Abstract
Intensive care unit (ICU) is a critical resource in a hospital, especially in developing countries such as India. The length of ICU stay after a cardiac surgery is an important variable for effective use of this critical resource. In this context, a predictive model can help a hospital to make optimum use of its ICU occupancy. A study was thus conducted on ICU patients and data gather over a 1-year period in a hospital in India. The critical factors for prolonged ICU stay (more than 72 h) were identified using univariate and multivariate logistic regression and a predictive index was built based on model development set. The predictive index was tested on a validation set and the mean length of ICU stay appeared to increase with an increase in the risk score. In addition, the risk score was tested in case of mortality. Efficient use of the ICU facility is possible with the help of this predictive index.
Similar content being viewed by others
1 Introduction
Intensive care unit (ICU) is a critical resource for a hospital, especially in developing countries such as India. As health care expenses rise and given that charges for ICU services constitute a significant portion of the total cost of patients’ overall hospital stay, those with prolonged ICU stay need special attention.
Postoperative stay (in hours) in the ICU following a cardiac surgery is an important variable for estimating the overall use of the ICU. For optimum capacity utilization of ICU in a hospital, a predictive model to obtain this information is critical for planning admission for an elective surgery or immediate postoperative care. This study develops an index, which is probably the first attempt in India.
This study is based on similar studies in Canada [1] and Europe [2]. Given that no such work exists in India so far, the past studies have been extended to the Indian context. This study was undertaken in a hospital in the western part of India. Data were gathered for a 1-year period on the demographic details of patients staying in the ICU. Once patient is admitted in a hospital who require a cardiac surgery, we need to know the severity of the patient. One way is to go by the conventional wisdom of the cardiologists and alternate way is the develop a severity score based on the scientific data analysis. If such system and severity (or critically) score is available, then the patients can be treated differently based on such criticality score. Although several studies done in western countries have developed such a severity score and some of those hospitals are possibly using the score, there is no such index available for Indian hospitals in similar condition We developed a predictive length of stay based on univariate and multivariate logistics regression and validated by 1-year dataset. The sample dataset was divided into two groups: one for model development and the other for model validation. The study identifies the critical factors for prolonged ICU stay (i.e., more than 72 h) using univariate and multivariate logistic regression, the mean length of ICU stay is found to increase with an increase in the risk scores.
The remainder of this paper is organized as follows. Section 2 presents a brief review of the available literature on the length of ICU stay. Section 3 describes the problem and the methodology used. Sections 4 and 5 present the data analysis and research findings, respectively. Section 6 describes the predictive index for coronary artery bypass grafting (CABG) patients. The findings are compared with that of the earlier studies in Sect. 7. Section 8 discusses the potential applications of the study. Finally, Sect. 9 presents the conclusions and discusses the possible extensions of the study.
2 Review of related literature
Several studies exist [3,4,5], on this subject in field of operations research, management science, and statistics. Need for using operations research, management science and statistics have been highlighted in several studies. The study [5] presents a conceptual framework for ICU capacity strain, considers what data elements may contribute to it, and suggests methods for determining the optimal metric. The studies by Solberg et al. [3], Troy and Rosenberg [4] demonstrates that application of scientific analysis for ICU capacity utilization.
A literature review shows that researchers rely on univariate and multivariate logistic regression to build a predictive index for the length of ICU stay. A predictive index is built on 713 patients and validated on 691 patients. This index is also tested for ICU stay more than 2, 4, 7, 10 days, and mortality [1]. In the Euro SCORE [2], a scoring system is developed from 13,302 patients, which predicts mortality in case of patients of cardiac surgery in Europe. Similar studies were undertaken by Tu et al. [6] and Tuman et al. [7]. While several researchers adopt similar methods of analysis, they find other factors significant for prolonged ICU stay, such as inotropic agents [8]. Christakis et al. [9] found that recent myocardial infarction and continued preoperative smoking were significant precursors. Lung disease, no-sinus-rhythm, no-mild valve pathology, reoperation, no-elective operation, and no-off-pump procedure were found to be responsible for prolonged ICU stay [10], while Ghotkar et al. [11] found renal dysfunction, unstable angina, poor ejection fraction, peripheral vascular disease, obesity, increasing age, smoking, diabetes, hypercholesterolaemia, hypertension, and Cardiopulmonary Bypass (CPB) as significant risk factors. Gender is also an important factor for prolonged ICU stay and even after preoperative adjustments female patients tend to stay longer in the ICU than male patients [12]. Another preoperative factor is on- and off-pump CABG, with off-pump CABG exhibiting a weaker correlation with prolonged ICU stay [13].
Numerous studies exist on operations research applications in ICU. Ridge et al. [14] employed a simulation model for ICU beds and suggested a scheduling system for elective patients, and Kim et al. [15] examined the ICU admission and discharge data with queuing framework and through computer simulation models. Kim et al. [16] suggested that a few beds may be reserved for elective patients to minimize the number of cancelled surgeries where they used simulation models to assess various bed reservation schemes based on the data on ICU. Often, an alternative ICU is used when the appropriate ICU is full. Vohra et al. [17] addressed this issue and developed a queuing model, which increased ICU utilization by 6.29%.
A comprehensive literature review did not reveal any prospective study on the length of ICU stay in the Indian context for a large number of consecutive patients. The present study addresses this gap. The study also includes more details of the patients such as risk factors (diabetes mellitus, hypertension, ischemic heart disease, left ventricular dysfunction), surgery on- or off-bypass pump, time spent on ventilator, and hematologic and pathologic investigations (haemoglobin, potassium, fasting blood sugar). However, the New York Heart Association Class and Charlson Comorbidity score in the study were not considered. Tu et al. [1] considered the length of ICU stay in number of days, but, in this study, data are gathered on an hourly basis, which makes the study more precise and relevant.
3 Problem description and research methodology
This study was conducted in a hospital in western India. It is based on univariate and multivariate logistic regression. Typically, logistic regression is used to predict a dichotomous variable—in this case, the length of ICU stay. As the ICU is a critical resource of a hospital, optimum utilization is essential. Higher-risk patients are likely to have longer ICU stays, resulting in the unavailability of ICU beds for new arrivals. The predictor variables are a mix of continuous and categorical variables.
Clinical data were obtained from forms filled in by the referring cardiologist and entered into a database for 1-year period. These data included patient’s name, age, gender, risk factors, left ventricular function, nature and type of the surgery performed and whether the patient had a history of cardiac surgery, surgery performed on- or off-bypass pump, time spent on ventilation, and details of pathological investigations such as haemoglobin (Hb), potassium (K) and fasting blood sugar (FBS). Left ventricular function is determined by the referring cardiologist and assigned a grade based on the ejection fraction (LVEF). The nature (urgency) and types of surgery are defined (e.g., CABG and valve surgery). Diabetes mellitus (DM) and hypertension (HT) as considered risk factors for cardiac surgery. Ischemic heart disease (IHD) is considered as a risk factor in surgeries where CABG is an add-on procedure (e.g., during aortic valve replacement). The data are gathered with the help of the hospital Admission Book, Death Book, patient’s personal file, and the daily chart sheet.
4 Data analysis
In this study, logistic regression is used to develop a predictive model for the length of ICU stay and the data are analysed using the Statistical Analysis Software (SAS 5.1). Data of 1289 patients admitted in 1 year were collected. First, the study sample was divided into a model derivation set and a validation set. The model is derived with 690 patients and the predictive power on 580 patients is verified. There were 19 reported cases of death in the sample. The predictive index was validated separately for patient deaths. A frequency distribution table was constructed, which showed that the length of the ICU stay was 48–72 h for a majority of patients. Therefore, in the Indian context, 72 h was assigned as the usual length of ICU stay following cardiac surgery. Further, this study identified the critical factors for which the length of ICU stay is more than 72 h, for which univariate analysis was conducted for all of the predictor variables. Our predicted variable is the length of ICU stay, which is a dichotomous variable and predictor variables are age, gender, left ventricular function, type of surgery, history of surgery, surgery on- or off-bypass pump, risk factors, duration of ventilator support, and hematologic and biochemical (blood) investigations. Only age and blood investigation details are continuous predictors, while the other details are categorical. Age is categorized into three groups (≤ 50 years, 51–74 years, and ≥ 75 years). Left ventricular function is grouped as into normal/Mild LV dysfunction (LVEF > 40%), moderate (LVEF 30–40%), and severe LV dysfunction (LVEF < 30%). The nature of surgery is classified as emergent (surgery required within 24 h of first presentation), urgent (surgery required within 24 to 72 h), and elective (planned admission for surgery). If a patient has a history of surgery, then that variable becomes a binary.
Surgeries are categorized into five classes:
-
(1)
Coronary Artery Bypass Grafting (CABG);
-
(2)
Surgeries with add-on CABG, such as double valve replacement (CABG + DVR), aortic valve replacement (CABG + AVR), mitral valve replacement (CABG + MVR), and mitral valve repair (CABG + MV repair);
-
(3)
Surgical ventricular restoration (CABG + SVR);
-
(4)
All types of stand-alone valve replacement or repair of Mitral, Aortic or both valves.
-
(5)
Others—including corrective surgeries for congenital heart diseases such as Tetralogy of Fallot (TOF), atrial septal defect (ASD), and ventricular septal defect (VSD).
Surgery on- or off-bypass pump is also a binary variable. DM, HT, and IHD are considered risk factors for a patient. All possible combinations of these risk factors are considered and eight different risk groups (presence of single risk factor i.e., DM, HT, and IHD; presence of two risk factors i.e., DM and HT, DM and IHD, HT and IHD; presence of all three risk factors and absence of all three risk factors) are identified. The hours spent on ventilation are classified into three categories (≤ 5 h, 5.1–10 h and > 10 h). The value of haemoglobin was classified as ≥ 10 gm % or < 10 gm %; potassium ≤ 3.5, 3.51 to 4.49 and ≥ 4.5 meq/lit; fasting blood sugar ≤ 110, 110 to 159.9 and ≥ 160 mg %.
Univariate analysis was run for each of these predictor variables and the odds ratios, Chi square statistics, and the associated p values were obtained using the software. The least mean length of ICU stay was considered as a reference category and others coded as 1 or 0 according to the presence or absence of that particular category.
Following the univariate analysis, a multivariate logistic regression model was developed. The potential predictors, which are significant at 10% level, are included in the multivariate logistic regression model. In the multivariate model, the odds ratios, Chi square statistics, and the associated p values are measured again.
The risk scores were developed using the odds ratios of the multivariate logistic regression model. Values of odds ratios are rounded to the nearest integer and considered as risk scores. The risk score was tested on the validation set (i.e., on 580 patients). A test was also conducted to confirm whether it could predict the mean length of ICU stay higher than 72 h, 96 h, and 120 h, as well as patient death.
5 Research findings and results
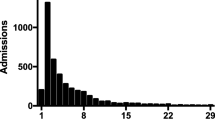
A frequency distribution of the number of patients against the length of ICU stay was developed (Fig. 1).
Table 1 presents the numbers regarding the diagram along with the cumulative percentage.
Table 1 shows that a majority of patients require ICU stay of about 48–72 h. Nearly 63% patients stay less than 72 h in an ICU, which means 37% patients stay more than 72 h. Therefore, ICU stay more than 72 h is assigned as the time limit beyond which the ICU stay was considered long for the purpose of this study in the context of cardiac surgery care in India.
Table 2 shows the results of the univariate analysis for 690 patients of the derivation set.
Variables such as patient’s age above 51 years; moderate and severe type of LV dysfunction; surgeries such as valve surgery, CABG, CABG and valve, CABG and SVR; presence of IHD as a risk factor, requiring ventilation for more than 10 h; are Hb less than 10 gm are found to be statistically significant at 10% level. Gender is not found to be a critical factor for prolonged ICU stay (significant at 15% level). Patients younger than 50 years who have normal or mild left ventricular dysfunction undergoing elective surgery, operated off pump, Hb greater than 10 gm, FBS less than 110, and stay on ventilation for less than 5 h are considered as the base category, because these patients have a short length of ICU stay.
According to the univariate analysis, patients who are aged at least 51 years having moderate or severe LV dysfunction; who are undergoing valve, CABG, CABG and valve, CABG and SVR surgeries; and requiring ventilation for more than 10 h, whose Hb is less than 10 gm, would probably stay longer in the ICU. These factors are significant at 10% level and are included in the logistic regression.
Table 3 shows the logistic regression model.
Six variables (age, LV dysfunction, CABG + valve surgery, IHD as risk factor, time spent on ventilation more than 10 h and Hb < 10 gm %) are found to be statistically significant at the 10% level.
Further, risk scores based on the odds ratios of the significant variables are developed. Table 4 shows the predictive index.
The index is validated on 580 patients to check their ability to predict the mean length of ICU stay by grouping the risk scores shown in Table 5.
The number of patients in each risk group; their mean length of ICU stay; and mean stay of more than 72 h, 96 h, and 120 h are enumerated. Risk scores are between 0 and 17. Higher scores indicate higher risk. Table 5 shows that the mean length of ICU stay increases as the risk score increases. For a lowest risk score (0–1), the mean length of ICU stay is 68.48 h; whereas for the highest risk (11–17), it is 124.70 h. The index is also validated for ICU stay of more than 72, 96, and 120 h and it is able to predict prolonged ICU stay. The study dataset included 19 death cases and this index is also validated for all cases of mortality (Table 6).
As much as 58% of deaths occurred in those in the 11–17 risk score range. Thus, the predictive index correlates well with respect to mortality.
The predictive power of risk scores is compared based on the model development set with the validation set and analysed in two ways. Figures 2 and 3 consider the individual risk scores, whereas Figs. 4 and 5 consider the grouped risk scores. The curves for the model development set (Figs. 2, 4) are quite similar to those of the validation set (Figs. 3, 5), which confirm that the risk scores based on the model development set work well with the validation set.
6 Predictive index for coronary artery bypass grafting patients
The predictive index is developed based on 690 patients and validated on 580 patients. In the derivation set, 501 out of 690 patients undergo CABG, and 446 of 580 patients undergo CABG in the validation set. The rest undergo surgeries for valve disease, among others. Thus, 70% of the study population were undergoing CABG. A comparative analysis between the CABG patients and all surgical patients is carried out.
All the variables considered in the previous analysis are categorized as before.
Table 7 shows the univariate analysis.
In the univariate analysis, age above 50 years, severe left ventricular dysfunction, requirement of ventilation above 10 h, and haemoglobin less than 10 gm % are considered as critical factors (significant at 10% level) for prolonged ICU stay for CABG patients. Factors such as gender of the patient, type of surgery performed, whether the patient had past history of surgery, and surgery on- or off-bypass pump are not found to be significant.
Factors found to be significant in the univariate analysis are entered in the logistic regression (Table 8).
All the variables are significant at the 10% level in the multivariate analysis. A predictive index for CABG patients based on the odds ratios of the variables in the logistic regression is developed. The risk score ranges from 0 to 11. The predictive index for CABG patients is shown in Table 9.
The predictive index is validated on 446 patients. In the previous analysis, the risk scores are combined into five groups, but for CABG there are grouped into four and the number of patients in each group; their mean length of ICU stay; and a mean stay of more than 72, 96, and 120 h are measured.
For a 0–1 risk score, the mean length of ICU stay is 66.14 h and 8–11 is considered as a high risk score, which has a mean length of ICU stay of around 112.09 h. Of 37 patients, 26 have prolonged ICU stays (Table 10).
7 Comparison with earlier studies
Although the present study extends the findings of the study by Tu et al. [1], there are some significant differences in the present findings from the published literature. The salient differences are as follows:
-
(1)
Tu et al. [1] found that female gender and urgent and emergent surgeries are significant factors for prolonged ICU stay, whereas these are not relevant in the present study. In this study, predictors such as risk factors (DM, HT, and IHD), on-/off-bypass pump, time required on ventilation, and pathological investigation (Hb and FBS) and the New York Heart Association class and Charlson comorbidity score are not considered. This study find that IHD is a risk factor and requirement of ventilation for more than 10 h and haemoglobin less than 10 gm% are significant factors responsible for prolonged ICU stays.
-
(2)
The study findings are significantly different from Butterworth et al. [12], which showed that female ICU stay is longer than male ICU stay, whereas gender was not a predictive factor in our study.
-
(3)
Bucerius et al. [13] found that on-pump CABG has a strong association with prolonged ICU stay, but in the present analysis found no such correlation.
8 Potential application of the study
The predictive index could be applied for diverse utilities, ranging from patient care to an objective comparison between surgical centres. The potential applications could be as follows:
-
1.
Prognostication and counselling of patient’s relatives can be facilitated when such a predictive index is used for individual surgeries. The approximate length of ICU stay and hospitalization can then be conveyed to the patient’s relatives. This is extremely reassuring to the family and would help greatly in managing the needs of the patient and their relatives.
-
2.
Scheduling of patients in busy surgical centers and ICUs can be done efficiently. Elective surgeries can be efficiently scheduled to maximize the use of an operating team or ICU beds. Emergency surgeries can be factored into smoothen the scheduling difficulties by using this predictive index.
-
3.
If the predictive index is used in combination with the patient load statistics, it may help the hospital administration to predict future need of expansion of facilities and the logistics involved.
-
4.
The length of ICU stay and hospitalization is an important component in the rating of cardiac surgical teams worldwide. The predictive index would serve as a benchmark for comparison with different surgical teams or hospitals. The operative and outcome data of different surgical teams can be normalized with respect to the predictive index, their outcomes can then be meaningfully compared. The predictive index would also be important to emphasize that patient demographics and clinical parameters would significantly affect the length of ICU stay and morbidity; prolonged ICU stay need not necessarily reflect on a surgical team’s ability.
-
5.
Improvement in surgical techniques, hardware, and care has resulted in favourable outcomes even in most critical patients. At the same time, patients who are in a worse condition are being operated upon in even greater numbers. The predictive index would serve to objectively define the changing demographics and corresponding improvement in outcomes when comparing data over a period of years.
-
6.
The predictive index is a good indicator of mortality risk. In high-risk patients, when counselling the patient and relatives, the index can be one of the tools to objectively and realistically discuss the outcome. Consent to surgery would then be a considered decision by the patient and relatives. In India, a philosophical attitude toward life at extremes of age may lead the patient and relatives toward a conservative management strategy rather than invasive or operative therapy. The predictive index may help in making this decision.
-
7.
In our study we found that on pump and off pump has no difference with respect to the LOS. However, with interaction of the several cardiologists we found that in several cities in India, the cardiologists tend to fast track off pump CABG patients and allow them to stay for a shorter duration in the ICU. There may be non-medical reasons attributed to this. It is possible that due to peer pressure, pressure on the hospital management to curtail cost or pressure on the doctors to fit into government scheme, where every additional day in ICU tends to eat into the viability of offering such programs. A study in this direction may correct this practice.
9 Conclusion and extension
This study is based on the data of a hospital in western India. This prospective study is the first of its kind for such a large population in the Indian context. As the risk score increases, the mean length of ICU stay also increases. For high risk scores, the percentage of patients staying in the ICU for more than 72 h is also high. Therefore, this predictive model is well fitted for the validation set and the logistic regression model is also robust. Therefore, it is recommended that with the patient’s demographic details, the hospital can manage its ICU capacity and plan to use this most critical resource efficiently, which is very effective in developing countries such as India. Future studies must consider the implemented of this index in practice. This study strongly recommends development of a risk score to address the criticality of ICU patients.
This study may be extended to more hospitals and a comparison between the results can be made.
References
Tu, J.V., Mazer, D., Levinton, C., Armstrong, P.W., Naylor, D.A.: Predictive index for length of stay in the intensive care unit following cardiac surgery. Can. Med. Assoc. J. 151, 177–185 (1994)
Nashef, S.A.M., Roques, F., Michel, P., Gauducheau, E., Lemeshow, S., Salamon, R.: The EuroSCORE study group; European system for cardiac operative risk evaluation (EuroSCORE). Eur. J. Cardiothorac. Surg. 16, 9–13 (1999)
Solberg, B.C., Dirksen, C.D., Nieman, F.H., et al.: Introducing an integrated intermediate care unit improves ICU utilization: a prospective intervention study. BMC Anesthesiol 14, 76 (2014). https://doi.org/10.1186/1471-2253-14-76
Troy, M., Rosenberg, L.: Using simulation to determine the need for ICU beds for surgery patients. Surgery 146(4), 608–620 (2009)
Halpern, S.D.: ICU capacity strain and the quality and allocation of critical care. Curr. Opin. Crit. Care 17(6), 648–657 (2011)
Tu, J.V., Jaglal, S.B., Naylor, C.D.: Multicenter validation of a risk index for mortality, intensive care unit stay, and overall hospital length of stay after cardiac surgery. Am. Heart Assoc. 91, 677–684 (1995)
Tuman, K.J., McCarthy, R.J., March, R.J., Najafi, H., Ivankovich, A.D.: Morbidity and duration of ICU stay after cardiac surgery a model for preoperative risk assessment. Chest 102(1), 36–44 (1992)
Michalopoulos, A., Tzelepis, G., Pavlides, G., Kriaras, J., Dafni, U., Geroulanos, S.: Determinants of duration of ICU stay after coronary artery bypass graft surgery. Br. J. Anaesth. 77(2), 208–212 (1996)
Christakis, G.T., Fremes, S.E., Naylor, C.D., Chen, E., Rao, V., Goldman, B.S.: Impact of preoperative risk and preoperative morbidity on ICU stay following coronary bypass surgery. Cardiovasc. Surg. 4, 29–35 (2000)
Janssen, D.P., Noyez, L., Wouters, C., Brouwer, R.M.: Preoperative prediction of prolonged stay in the intensive care unit for coronary bypass surgery. Eur. J. Cardiothorac. Surg. 25(2), 203–207 (2004)
Ghotkar, S.V., Grayson, A.D., Fabri, B.M., Dihmis, W., Pullan, D.M.: Preoperative calculation of risk for prolonged intensive care unit stay following coronary artery bypass grafting. J. Cardiothor. Surg. 1(14), 1–14 (2006)
Butterworth, J., James, R., Prielipp, R., Cerese, J., Livingston, J., Burnett, D.: Female gender associates with increased duration of intubation and length of stay after coronary artery surgery. CABG Clin. Benchmark. Database Particip. Anesthesiol. 92(2), 414–424 (2000)
Bucerius, J., Gummert, J.F., Walther, T., Doll, N., Falk, V., Schmitt, D.V., Mohr, F.W.: Predictors of prolonged ICU stay after on-pump versus off-pump coronary artery bypass grafting. Intensive Care Med. 30(1), 88–95 (2004)
Ridge, J.C., Jones, S.K., Nielsen, M.S., Shahani, A.K.: Capacity planning for intensive care units. Eur. J. Oper. Res. 105, 346–355 (1998)
Kim, S.C., Horowitz, I., Young, K.K., Buckley, T.A.: Analysis of capacity management of the intensive care unit in a hospital. Eur. J. Oper. Res. 115, 36–46 (1999)
Kim, S.C., Horowitz, I., Young, K.K., Buckley, T.A.: Flexible bed allocation and performance in the intensive care unit. J. Oper. Manag. 18, 427–443 (2000)
Vohra, S., Dutta, G., Ghosh, D.K.: Capacity management of intensive care units in a multi-specialty hospital in India. Indian Institute of Management Ahmedabad Working Paper, No.2006-07-04 (2006)
Funding
The funding was provided by Indian Institute of Management Ahmedabad (Grant No. IIMA-R&P 2010).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dutta, G., Naik, A., Gosai, D. et al. A mathematical model for predicting length of postoperative intensive care requirement following cardiac surgery in an Indian hospital. OPSEARCH 58, 330–350 (2021). https://doi.org/10.1007/s12597-020-00480-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12597-020-00480-7