1996) Recall and recognition memory in obsessive-compulsive disorder. J Neuropsychiatry Clin Neurosci 8(1):99–103
Savage CR, Baer L, Keuthen NJ, Brown HD, Rauch SL, Jenike MA (1999) Organizational strategies mediate nonverbal memory impairment in obsessive-compulsive disorder. Biol Psychiatry 45(7):905–916
Saviouk V, Hottenga JJ, Slagboom EP, Distel MA, de Geus EJ, Willemsen G, Boomsma DI (2011) ADHD in Dutch adults: heritability and linkage study. Am J Med Genet B Neuropsychiatr Genet 156B(3):352–362. doi:10.1002/ajmg.b.31170
Saxena S, Rauch SL (2000) Functional neuroimaging and the neuroanatomy of obsessive-compulsive disorder. Psychiatr Clin North Am 23(3):563–586
Scarone S, Colombo C, Livian S, Abbruzzese M, Ronchi P, Locatelli M, Scotti G, Smeraldi E (1992) Increased right caudate nucleus size in obsessive-compulsive disorder: detection with magnetic resonance imaging. Psychiatr Res 45(2):115–121
Schachar RJ, Chen S, Logan GD, Ornstein TJ, Crosbie J, Ickowicz A, Pakulak A (2004) Evidence for an error monitoring deficit in attention deficit hyperactivity disorder. J Abnorm Child Psychol 32(3):285–293
Schulz KP, Fan J, Tang CY, Newcorn JH, Buchsbaum MS, Cheung AM, Halperin JM (2004) Response inhibition in adolescents diagnosed with attention deficit hyperactivity disorder during childhood: an event-related FMRI study. Am J Psychiatry 161(9):1650–1657. doi:10.1176/appi.ajp.161.9.1650
Shaw P, Eckstrand K, Sharp W, Blumenthal J, Lerch JP, Greenstein D, Clasen L, Evans A, Giedd J, Rapoport JL (2007) Attention-deficit/hyperactivity disorder is characterized by a delay in cortical maturation. Proc Natl Acad Sci USA 104(49):19649–19654. doi:10.1073/pnas.0707741104
Sheppard B, Chavira D, Azzam A, Grados MA, Umana P, Garrido H, Mathews CA (2010) ADHD prevalence and association with hoarding behaviors in childhood-onset OCD. Depress Anxiety 27(7):667–674. doi:10.1002/da.20691
Shiffrin ND, Gruber J, Glatt SJ, Faraone SV (2013) No association between MspI allele of the ADRA2A polymorphism and ADHD: meta-analysis of family-based studies. Psychiatr Genet 23(4):174–175. doi:10.1097/YPG.0b013e3283631509
Shin MS, Chung SJ, Hong KE (2001) Comparative study of the behavioral and neuropsychologic characteristics of tic disorder with or without attention-deficit hyperactivity disorder (ADHD). J Child Neurol 16(10):719–726
Shin MS, Choi H, Kim H, Hwang JW, Kim BN, Cho SC (2008) A study of neuropsychological deficit in children with obsessive-compulsive disorder. Eur Psychiatry 23(7):512–520. doi:10.1016/j.eurpsy.2008.03.010
Shugart YY, Samuels J, Willour VL, Grados MA, Greenberg BD, Knowles JA, McCracken JT, Rauch SL, Murphy DL, Wang Y, Pinto A, Fyer AJ, Piacentini J, Pauls DL, Cullen B, Page J, Rasmussen SA, Bienvenu OJ, Hoehn-Saric R, Valle D, Liang KY, Riddle MA, Nestadt G (2006) Genomewide linkage scan for obsessive-compulsive disorder: evidence for susceptibility loci on chromosomes 3q, 7p, 1q, 15q, and 6q. Mol Psychiatry 11(8):763–770. doi:10.1038/sj.mp.4001847
Simpson HB, Rosen W, Huppert JD, Lin SH, Foa EB, Liebowitz MR (2006) Are there reliable neuropsychological deficits in obsessive-compulsive disorder? J Psychiatr Res 40(3):247–257. doi:10.1016/j.jpsychires.2005.04.004
Simpson HB, Shungu DC, Bender J Jr, Mao X, Xu X, Slifstein M, Kegeles LS (2012) Investigation of cortical glutamate-glutamine and gamma-aminobutyric acid in obsessive-compulsive disorder by proton magnetic resonance spectroscopy. Neuropsychopharmacology 37(12):2684–2692. doi:10.1038/npp.2012.132
Sinzig J, Morsch D, Bruning N, Schmidt MH, Lehmkuhl G (2008) Inhibition, flexibility, working memory and planning in autism spectrum disorders with and without comorbid ADHD-symptoms. Child Adolesc Psychiatry Ment Health 2(1):4. doi:10.1186/1753-2000-2-4
Soeiro-De-Souza MG, Stanford MS, Bio DS, Machado-Vieira R, Moreno RA (2013) Association of the COMT Met(1)(5)(8) allele with trait impulsivity in healthy young adults. Mol Med Rep 7(4):1067–1072. doi:10.3892/mmr.2013.1336
Sohn MH, Albert MV, Jung K, Carter CS, Anderson JR (2007) Anticipation of conflict monitoring in the anterior cingulate cortex and the prefrontal cortex. Proc Natl Acad Sci USA 104(25):10330–10334. doi:10.1073/pnas.0703225104
Sonuga-Barke EJ (2002) Psychological heterogeneity in AD/HD—a dual pathway model of behaviour and cognition. Behav Brain Res 130(1–2):29–36
Sonuga-Barke EJ (2005) Causal models of attention-deficit/hyperactivity disorder: from common simple deficits to multiple developmental pathways. Biol Psychiatry 57(11):1231–1238. doi:10.1016/j.biopsych.2004.09.008
Sonuga-Barke E, Bitsakou P, Thompson M (2010) Beyond the dual pathway model: evidence for the dissociation of timing, inhibitory, and delay-related impairments in attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 49(4):345–355
Sowell ER, Thompson PM, Welcome SE, Henkenius AL, Toga AW, Peterson BS (2003) Cortical abnormalities in children and adolescents with attention-deficit hyperactivity disorder. Lancet 362(9397):1699–1707. doi:10.1016/S0140-6736(03)14842-8
Spencer TJ, Biederman J, Faraone SV, Madras BK, Bonab AA, Dougherty DD, Batchelder H, Clarke A, Fischman AJ (2013) Functional genomics of attention-deficit/hyperactivity disorder (ADHD) risk alleles on dopamine transporter binding in ADHD and healthy control subjects. Biol Psychiatry 74(2):84–89. doi:10.1016/j.biopsych.2012.11.010
Steinhausen HC, Bisgaard C, Munk-Jorgensen P, Helenius D (2013) Family aggregation and risk factors of obsessive-compulsive disorders in a nationwide three-generation study. Depress Anxiety. doi:10.1002/da.22163
Stewart SE, Geller DA, Jenike M, Pauls D, Shaw D, Mullin B, Faraone SV (2004) Long-term outcome of pediatric obsessive-compulsive disorder: a meta-analysis and qualitative review of the literature. Acta Psychiatr Scand 110(1):4–13. doi:10.1111/j.1600-0447.2004.00302.x
Stewart SE, Jenike EA, Hezel DM, Stack DE, Dodman NH, Shuster L, Jenike MA (2010) A single-blinded case-control study of memantine in severe obsessive-compulsive disorder. J Clin Psychopharmacol 30(1):34–39. doi:10.1097/JCP.0b013e3181c856de
Stewart SE, Mayerfeld C, Arnold PD, Crane JR, O’Dushlaine C, Fagerness JA, Yu D, Scharf JM, Chan E, Kassam F, Moya PR, Wendland JR, Delorme R, Richter MA, Kennedy JL, Veenstra-VanderWeele J, Samuels J, Greenberg BD, McCracken JT, Knowles JA, Fyer AJ, Rauch SL, Riddle MA, Grados MA, Bienvenu OJ, Cullen B, Wang Y, Shugart YY, Piacentini J, Rasmussen S, Nestadt G, Murphy DL, Jenike MA, Cook EH, Pauls DL, Hanna GL, Mathews CA (2013a) Meta-analysis of association between obsessive-compulsive disorder and the 3′ region of neuronal glutamate transporter gene SLC1A1. Am J Med Genet B Neuropsychiatr Genet 162B(4):367–379. doi:10.1002/ajmg.b.32137
Stewart SE, Yu D, Scharf JM, Neale BM, Fagerness JA, Mathews CA, Arnold PD, Evans PD, Gamazon ER, Davis LK, Osiecki L, McGrath L, Haddad S, Crane J, Hezel D, Illman C, Mayerfeld C, Konkashbaev A, Liu C, Pluzhnikov A, Tikhomirov A, Edlund CK, Rauch SL, Moessner R, Falkai P, Maier W, Ruhrmann S, Grabe HJ, Lennertz L, Wagner M, Bellodi L, Cavallini MC, Richter MA, Cook EH Jr, Kennedy JL, Rosenberg D, Stein DJ, Hemmings SM, Lochner C, Azzam A, Chavira DA, Fournier E, Garrido H, Sheppard B, Umana P, Murphy DL, Wendland JR, Veenstra-VanderWeele J, Denys D, Blom R, Deforce D, Van Nieuwerburgh F, Westenberg HG, Walitza S, Egberts K, Renner T, Miguel EC, Cappi C, Hounie AG, Conceicao do Rosario M, Sampaio AS, Vallada H, Nicolini H, Lanzagorta N, Camarena B, Delorme R, Leboyer M, Pato CN, Pato MT, Voyiaziakis E, Heutink P, Cath DC, Posthuma D, Smit JH, Samuels J, Bienvenu OJ, Cullen B, Fyer AJ, Grados MA, Greenberg BD, McCracken JT, Riddle MA, Wang Y, Coric V, Leckman JF, Bloch M, Pittenger C, Eapen V, Black DW, Ophoff RA, Strengman E, Cusi D, Turiel M, Frau F, Macciardi F, Gibbs JR, Cookson MR, Singleton A, North American Brain Expression C, Hardy J, Database UKBE, Crenshaw AT, Parkin MA, Mirel DB, Conti DV, Purcell S, Nestadt G, Hanna GL, Jenike MA, Knowles JA, Cox N, Pauls DL (2013b) Genome-wide association study of obsessive-compulsive disorder. Mol Psychiatry 18(7):788–798. doi:10.1038/mp.2012.85
Strik WK, Fallgatter AJ, Brandeis D, Pascual-Marqui RD (1998) Three-dimensional tomography of event-related potentials during response inhibition: evidence for phasic frontal lobe activation. Electroencephalogr Clin Neurophysiol 108(4):406–413
Sun H, Yuan F, Shen X, Xiong G, Wu J (2013) Role of COMT in ADHD: a Systematic Meta-Analysis. Mol Neurobiol. doi:10.1007/s12035-013-8516-5
Szeszko PR, Christian C, Macmaster F, Lencz T, Mirza Y, Taormina SP, Easter P, Rose M, Michalopoulou GA, Rosenberg DR (2008) Gray matter structural alterations in psychotropic drug-naive pediatric obsessive-compulsive disorder: an optimized voxel-based morphometry study. Am J Psychiatry 165(10):1299–1307. doi:10.1176/appi.ajp.2008.08010033
Tamm L, Menon V, Ringel J, Reiss AL (2004) Event-related FMRI evidence of frontotemporal involvement in aberrant response inhibition and task switching in attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 43(11):1430–1440. doi:10.1097/01.chi.0000140452.51205.8d
Taylor S (2013) Molecular genetics of obsessive-compulsive disorder: a comprehensive meta-analysis of genetic association studies. Mol Psychiatry 18(7):799–805. doi:10.1038/mp.2012.76
Thomsen PH (2013) Obsessive-compulsive disorders. Eur Child Adolesc Psychiatry 22(Suppl 1):S23–S28. doi:10.1007/s00787-012-0357-7
Tolin DF, Villavicencio A, Umbach A, Kurtz MM (2011) Neuropsychological functioning in hoarding disorder. Psychiatr Res 189(3):413–418. doi:10.1016/j.psychres.2011.06.022
Trifilieff P, Feng B, Urizar E, Winiger V, Ward RD, Taylor KM, Martinez D, Moore H, Balsam PD, Simpson EH, Javitch JA (2013) Increasing dopamine D2 receptor expression in the adult nucleus accumbens enhances motivation. Mol Psychiatry 18(9):1025–1033. doi:10.1038/mp.2013.57
Tukel R, Gurvit H, Ozturk N, Ozata B, Ertekin BA, Ertekin E, Baran B, Kalem SA, Buyukgok D, Direskeneli GS (2013) COMT Val158Met polymorphism and executive functions in obsessive-compulsive disorder. J Neuropsychiatry Clin Neurosci 25(3):214–221. doi:10.1176/appi.neuropsych.12040103
Ullsperger M, von Cramon DY (2004) Decision making, performance and outcome monitoring in frontal cortical areas. Nat Neurosci 7(11):1173–1174. doi:10.1038/nn1104-1173
Ullsperger M, von Cramon DY (2006) The role of intact frontostriatal circuits in error processing. J Cogn Neurosci 18(4):651–664. doi:10.1162/jocn.2006.18.4.651
Ursu S, Stenger VA, Shear MK, Jones MR, Carter CS (2003) Overactive action monitoring in obsessive-compulsive disorder: evidence from functional magnetic resonance imaging. Psychol Sci 14(4):347–353
Valera EM, Faraone SV, Murray KE, Seidman LJ (2007) Meta-analysis of structural imaging findings in attention-deficit/hyperactivity disorder. Biol Psychiatry 61(12):1361–1369. doi:10.1016/j.biopsych.2006.06.011
van den Heuvel OA, Veltman DJ, Groenewegen HJ, Cath DC, van Balkom AJ, van Hartskamp J, Barkhof F, van Dyck R (2005) Frontal-striatal dysfunction during planning in obsessive-compulsive disorder. Arch Gen Psychiatry 62(3):301–309. doi:10.1001/archpsyc.62.3.301
van den Heuvel OA, van der Werf YD, Verhoef KM, de Wit S, Berendse HW, Wolters E, Veltman DJ, Groenewegen HJ (2010) Frontal-striatal abnormalities underlying behaviours in the compulsive-impulsive spectrum. J Neurol Sci 289(1–2):55–59. doi:10.1016/j.jns.2009.08.043
van der Meer JM, Oerlemans AM, van Steijn DJ, Lappenschaar MG, de Sonneville LM, Buitelaar JK, Rommelse NN (2012) Are autism spectrum disorder and attention-deficit/hyperactivity disorder different manifestations of one overarching disorder? Cognitive and symptom evidence from a clinical and population-based sample. J Am Acad Child Adolesc Psychiatry 51 (11):1160–1172 e1163. doi:10.1016/j.jaac.2012.08.024
van Grootheest DS, Cath DC, Beekman AT, Boomsma DI (2005) Twin studies on obsessive-compulsive disorder: a review. Twin Res Hum Genet 8(5):450–458. doi:10.1375/183242705774310060
van Grootheest DS, Boomsma DI, Hettema JM, Kendler KS (2008) Heritability of obsessive-compulsive symptom dimensions. Am J Med Genet B Neuropsychiatr Genet 147B(4):473–478. doi:10.1002/ajmg.b.30622
van Meel CS, Heslenfeld DJ, Oosterlaan J, Sergeant JA (2007) Adaptive control deficits in attention-deficit/hyperactivity disorder (ADHD): the role of error processing. Psychiatr Res 151(3):211–220. doi:10.1016/j.psychres.2006.05.011
van Veen V, Carter CS (2002a) The anterior cingulate as a conflict monitor: fMRI and ERP studies. Physiol Behav 77(4–5):477–482
van Veen V, Carter CS (2002b) The timing of action-monitoring processes in the anterior cingulate cortex. J Cogn Neurosci 14(4):593–602. doi:10.1162/08989290260045837
Veale DM, Sahakian BJ, Owen AM, Marks IM (1996) Specific cognitive deficits in tests sensitive to frontal lobe dysfunction in obsessive-compulsive disorder. Psychol Med 26(6):1261–1269
Vloet TD, Marx I, Kahraman-Lanzerath B, Zepf FD, Herpertz-Dahlmann B, Konrad K (2010) Neurocognitive performance in children with ADHD and OCD. J Abnorm Child Psychol 38(7):961–969. doi:10.1007/s10802-010-9422-1
Vulink NC, Westenberg HG, van Nieuwerburgh F, Deforce D, Fluitman SB, Meinardi JS, Denys D (2012) Catechol-O-methyltranferase gene expression is associated with response to citalopram in obsessive-compulsive disorder. Int J Psychiatry Clin Pract 16(4):277–283. doi:10.3109/13651501.2011.653375
Walitza S (2014) Zwangsstörungen im DSM-5: was ist neu? Z Kinder Jugendpsychiatr 42(2):121–126. doi:10.1024/1422-4917/a000279
Walitza S, Renner TJ, Dempfle A, Konrad K, Wewetzer C, Halbach A, Herpertz-Dahlmann B, Remschmidt H, Smidt J, Linder M, Flierl L, Knolker U, Friedel S, Schafer H, Gross C, Hebebrand J, Warnke A, Lesch KP (2005) Transmission disequilibrium of polymorphic variants in the tryptophan hydroxylase-2 gene in attention-deficit/hyperactivity disorder. Mol Psychiatry 10(12):1126–1132. doi:10.1038/sj.mp.4001734
Walitza S, Zellmann H, Irblich B, Lange KW, Tucha O, Hemminger U, Wucherer K, Rost V, Reinecker H, Wewetzer C, Warnke A (2008) Children and adolescents with obsessive-compulsive disorder and comorbid attention-deficit/hyperactivity disorder: preliminary results of a prospective follow-up study. J Neural Transm 115(2):187–190. doi:10.1007/s00702-007-0841-2
Walitza S, Wendland JR, Gruenblatt E, Warnke A, Sontag TA, Tucha O, Lange KW (2010) Genetics of early-onset obsessive-compulsive disorder. Eur Child Adolesc Psychiatry 19(3):227–235. doi:10.1007/s00787-010-0087-7
Wan M, Hejjas K, Ronai Z, Elek Z, Sasvari-Szekely M, Champagne FA, Miklosi A, Kubinyi E (2013) DRD4 and TH gene polymorphisms are associated with activity, impulsivity and inattention in Siberian Husky dogs. Anim Genet. doi:10.1111/age.12058
Wang Z, Xiao Z, Inslicht SS, Tong H, Jiang W, Wang X, Metzler T, Marmar CR, Jiang S (2009) Low expression of catecholamine-O-methyl-transferase gene in obsessive-compulsive disorder. J Anxiety Disord 23(5):660–664. doi:10.1016/j.janxdis.2009.02.004
Wang Y, Adamczyk A, Shugart YY, Samuels JF, Grados MA, Greenberg BD, Knowles JA, McCracken JT, Rauch SL, Murphy DL, Rasmussen SA, Cullen B, Pinto A, Fyer AJ, Piacentini J, Pauls DL, Bienvenu OJ, Riddle M, Liang KY, Valle D, Wang T, Nestadt G (2010) A screen of SLC1A1 for OCD-related alleles. Am J Med Genet B Neuropsychiatr Genet 153B(2):675–679. doi:10.1002/ajmg.b.31001
Watkins LH, Sahakian BJ, Robertson MM, Veale DM, Rogers RD, Pickard KM, Aitken MR, Robbins TW (2005) Executive function in Tourette’s syndrome and obsessive-compulsive disorder. Psychol Med 35(4):571–582
Westenberg HG, Fineberg NA, Denys D (2007) Neurobiology of obsessive-compulsive disorder: serotonin and beyond. CNS Spectr 12(2 Suppl 3):14–27
Whiteside SP, Abramowitz JS, Port JD (2012) Decreased caudate N-acetyl-l-aspartic acid in pediatric obsessive-compulsive disorder and the effects of behavior therapy. Psychiatr Res 202(1):53–59. doi:10.1016/j.pscychresns.2011.11.010
Wilens TE, Hahesy AL, Biederman J, Bredin E, Tanguay S, Kwon A, Faraone SV (2005) Influence of parental SUD and ADHD on ADHD in their offspring: preliminary results from a pilot-controlled family study. Am J Addict 14(2):179–187. doi:10.1080/10550490590924872
Willcutt EG, Pennington BF, Olson RK, Chhabildas N, Hulslander J (2005) Neuropsychological analyses of comorbidity between reading disability and attention deficit hyperactivity disorder: in search of the common deficit. Dev Neuropsychol 27(1):35–78. doi:10.1207/s15326942dn2701_3
Wood AC, Neale MC (2010) Twin studies and their implications for molecular genetic studies: endophenotypes integrate quantitative and molecular genetics in ADHD research. J Am Acad Child Adolesc Psychiatry 49(9):874–883. doi:10.1016/j.jaac.2010.06.006
Woolley J, Heyman I, Brammer M, Frampton I, McGuire PK, Rubia K (2008) Brain activation in paediatric obsessive compulsive disorder during tasks of inhibitory control. Br J Psychiatry 192(1):25–31. doi:10.1192/bjp.bp.107.036558
World Health Organization (1996) International statistical classification of diseases and related health problems, 10th revision (ICD-10), 10th edn. WHO, Geneva
Wu J, Xiao H, Sun H, Zou L, Zhu LQ (2012) Role of dopamine receptors in ADHD: a systematic meta-analysis. Mol Neurobiol 45(3):605–620. doi:10.1007/s12035-012-8278-5
Wu H, Wang X, Xiao Z, Yu S, Zhu L, Wang D, Jiang K, Wang Z, Zhang T, Fralick D (2013a) Association between SLC1A1 gene and early-onset OCD in the Han Chinese population: a case-control study. J Mol Neurosci 50(2):353–359. doi:10.1007/s12031-013-9995-6
Wu K, Hanna GL, Easter P, Kennedy JL, Rosenberg DR, Arnold PD (2013b) Glutamate system genes and brain volume alterations in pediatric obsessive-compulsive disorder: a preliminary study. Psychiatr Res 211(3):214–220. doi:10.1016/j.pscychresns.2012.07.003
Yerys BE, Wallace GL, Sokoloff JL, Shook DA, James JD, Kenworthy L (2009) Attention deficit/hyperactivity disorder symptoms moderate cognition and behavior in children with autism spectrum disorders. Autism Res 2(6):322–333. doi:10.1002/aur.103
Yucel M, Wood SJ, Wellard RM, Harrison BJ, Fornito A, Pujol J, Velakoulis D, Pantelis C (2008) Anterior cingulate glutamate-glutamine levels predict symptom severity in women with obsessive-compulsive disorder. Aust N Z J Psychiatry 42(6):467–477. doi:10.1080/00048670802050546
Yuen EY, Zhong P, Li X, Wei J, Yan Z (2013) Restoration of glutamatergic transmission by dopamine D4 receptors in stressed animals. J Biol Chem 288(36):26112–26120. doi:10.1074/jbc.M112.396648
Zandt F, Prior M, Kyrios M (2007) Repetitive behaviour in children with high functioning autism and obsessive compulsive disorder. J Autism Dev Disord 37(2):251–259. doi:10.1007/s10803-006-0158-2
Zandt F, Prior M, Kyrios M (2009) Similarities and differences between children and adolescents with autism spectrum disorder and those with obsessive compulsive disorder: executive functioning and repetitive behaviour. Autism 13(1):43–57. doi:10.1177/1362361308097120
Zellmann H, Jans T, Irblich B, Hemminger U, Reinecker H, Sauer C, Lange KW, Tucha O, Wewetzer C, Warnke A, Walitza S (2009) Children and adolescents with obsessive-compulsive disorders. Z Kinder Jugendpsychiatr Psychother 37(3):173–182. doi:10.1024/1422-4917.37.3.173
Zepf FD, Landgraf M, Biskup CS, Dahmen B, Poustka F, Wockel L, Stadler C (2013) No effect of acute tryptophan depletion on verbal declarative memory in young persons with ADHD. Acta Psychiatr Scand 128(2):133–141. doi:10.1111/acps.12089
Zhang L, Chang S, Li Z, Zhang K, Du Y, Ott J, Wang J (2012) ADHDgene: a genetic database for attention deficit hyperactivity disorder. Nucleic Acids Res 40 (Database issue):D1003–1009. doi:10.1093/nar/gkr992
Zhou K, Dempfle A, Arcos-Burgos M, Bakker SC, Banaschewski T, Biederman J, Buitelaar J, Castellanos FX, Doyle A, Ebstein RP, Ekholm J, Forabosco P, Franke B, Freitag C, Friedel S, Gill M, Hebebrand J, Hinney A, Jacob C, Lesch KP, Loo SK, Lopera F, McCracken JT, McGough JJ, Meyer J, Mick E, Miranda A, Muenke M, Mulas F, Nelson SF, Nguyen TT, Oades RD, Ogdie MN, Palacio JD, Pineda D, Reif A, Renner TJ, Roeyers H, Romanos M, Rothenberger A, Schafer H, Sergeant J, Sinke RJ, Smalley SL, Sonuga-Barke E, Steinhausen HC, van der Meulen E, Walitza S, Warnke A, Lewis CM, Faraone SV, Asherson P (2008) Meta-analysis of genome-wide linkage scans of attention deficit hyperactivity disorder. Am J Med Genet B Neuropsychiatr Genet 147B(8):1392–1398. doi:10.1002/ajmg.b.30878
Zimmermann M, Grabemann M, Mette C, Abdel-Hamid M, Uekermann J, Kraemer M, Wiltfang J, Kis B, Zepf FD (2012) The effects of acute tryptophan depletion on reactive aggression in adults with attention-deficit/hyperactivity disorder (ADHD) and healthy controls. PLoS ONE 7(3):e32023. doi:10.1371/journal.pone.0032023
Zohar AH (1999) The epidemiology of obsessive-compulsive disorder in children and adolescents. Child Adolesc Psychiatr Clin N Am 8(3):445–460
Author information
Authors and Affiliations
Corresponding author
Additional information
Silvia Brem and Edna Grünblatt have contributed equally to the work.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Brem, S., Grünblatt, E., Drechsler, R. et al. The neurobiological link between OCD and ADHD. ADHD Atten Def Hyp Disord 6, 175–202 (2014). https://doi.org/10.1007/s12402-014-0146-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12402-014-0146-x