Abstract
Background
Neonatal jaundice is a common condition characterized by a yellowish discoloration of the skin, conjunctiva, and sclera caused by elevated serum or plasma bilirubin levels during the newborn period. The condition is usually not dangerous, but it can progress to severe hyperbilirubinemia, which can lead to acute bilirubin encephalopathy and kernicterus, a bilirubin-induced neurological damage. Therefore, this study aimed to assess the pooled prevalence of neonatal jaundice and its determinants in Ethiopia.
Methods
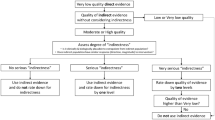
Scopus, PubMed, Google Scholar, Embase, and CINAHL databases were searched for studies published between January 1, 2010 and July 30, 2021. A weighted DerSimonian Laird random-effects model was used to estimate the pooled prevalence of neonatal jaundice and its associated factors. The I2 was used to calculate the degree of heterogeneity. The funnel plot and Egger's regression test were used to assess publication bias.
Results
Totally 697 articles were generated from various databases, and the review included a total of eight articles. The pooled prevalence of neonatal jaundice was 30.96% [95% confidence interval (CI) 16.61%–45.31%)] in Ethiopia. This review showed that prolonged labor [adjusted odd ratio (AOR) = 3.39; 95% CI 2.41–4.77), low birth weight (AOR = 5.12; 95% CI 3.11–8.72), birth asphyxia (AOR = 3.75; 95% CI 2.11–6.66), cephalohematoma (AOR = 7.07; 95% CI 2.72–18.38), ABO incompatibility (AOR = 6.05; 95% CI 2.95–12.42), Rhesus (RH) incompatibility (AOR = 3.77; 95% CI 2.04–6.96), male sex (AOR = 4.53; 95% CI 3.39–6.07), and neonatal sepsis (AOR = 2.47; 95% CI 1.49–4.08) were identified as a determining factor for neonatal jaundice in Ethiopia.
Conclusions
In low- and middle-income countries, neonatal jaundice is a significant healthcare burden, accounting for a significant portion of global childhood mortality and morbidity. However, some low-cost, effective, practical, and dependable solutions have been implemented. Prolonged labor, ABO incompatibility, RH incompatibility, birth asphyxia, neonatal sepsis, low birth weight, cephalohematoma, and male sex were identified as risk factors for neonatal jaundice in Ethiopia.






Similar content being viewed by others
References
Leung TS, Outlaw F, MacDonald LW, Meek J. Jaundice Eye Color Index (JECI): quantifying the yellowness of the sclera in jaundiced neonates with digital photography. Biomed Opt Express. 2019;10:1250–6.
Olusanya BO, Ogunlesi TA, Slusher TM. Why is kernicterus still a major cause of death and disability in low-income and middle-income countries? Arch Dis Child. 2014;99:1117–21.
Olusanya BO, Kaplan M, Hansen TWR. Neonatal hyperbilirubinaemia: a global perspective. Lancet Child Adolesc Health. 2018;2:610–20.
Greco C, Arnolda G, Boo NY, Iskander IF, Okolo AA, Rohsiswatmo R, et al. Neonatal jaundice in low- and middle-income countries: lessons and future directions from the 2015 Don Ostrow trieste yellow retreat. Neonatology. 2016;110:172–80.
Erdeve O, Okulu E, Olukman O, Ulubas D, Buyukkale G, Narter F, et al. The Turkish Neonatal Jaundice Online Registry: a national root cause analysis. PLoS ONE. 2018;13:e0193108.
Mitra S, Rennie J. Neonatal jaundice: aetiology, diagnosis and treatment. Br J Hosp Med (Lond). 2017;78:699–704.
Le Pichon JB, Riordan SM, Watchko J, Shapiro SM. The neurological sequelae of neonatal hyperbilirubinemia: definitions, diagnosis and treatment of the kernicterus spectrum disorders (KSDs). Curr Pediatr Rev. 2017;13:199–209.
Olusanya BO, Osibanjo FB, Mabogunje CA, Slusher TM, Olowe SA. The burden and management of neonatal jaundice in Nigeria: a scoping review of the literature. Niger J Clin Pract. 2016;19:1–17.
Tette EMA, Nartey ET, Nuertey BD, Azusong EA, Akaateba D, Yirifere J, et al. The pattern of neonatal admissions and mortality at a regional and district hospital in the Upper West Region of Ghana; a cross-sectional study. PLoS ONE. 2020;15:e0232406.
Harsha L, Priya J, Shah KK, Reshmi B. Systemic approach to management of neonatal jaundice and prevention of kernicterus. Res J Pharm Technol. 2015;8:1087.
Stevenson DK, Vreman HJ, Wong RJ. Bilirubin production and the risk of bilirubin neurotoxicity. Semin Perinatol. 2011;35:121–6.
Maisels MJ. Managing the jaundiced newborn: a persistent challenge. CMAJ. 2015;187:335–43.
Bhutani VK, Zipursky A, Blencowe H, Khanna R, Sgro M, Ebbesen F, et al. Neonatal hyperbilirubinemia and Rhesus disease of the newborn: incidence and impairment estimates for 2010 at regional and global levels. Pediatr Res. 2013;74:86–100.
Olusanya BO, Osibanjo FB, Slusher TM. Risk factors for severe neonatal hyperbilirubinemia in low and middle-income countries: a systematic review and meta-analysis. PLoS ONE. 2015;10:e0117229.
Arnolda G, Thein AA, Trevisanuto D, Aung N, Nwe HM, Thin AA, et al. Evaluation of a simple intervention to reduce exchange transfusion rates among inborn and outborn neonates in Myanmar, comparing pre- and post-intervention rates. BMC Pediatr. 2015;15:216.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4:1.
Sanderson S, Tatt ID, Higgins J. Tools for assessing quality and susceptibility to bias in observational studies in epidemiology: a systematic review and annotated bibliography. Int J Epidemiol. 2007;36:666–76.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–58.
Sterne JA, Egger M. Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemiol. 2001;54:1046–55.
Duval S, Tweedie R. A nonparametric, “Trim and Fill” method of accounting for publication bias in meta-analysis. J Am Stat Assoc. 2000;95:89–98.
Tessema M. Assessment of magnitude and determinants of neonatal jaundice among neonates admitted to neonatal intensive care unit of Dessie town public hospitals, Amhara region, Ethiopia, 2020. 2020. http://etd.aau.edu.et/handle/123456789/24245.
Gudeta H. Assesment of magnitude and associated factors of neonatal hyperbilirubinemia at neonatal intensive care unit of tikur anbessa specialized Hospital, Addis Ababa, Ethiopia, 2017. 2017. http://thesisbank.jhia.ac.ke/6565/ Accessed 13 June 2022.
Bizuneh AD, Alemnew B, Getie A, Wondmieneh A, Gedefaw G. Determinants of neonatal jaundice among neonates admitted to five referral hospitals in Amhara region, Northern Ethiopia: an unmatched case-control study. BMJ Paediatr Open. 2020;4:e000830.
Asefa GG, Gebrewahid TG, Nuguse H, Gebremichael MW, Birhane M, Zereabruk K, et al. Determinants of neonatal jaundice among neonates admitted to neonatal intensive care unit in public general hospitals of Central Zone, Tigray, Northern Ethiopia, 2019: a case-control study. Biomed Res Int. 2020;2020:4743974.
Birhanu MY, Workineh AA, Molla Y, Abebaw E, Arora A, Bazezew Y. Rate and Predictors of Neonatal Jaundice in Northwest Ethiopia: Prospective Cohort Study. J Multidiscip Healthc. 2021;14:447–57.
Aynalem YA, Mulu GB, Akalu TY, Shiferaw WS. Prevalence of neonatal hyperbilirubinaemia and its association with glucose-6-phosphate dehydrogenase deficiency and blood-type incompatibility in sub-Saharan Africa: a systematic review and meta-analysis. BMJ Paediatr Open. 2020;4:e000750.
Lake EA, Abera GB, Azeze GA, Gebeyew NA, Demissie BW. Magnitude of neonatal jaundice and its associated factor in neonatal intensive care units of Mekelle City Public Hospitals, Northern Ethiopia. Int J Pediatr. 2019;2019:1054943.
Girma MT. Prevalence and contributing factors of neonatal jaundice in neonatal intensive care unit at St Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia, 2019. J Health Med Nurs. 2020;74:21–6.
Aynalem YA, Mulu GB, Akalu TY, Shiferaw WS. Prevalence of neonatal hyperbilirubinaemia and its association with glucose-6-phosphate dehydrogenase deficiency and blood-type incompatibility in sub-Saharan Africa: a systematic review and meta-analysis. BMJ Paediatrics Open. 2020;4:4–7.
Onyearugha CN, Onyire BN, Ugboma HAA. Neonatal jaundice: Prevalence and associated factors as seen in Federal medical centre Abakaliki. Southeast Nigeria J Clin Med Res. 2011;3:40–5.
Slusher TM, Zamora TG, Appiah D, Stanke JU, Strand MA, Lee BW, et al. Burden of severe neonatal jaundice: a systematic review and meta-analysis. BMJ Paediatr Open. 2017;1:e000105.
Scrafford CG, Mullany LC, Katz J, Khatry SK, LeClerq SC, Darmstadt GL, et al. Incidence of and risk factors for neonatal jaundice among newborns in southern Nepal. Trop Med Int Health. 2013;18:1317–28.
Tavakolizadeh R, Izadi A, Seirafi G, Khedmat L, Mojtahedi SY. Maternal risk factors for neonatal jaundice: a hospital-based cross-sectional study in Tehran. Eur J Trans Myol. 2018;28:256–62.
Akangire G, Carter B. Birth injuries in neonates. Pediatr Rev. 2016;37:451–62.
Sukla KK, Tiwari PK, Kumar A, Raman R. Low birthweight (LBW) and neonatal hyperbilirubinemia (NNH) in an Indian cohort: association of homocysteine, its metabolic pathway genes and micronutrients as risk factors. PLoS ONE. 2013;8:e71587.
Menon S, Amanullah N. Maternal and neonatal determinants of neonatal jaundice-a case-control study. J Clin Med Res. 2017;5:19659–65.
Chime HE, Egenede JA, Arute JE. Prevalence of neonatal jaundice on central hospital, Warri, delta state. Nigeria Int J Health Res. 2012;4:123–6.
Korejo HB, Bhurgri GR, Bhand S, Qureshi MA, Dahri GM, Chohan RK, et al. Risk factors for kernicterus in neonatal jaundice. Gomal J Med Sci. 2010;8:12–5.
Morioka I. Hyperbilirubinemia in preterm infants in Japan: New treatment criteria. Pediatr Int. 2018;60:684–90.
Lai MC, Yang SN. Perinatal hypoxic-ischemic encephalopathy. J Biomed Biotechnol. 2010;2011:609813.
Simon EN. Effects of perinatal asphyxia plus bilirubin? Pediatrics. 2011;127:e858.
Garosi E, Mohammadi F, Ranjkesh F. The relationship between neonatal jaundice and maternal and neonatal factors. Iran J Neonatol. 2016;7:37–40.
Israel-Aina YT, Omoigberale AI. Risk factors for neonatal jaundice in babies presenting at the University of Benin Teaching Hospital. Benin City Niger J Clin Pract. 2012;39:159–63.
Erdeve O, Okulu E, Olukman O, Ulubas D, Buyukkale G, Narter F, et al. The Turkish neonatal jaundice online registry: a national root cause analysis. PLoS ONE. 2018;13:e0193108.
Chand N, Sanyal AJ. Sepsis-induced cholestasis. Hepatology. 2007;45:230–41.
Acknowledgements
The authors would like to thank all of the original study’s authors and publishers.
Funding
The author did not receive any fundings for this study.
Author information
Authors and Affiliations
Contributions
HGB, GAD, and MDW: conceptualization, data curation, formal analysis, and interpretation, funding acquisition, investigation, methodology, software; writing–review and editing. ADA, BGK, and GNM: supervision, validation, visualization, formal analysis, writing–original draft, writing–review, and editing.
Corresponding author
Ethics declarations
Conflict of interest
Non-financial benefits have been received.
Ethical approval
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Belay, H.G., Debebe, G.A., Ayele, A.D. et al. Determinants of neonatal jaundice in Ethiopia: a systematic review and meta-analysis. World J Pediatr 18, 725–733 (2022). https://doi.org/10.1007/s12519-022-00597-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12519-022-00597-3