Abstract
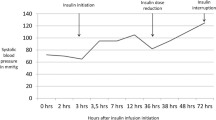
The objective of this case is to describe the pharmacokinetics and toxicity of midodrine in overdose. A 20 year old female ingested up to 350 mg midodrine while recovering in hospital from another overdose. She developed vomiting and severe hypertension (blood pressure [BP], 210/100 mmHg). Remarkable findings included a heart rate with a range of 43–60 beats/min, spontaneous respirations (20 breaths/min), and oxygen saturations of >95 % on FiO2 25 %, and a GS of 8. She was admitted to intensive care and had a normal non-contrast CT brain. She was treated with a glyceryl trinitrate patch (5 mg) and observed for 36 h with subsequent BP reduction to 124/81 mmHg and improved in conscious state. Midodrine and desglymidodrine concentrations were measured with liquid chromatography tandem mass spectrometry and were detected with 2-h post-ingestion at concentrations of 158.4 and 169.7 ng/mL, respectively. The parent drug concentrations rapidly decreased with an elimination of half-life of 1.6 h, and the metabolite initially increased and then decreased. The peak in blood pressure appeared to coincide with peak metabolite concentrations. Midodrine in overdose can potentially cause severe hypertension and reflex bradycardia but given its short half-life treatment with vasodilator agents and supportive care is sufficient.

Similar content being viewed by others
References
Jankovic J, Hiner B, Brown D, Rubin M. Neurogenic orthostatic hypotension: a double-blind placebo-controlled study with midodrine. Am J Med. 1993;95:38–48.
Izcovich A, Malla C, Manzotti M, Catalano H, Guyatt G. Midodrine for orthostatic hypotension and recurrent reflex syncope: a systematic review. Neurology. 2014;83:1170–7.
Perazella M. Efficacy and safety of midodrine in the treatment of dialysis-associated hypotension. Expert Opin Drug Saf. 2003;2:37–47.
Ward C, Gray J, Gilroy J, Kenny R. Midodrine: a role in the management of neurocardiogenic syncope. Heart. 1998;79:45–9.
Zachariah P, Moyer T, Fealey R. Pharmacodynamics of midodrine, an antihypotensive agent. Clin Pharmacol Ther. 1986;39:586–91.
Kaufmann H, Saadia D, Voustianiouk A. Midodrine in neutrally mediated syncope: a double blind, randomized, crossover study. Ann Neurol. 2002;52:342–5.
McTavish D, Goa K. Midodrine: a review of its pharmacologic properties and therapeutic use in orthostatic hypotension and secondary hypotensive disorders. Drugs. 1989;38:757–77.
Low P, Gilden J, Freeman R, Sheng K, McElligott M. Efficacy of midodrine vs placebo in neurogenic orthostatic hypotension. JAMA. 1997;277:1046–51.
Hofer K, Rauber-Luthy C, Kupferschmidt H, Ceschi A. Acute midodrine overdose: a case series (abstract). Clin Toxicol 2012;50:362
Olgar S, Omeroglu R. Prolonged supine hypertension due to midodrine use in an orthostatic hypotensive child. Pediatr Cardiol. 2007;28:309–10.
Vaughan C, Delanty N. Hypertensive emergencies. Lancet. 2000;356:411–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Informed consent was obtained to publish this case report.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Funding
The study was supported by the NHMRC Program Grant (1055176). GKI is supported by the NHMRC Senior Research Fellowship ID1061041; MR is supported by the NHMRC Senior Principal Research Fellowship ID1002611 and AW is supported by a NHMRC Postgraduate Research Scholarship ID1114284.
Informed Consent
Consent for publication of this case was obtained and provided to the journal in accordance with JMT policy.
Rights and permissions
About this article
Cite this article
Wong, L.Y., Wong, A., Robertson, T. et al. Severe Hypertension and Bradycardia Secondary to Midodrine Overdose. J. Med. Toxicol. 13, 88–90 (2017). https://doi.org/10.1007/s13181-016-0574-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13181-016-0574-4