Abstract
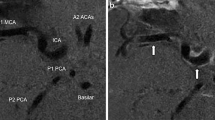
Subarachnoid hemorrhage (SAH) is associated with a high incidence of morbidity and mortality, particularly within the first 72 h after aneurysm rupture. We recently found ultra-early cerebral thrombosis, detectable on T2* magnetic resonance imaging (MRI), in a mouse SAH model at 4 h after onset. The current study examined whether such changes also occur in rat at 24 h after SAH, the vessels involved, whether the degree of thrombosis varied with SAH severity and brain injury, and if it differed between male and female rats. Adult Sprague Dawley rats were subjected to an endovascular perforation SAH model or sham surgery and underwent T2 and T2* MRI 24 h later. Following SAH, increased numbers of T2* hypointense vessels were detected on MRI. The number of such vessels correlated with SAH severity, as assessed by MRI-based grading of bleeding. Histologically, thrombotic vessels were found on hematoxylin and eosin staining, had a single layer of smooth muscle cells on alpha-smooth muscle actin immunostaining, and had laminin 2α/fibrinogen double labeling, suggesting venule thrombosis underlies the T2*-positive vessels on MRI. Capillary thrombosis was also detected which may follow the venous thrombosis. In both male and female rats, the number of T2*-positive thrombotic vessels correlated with T2 lesion volume and neurological function, and the number of such vessels was significantly greater in female rats. In summary, this study identified cerebral venous thrombosis 24 h following SAH in rats that could be detected with T2* MRI imaging and may contribute to SAH-induced brain injury.






Similar content being viewed by others
References
Broderick JP, Brott TG, Duldner JE, Tomsick T, Leach A. Initial and recurrent bleeding are the major causes of death following subarachnoid hemorrhage. Stroke. 1994;25(7):1342–7. https://doi.org/10.1161/01.str.25.7.1342.
Nieuwkamp DJ, Setz LE, Algra A, Linn FH, de Rooij NK, Rinkel GJ. Changes in case fatality of aneurysmal subarachnoid haemorrhage over time, according to age, sex, and region: a meta-analysis. Lancet Neurol. 2009;8(7):635–42. https://doi.org/10.1016/S1474-4422(09)70126-7.
Fujii M, Yan J, Rolland WB, Soejima Y, Caner B, Zhang JH. Early brain injury, an evolving frontier in subarachnoid hemorrhage research. Transl Stroke Res. 2013;4(4):432–46. https://doi.org/10.1007/s12975-013-0257-2.
Vergouwen MD, Vermeulen M, Coert BA, Stroes ES, Roos YB. Microthrombosis after aneurysmal subarachnoid hemorrhage: an additional explanation for delayed cerebral ischemia. J Cereb Blood Flow Metab. 2008;28(11):1761–70. https://doi.org/10.1038/jcbfm.2008.74.
Clarke JV, Suggs JM, Diwan D, Lee JV, Lipsey K, Vellimana AK, et al. Microvascular platelet aggregation and thrombosis after subarachnoid hemorrhage: A review and synthesis. J Cereb Blood Flow Metab. 2020;40(8):1565–75. https://doi.org/10.1177/0271678X20921974.
Dienel A, Ammassam Veettil R, Hong SH, Matsumura K, Kumar TP, Yan Y, et al. Microthrombi Correlates With Infarction and Delayed Neurological Deficits After Subarachnoid Hemorrhage in Mice. Stroke. 2020;51(7):2249–54. https://doi.org/10.1161/STROKEAHA.120.029753.
Sabri M, Ai J, Lakovic K, D’Abbondanza J, Ilodigwe D, Macdonald RL. Mechanisms of microthrombi formation after experimental subarachnoid hemorrhage. Neuroscience. 2012;224:26–37. https://doi.org/10.1016/j.neuroscience.2012.08.002.
Grote E, Hassler W. The critical first minutes after subarachnoid hemorrhage. Neurosurgery. 1988;22(4):654–61. https://doi.org/10.1227/00006123-198804000-00006.
Aguiar de Sousa D, Lucas Neto L, Jung S, Penas S, Panos L, Heldner MR, et al. Brush Sign Is Associated With Increased Severity in Cerebral Venous Thrombosis. Stroke. 2019;50(6):1574–7. https://doi.org/10.1161/STROKEAHA.119.025342.
Buyck PJ, Zuurbier SM, Garcia-Esperon C, Barboza MA, Costa P, Escudero I, et al. Diagnostic accuracy of noncontrast CT imaging markers in cerebral venous thrombosis. Neurology. 2019;92(8):e841–51. https://doi.org/10.1212/WNL.0000000000006959.
Lv B, Tian CL, Cao XY, Liu XF, Wang J, Yu SY. Role of diffusion-weighted imaging in the diagnosis of cerebral venous thrombosis. J Int Med Res. 2020;48(6):300060520933448. https://doi.org/10.1177/0300060520933448.
Ta HT, Arndt N, Wu Y, Lim HJ, Landeen S, Zhang R, et al. Activatable magnetic resonance nanosensor as a potential imaging agent for detecting and discriminating thrombosis. Nanoscale. 2018;10(31):15103–15. https://doi.org/10.1039/c8nr05095c.
Ta HT, Li Z, Hagemeyer CE, Cowin G, Zhang S, Palasubramaniam J, et al. Molecular imaging of activated platelets via antibody-targeted ultra-small iron oxide nanoparticles displaying unique dual MRI contrast. Biomaterials. 2017;134:31–42. https://doi.org/10.1016/j.biomaterials.2017.04.037.
Wang Z, Chen J, Toyota Y, Keep RF, Xi G, Hua Y. Ultra-Early Cerebral Thrombosis Formation After Experimental Subarachnoid Hemorrhage Detected on T2* Magnetic Resonance Imaging. Stroke. 2021:STROKEAHA120032397. https://doi.org/10.1161/STROKEAHA.120.032397
Longstreth WT Jr, Koepsell TD, Yerby MS, van Belle G. Risk factors for subarachnoid hemorrhage. Stroke. 1985;16(3):377–85. https://doi.org/10.1161/01.str.16.3.377.
Kongable GL, Lanzino G, Germanson TP, Truskowski LL, Alves WM, Torner JC, et al. Gender-related differences in aneurysmal subarachnoid hemorrhage. J Neurosurg. 1996;84(1):43–8. https://doi.org/10.3171/jns.1996.84.1.0043.
Lee JY, Keep RF, He Y, Sagher O, Hua Y, Xi G. Hemoglobin and iron handling in brain after subarachnoid hemorrhage and the effect of deferoxamine on early brain injury. J Cereb Blood Flow Metab. 2010;30(11):1793–803. https://doi.org/10.1038/jcbfm.2010.137.
Egashira Y, Hua Y, Keep RF, Xi G. Acute white matter injury after experimental subarachnoid hemorrhage: potential role of lipocalin 2. Stroke. 2014;45(7):2141–3. https://doi.org/10.1161/STROKEAHA.114.005307.
Egashira Y, Shishido H, Hua Y, Keep RF, Xi G. New grading system based on magnetic resonance imaging in a mouse model of subarachnoid hemorrhage. Stroke. 2015;46(2):582–4. https://doi.org/10.1161/STROKEAHA.114.007834.
Dang G, Yang Y, Wu G, Hua Y, Keep RF, Xi G. Early Erythrolysis in the Hematoma After Experimental Intracerebral Hemorrhage. Transl Stroke Res. 2017;8(2):174–82. https://doi.org/10.1007/s12975-016-0505-3.
Tan XX, Chen JY, Keep RF, Xi GH, Hua Y. Prx2 (Peroxiredoxin 2) as a Cause of Hydrocephalus After Intraventricular Hemorrhage. Stroke. 2020;51(5):1578–86. https://doi.org/10.1161/Strokeaha.119.028672.
Wan Y, Gao F, Ye F, Yang W, Hua Y, Keep RF, et al. Effects of aging on hydrocephalus after intraventricular hemorrhage. Fluids Barriers CNS. 2020;17(1):8. https://doi.org/10.1186/s12987-020-0169-y.
Wei J, Wang M, Jing C, Keep RF, Hua Y, Xi G. Multinucleated Giant Cells in Experimental Intracerebral Hemorrhage. Transl Stroke Res. 2020;11(5):1095–102. https://doi.org/10.1007/s12975-020-00790-4.
Hannocks MJ, Pizzo ME, Huppert J, Deshpande T, Abbott NJ, Thorne RG, et al. Molecular characterization of perivascular drainage pathways in the murine brain. J Cereb Blood Flow Metab. 2018;38(4):669–86. https://doi.org/10.1177/0271678X17749689.
Behrouzi R, Punter M. Diagnosis and management of cerebral venous thrombosis. Clin Med (Lond). 2018;18(1):75–9. https://doi.org/10.7861/clinmedicine.18-1-75.
Tiebosch IA, van den Bergh WM, Bouts MJ, Zwartbol R, van der Toorn A, Dijkhuizen RM. Progression of brain lesions in relation to hyperperfusion from subacute to chronic stages after experimental subarachnoid hemorrhage: a multiparametric MRI study. Cerebrovasc Dis. 2013;36(3):167–72. https://doi.org/10.1159/000352048.
Shimoda M, Takeuchi M, Tominaga J, Oda S, Kumasaka A, Tsugane R. Asymptomatic versus symptomatic infarcts from vasospasm in patients with subarachnoid hemorrhage: serial magnetic resonance imaging. Neurosurgery. 2001;49(6):1341–8. https://doi.org/10.1097/00006123-200112000-00010 (discussion 8-50).
Kivisaari RP, Salonen O, Servo A, Autti T, Hernesniemi J, Ohman J. MR imaging after aneurysmal subarachnoid hemorrhage and surgery: a long-term follow-up study. AJNR Am J Neuroradiol. 2001;22(6):1143–8.
Rashad S, Niizuma K, Sato-Maeda M, Fujimura M, Mansour A, Endo H, et al. Early BBB breakdown and subacute inflammasome activation and pyroptosis as a result of cerebral venous thrombosis. Brain Res. 2018;1699:54–68. https://doi.org/10.1016/j.brainres.2018.06.029.
Dewyer NA, Sood V, Lynch EM, Luke CE, Upchurch GR Jr, Wakefield TW, et al. Plasmin inhibition increases MMP-9 activity and decreases vein wall stiffness during venous thrombosis resolution. J Surg Res. 2007;142(2):357–63. https://doi.org/10.1016/j.jss.2007.03.064.
Ding Y, Li X. Resistin Promotes Thrombosis in Rats with Deep Vein Thrombosis via Up-Regulating MMP-2, MMP-9, and PAI-1. Clin Lab. 2019;65(10). https://doi.org/10.7754/Clin.Lab.2019.181119
Guo D, Wilkinson DA, Thompson BG, Pandey AS, Keep RF, Xi G, et al. MRI Characterization in the Acute Phase of Experimental Subarachnoid Hemorrhage. Transl Stroke Res. 2017;8(3):234–43. https://doi.org/10.1007/s12975-016-0511-5.
Shishido H, Zhang H, Okubo S, Hua Y, Keep RF, Xi G. The Effect of Gender on Acute Hydrocephalus after Experimental Subarachnoid Hemorrhage. Acta Neurochir Suppl. 2016;121:335–9. https://doi.org/10.1007/978-3-319-18497-5_58.
Prunell GF, Mathiesen T, Diemer NH, Svendgaard NA. Experimental subarachnoid hemorrhage: subarachnoid blood volume, mortality rate, neuronal death, cerebral blood flow, and perfusion pressure in three different rat models. Neurosurgery. 2003;52(1):165–75. https://doi.org/10.1097/00006123-200301000-00022 (discussion 75-6).
Shishido H, Egashira Y, Okubo S, Zhang H, Hua Y, Keep RF, et al. A magnetic resonance imaging grading system for subarachnoid hemorrhage severity in a rat model. J Neurosci Methods. 2015;243:115–9. https://doi.org/10.1016/j.jneumeth.2015.01.035.
Friedrich V, Bederson JB, Sehba FA. Gender influences the initial impact of subarachnoid hemorrhage: an experimental investigation. PLoS ONE. 2013;8(11):e80101. https://doi.org/10.1371/journal.pone.0080101.
Etminan N, Chang HS, Hackenberg K, de Rooij NK, Vergouwen MDI, Rinkel GJE, et al. Worldwide Incidence of Aneurysmal Subarachnoid Hemorrhage According to Region, Time Period, Blood Pressure, and Smoking Prevalence in the Population: A Systematic Review and Meta-analysis. JAMA Neurol. 2019;76(5):588–97. https://doi.org/10.1001/jamaneurol.2019.0006.
Funding
YH, RFK, and GX were supported by grants NS-096917, NS106746, NS112394, and NS116786 from the National Institutes of Health (NIH).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
All institutional and national guidelines for the care and use of laboratory animals were followed.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zhang, J., Peng, K., Ye, F. et al. Acute T2*-Weighted Magnetic Resonance Imaging Detectable Cerebral Thrombosis in a Rat Model of Subarachnoid Hemorrhage. Transl. Stroke Res. 13, 188–196 (2022). https://doi.org/10.1007/s12975-021-00918-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12975-021-00918-0