Abstract
Introduction
There is limited published literature on longitudinal utilization of glucose-lowering agents (GLAs) among patients with type 2 diabetes (T2D) and cardiovascular disease (CVD or risk of CVD). This retrospective, observational study aimed to provide updated evidence on patient characteristics and utilization of GLAs among patients with T2D and CVD or risk of CVD in the United States.
Methods
This was a cross-sectional evaluation of patients with T2D aged 50–89 years with annual continuous enrolment in a Medicare Advantage and Prescription Drug plan, identified from administrative claims data (Humana Research Database). Patients with T2D and atherosclerotic cardiovascular disease (ASCVD) or heart failure (HF) (CVD cohort), or T2D and an additional CVD risk factor without pre-existing CVD (CVD risk cohort) were identified from 2015 to 2019. Patients were followed from their first observed ASCVD/HF diagnosis or CVD risk factor for each year they were continuously enrolled or until occurrence of a CVD diagnosis (CVD risk cohort only). Use of GLA classes were reported by year, cohort, and age groups (50–64 years and ≥ 65 years).
Results
The percentage of patients on sodium-glucose co-transporter-2 inhibitors (SGLT-2is), glucagon-like peptide-1 receptor agonists (GLP-1 RAs), and GLP-1 RAs with proven cardiovascular benefit, respectively, increased from 2015 to 2019 among ≥ 65 years (CVD cohort: 1.1–3.4%, 1.6–4.0%, and 1.2–3.8%; CVD risk cohort: 1.4–3.7%, 2.0–4.3%, and 1.5–4.1%); and among 50–64 years (CVD cohort: 2.6–7.3%, 4.3–10.1%, and 3.4–9.4%; CVD risk cohort: 3.3–6.8%, 4.6–9.6%, and 3.5–8.9%).
Conclusions
Although use of SGLT-2is and GLP-1 RAs increased over time, overall utilization of these agents in patients with T2D and ASCVD/HF or at risk for ASCVD/HF remained low, especially for those aged ≥ 65 years.
Plain Language Summary
Sodium-glucose co-transporter-2 inhibitors (SGLT-2is) and glucagon-like peptide-1 receptor agonists (GLP-1 RAs) are types of glucose-lowering medications for patients with type 2 diabetes (T2D). The American Diabetes Association, the American Association of Clinical Endocrinologists, and American College of Endocrinology have recommended these medications for patients who have been diagnosed with T2D and atherosclerotic cardiovascular disease or heart failure (ASCVD/HF). The purpose of this study was to find out how many patients in a US-based health insurance population with T2D and ASCVD/HF were treated with SGLT-2is, GLP-1 RAs, and other glucose-lowering medications from 2015 to 2019. Using insurance claims data, we identified 50- to 89-year-old patients with T2D and either ASCVD/HF or at least one risk factor for ASCVD/HF. We tracked the number of patients with T2D and either ASCVD/HF or ASCVD/HF risk factors who were using different glucose-lowering medications. Glucose-lowering medications were used in most patients (60–78%), but fewer than 11% of patients aged 50–64 years, and fewer than 5% of patients over 65 years of age were prescribed SGLT-2i and GLP-1 RA medications, despite clinical guidelines recommending their use for the above-mentioned indications. Increasing awareness among healthcare providers may be required to ensure patients with T2D and ASCVD/HF or ASCVD/HF risk factors are prescribed the guideline-recommended cardioprotective glucose-lowering agents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Sodium-glucose co-transporter-2 inhibitors (SGLT-2is) and glucagon-like peptide-1 receptor agonists (GLP-1 RAs) with proven cardiovascular benefit are recommended per current guidelines for patients with type 2 diabetes (T2D) and atherosclerotic cardiovascular disease (ASCVD) or heart failure (HF) or at risk for ASCVD/HF. However, published information on treatment patterns of such patients in the United States is limited. |
The aim of this study was to evaluate treatment patterns of classes of glucose-lowering agents for patients with T2D and ASCVD/HF (CVD cohort) or T2D and at risk for ASCVD/HF (CVD risk cohort) from 2015 to 2019. |
What was learned from the study? |
SGLT-2i and GLP-1 RA use was low in patients aged ≥ 65 years (CVD cohort: 1.1–3.4% and 1.6–4.0%, CVD risk cohort: 1.4–3.7% and 2.0–4.3%) and 50–64 years (CVD cohort: 2.6–7.3% and 4.3–10.1%; CVD risk cohort: 3.3–6.8% and 4.6–9.6%). |
Although the American Diabetes Association, the American Association of Clinical Endocrinologists, and the American College of Endocrinology recommend SGLT-2is and GLP-1 RAs, their use is low. |
Efforts should be made to identify the reasons for lower use and evaluate these patterns as more recent data become available. |
Introduction
In the United States (US), type 2 diabetes (T2D) accounts for ≥ 90.0% of all diabetes cases [1]. Cardiovascular diseases (CVD) such as atherosclerotic CVD (ASCVD) and heart failure (HF) are the major causes of morbidity and mortality in people with T2D [2]. Major risk factors for ASCVD and HF among individuals with T2D include hypertension, dyslipidemia, obesity, smoking, chronic kidney disease (CKD), family history of premature coronary disease, and albuminuria [2]. A recent systematic review reported that coronary heart disease, HF, and stroke affected 21.2, 14.9, and 7.6% of adults with T2D, respectively [3]. Moreover, compared to people without T2D, those with T2D had a 2.0–4.0 times higher risk for coronary heart disease and ischemic stroke and 1.5–3.6 times higher risk of mortality, resulting in reduced life expectancy [4, 5].
Large cardiovascular outcomes trials of sodium-glucose co-transporter-2 inhibitors (SGLT-2is: empagliflozin, canagliflozin, and dapagliflozin) and glucagon-like peptide-1 receptor agonists (GLP-1 RAs: liraglutide, semaglutide, dulaglutide) conducted over the past decade have demonstrated a lower risk of death from cardiovascular causes, nonfatal myocardial infarction, and nonfatal stroke among patients with T2D and high cardiovascular risk [6,7,8,9,10]. Considering this evidence, as early as 2017, the American Diabetes Association (ADA) and the American Association of Clinical Endocrinologists and American College of Endocrinology recommended using empagliflozin and liraglutide in patients with comorbid ASCVD for cardiovascular benefit, with more recent guideline updates including canagliflozin, dapagliflozin, semaglutide, and dulaglutide [11,12,13,14]. Moreover, SGLT-2is and GLP-1 RAs are currently recommended as part of glucose-lowering regimens for patients with or at risk for ASCVD, HF, and CKD, independent of a patient’s baseline glycated hemoglobin levels and use of metformin as first-line treatment [12, 13].
Despite the availability of published evidence on the cardiovascular benefits of SGLT-2is and GLP-1 RAs since 2015 and recommendations of their use in clinical guidelines since 2017, there is limited understanding of the utilization patterns of these and other classes of glucose-lowering agents (GLAs) among patients with T2D and ASCVD/HF or at risk for ASCVD/HF. Only three studies have evaluated treatment patterns for patients with T2D and ASCVD [15, 16] or HF [17] using data from 2017 or later, i.e., post ADA recommendation for SGLT-2is and GLP-1 RAs. Additionally, these studies were conducted in either newly diagnosed patients with T2D, patients with established ASCVD or HF, or over < 5 years. Therefore, the goal of the current observational, retrospective, study was to provide more recent evidence on the utilization of different classes of GLAs by each year over a 5-year period (2015–2019) in patients with T2D and existing ASCVD/HF (CVD cohort) or at risk for ASCVD/HF (CVD risk cohort) enrolled in a Medicare Advantage and Prescription Drug (MAPD) plan.
Methods
Data Source and Study Design
This retrospective, cross-sectional study used administrative claims data from the Humana Research Database (Louisville, KY) from January 1, 2015 to December 31, 2019. Humana, a large national health and wellness company, provides Medicare Advantage, a stand-alone prescription drug plan, and commercial health insurance across the US. This database contains de-identified enrolment information linked to medical (inpatient, emergency department, and outpatient); laboratory; and pharmacy claims data for individuals enrolled in Medicare or commercial health plans across the US. Some laboratory results data are available for ~ 60% of the patients. The Humana Healthcare Research Human Subject Protection Office reviewed this study and determined that it did not constitute human subject research and hence formal patient consent was not required. Only authorized employees of Humana Healthcare Research had access to de-identified, member-level data for analysis.
This study focused on patients with T2D enrolled in MAPD plans. This study included two cohorts—patients with T2D and existing ASCVD/HF (CVD cohort) and patients with T2D and at risk for ASCVD/HF (CVD risk cohort). Given the differences in treatment of older adults with T2D compared to younger adults, the study also evaluated GLA utilization by age group (50–64 years and ≥ 65 years) within each cohort.
Patient Selection
Patients with ≥ 2 claims with T2D diagnosis codes (International Classification of Diseases, Ninth Edition [ICD-9] 250.x0, 250.x2; International Classification of Diseases, Tenth Edition [ICD-10] E11; Supplementary material Table S1) on different dates during a calendar year (2015–2019) and continuous enrolment in MAPD during the evaluation calendar year were included in the study. Patients were 50–89 years at the time of identification of T2D. Individuals with claims for type 1 diabetes and/or individuals with end-stage renal disease (renal transplant or dialysis) or with evidence of stage V CKD (estimated glomerular filtration rate < 15 ml/min/1.73 m2) at any time during the study were excluded.
Individuals with T2D were assigned to the CVD cohort and CVD risk cohort on an annual calendar year basis. To be included in the CVD cohort, patients had to have ≥ 1 inpatient claim (primary) or ≥ 2 outpatient claims for ASCVD/HF diagnosis or CVD procedures (Supplementary material Table S1) in the same calendar year as the T2D diagnosis or during subsequent calendar years after the T2D diagnosis. ASCVD diagnosis included myocardial infarction, acute coronary syndrome, carotid arterial disease, transient ischemic attack, coronary artery disease, unstable angina, ischemic stroke, and peripheral artery disease. After identification and classification to the CVD cohort for a given calendar year, patients were included as part of that cohort for the subsequent years as long as they were enrolled in a MAPD plan during each calendar year.
For inclusion in the CVD risk cohort, patients were required to have evidence of risk factors for ASCVD/HF during the same calendar year as the T2D diagnosis or during subsequent years after the T2D diagnosis (Supplementary material Table S2). These risk factors included CKD, hypertension, hyperlipidemia, microalbuminuria/macroalbuminuria, obesity, and smoking. If patients in the CVD risk cohort had an ASCVD/HF diagnosis or procedure in a given year, they were excluded from the CVD risk cohort for that year as well as any subsequent years.
Variables
Baseline demographic characteristics including age, sex, race/ethnicity, geographic location, and population density were evaluated. Patients eligible for both Medicare and Medicaid (dual eligible) or eligible for low-income subsidy (Medicare beneficiaries with income below 150% of poverty and limited resources; eligible for additional premium and cost-share assistance for prescription drugs under the Medicare Part D program) were flagged.
Use of different classes of GLAs for each year over the 5-year period was reported. The classes of GLAs included biguanides, sulfonylureas, thiazolidinediones, amylin agonists, meglitinides, α-glucosidase inhibitors, dipeptidyl peptidase-4 inhibitors, insulin, SGLT-2is, and GLP-1 RAs (Supplementary material Table S3). As per the Food and Drug Administration, SGLT-2is with proven cardiovascular benefit include empagliflozin, canagliflozin, and dapagliflozin. GLP-1 RAs with proven cardiovascular benefit (liraglutide, injectable semaglutide, and dulaglutide) are considered cardioprotective GLP-1 RAs. Oral semaglutide was not marketed during the study period, and therefore use of the oral form of semaglutide was not assessed. Patients were classified as receiving medication for that class if they had at least one prescription claim for that medication at any point during the year. If patients were on medications in multiple classes, they were counted in each class.
Statistical Analysis
The proportion of patients with T2D and existing ASCVD/HF and the proportion of patients with T2D and > 1 risk factor for ASCVD/HF without evidence of ASCVD/HF diagnosis was assessed in the overall cohort. Descriptive analyses were used to characterize demographic characteristics and utilization patterns of GLAs. Means and standard deviations (SD) and median and interquartile range (IQR) were reported for continuous variables while frequencies and percentages were reported for categorical variables. Medication utilization patterns was analyzed and reported for both cohorts segmented by year and patient age (50–64 years and ≥ 65 years).
Results
After applying all inclusion and exclusion criteria, the number of patients with T2D ranged from 525,731 in 2015 to 908,153 in 2019 (Fig. 1). From 2015 to 2019, the number of patients in the CVD cohort ranged from 177,254 to 416,149 while the number of patients in the CVD risk cohort ranged from 340,885 to 485,456. The following sections report the characteristics of patients with ASCVD/HF or at-risk for ASCVD/HF among patients with T2D.
Study design and patient attrition. The figure represents the patient attrition for each year. The dotted line represents patients excluded as per the criteria each year. Patients with ASCVD/HF were included in the CVD cohort and patients at risk for ASCVD/HF were included in the CVD risk cohort. ** “prior” evaluation only applies to 2016 onwards. To identify patients with T2D in 2015, we only looked at 2015 claims. ASCVD atherosclerotic cardiovascular disease, CKD chronic kidney disease, CVD cardiovascular disease, ESRD end-stage renal disease, HF heart failure, MAPD Medicare Advantage and Prescription Drug, T1D type 1 diabetes mellitus, T2D type 2 diabetes
CVD Cohort
Demographic Characteristics
At the time of inclusion, the mean (SD) age of patients was 74.5 (6.1) years and 59.7 (3.5) years in the ≥ 65 years and 50–64 years groups, respectively. The majority of patients in the study were men, White, living in the South, and in urban areas of the US. The proportion of patients eligible for low-income subsidy/dual eligible was 21.6% and 45.3% in the ≥ 65 years and 50–64 years groups, respectively (Table 1).
Glucose-Lowering Agent Use
The use of GLAs from 2015 to 2019 ranged from 60.9 to 69.9% among patients aged ≥ 65 years, and from 71.8 to 77.1% among patients aged 50–64 years. Biguanides and sulfonylureas were commonly used in both groups, although a decline in usage from 2015 to 2019 was observed. Insulin use increased from 2015 to 2019 among patients aged ≥ 65 years (14.2–17.1%) and 50–64 years (24.4–27.3%). From 2015 to 2019, use of SGLT-2is in patients aged ≥ 65 years increased from 1.1 (2015) to 3.4% (2019), GLP-1 RA from 1.6 to 4.0%, and cardioprotective GLP-1 RA from 1.2 to 3.8%. A similar trend was observed for patients aged 50–64 years: SGLT-2i usage increased from 2.6 to 7.3%, GLP-1 RA from 4.3 to 10.1%, and cardioprotective GLP-1 RA from 3.4 to 9.4% (Fig. 2A and B).
Glucose-lowering agent use in patients aged ≥ 65 and 50–64 years with T2D and ASCVD/heart failure (CVD cohort). A, B Usage of glucose-lowering agents in patients aged ≥ 65 years and 50–64 years, respectively. Cardioprotective GLP-1 RA includes liraglutide, injectable semaglutide, or dulaglutide. Others include amylin agonists, meglitinides, and alpha-glucosidase inhibitors. Fixed-dose combinations including insulin degludec-liraglutide (subcutaneous) and insulin glargine-lixisenatide (subcutaneous) were not shown since usage was < 0.5%. ASCVD atherosclerotic cardiovascular disease, CDPT GLP-1RAs cardioprotective glucagon-like peptide-1 receptor agonists, CVD cardiovascular disease, DPP-4is dipeptidyl peptidase-4 inhibitors, GLP-1 RAs glucagon-like peptide-1 receptor agonists, SGLT-2is sodium-glucose Co-transporter-2 inhibitors, TZD thiazolidinediones
CVD Risk Cohort
Demographic Characteristics
The mean (SD) age was 72.7 (5.8) years in the ≥ 65 years group and 59.0 (3.7) years in the 50–64 years group. In both groups, most patients were female, White, living in the South, and in urban areas of the US. The proportion of patients eligible for low-income subsidy/dual eligible was 18.9% for patients aged ≥ 65 years and 43.9% for patients aged 50–64 years (Table 1).
Glucose-Lowering Agent Use
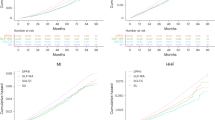
The use of GLAs ranged from 62.7 to 73.6% among patients aged ≥ 65 years, and from 71.6 to 77.9% among patients aged 50–64 years. Biguanides and sulfonylureas were commonly used in both groups, although a decline in usage from 2015 to 2019 was observed. From 2015 to 2019, use of SGLT-2is in patients aged ≥ 65 years increased from 1.4 to 3.7%, GLP-1 RA from 2.0 to 4.3%, and cardioprotective GLP-1 RA from 1.5 to 4.1%. A similar trend was observed for patients aged 50–64 years but at greater percentages. SGLT-2i usage increased from 3.3 to 6.8%, GLP-1 RA from 4.6 to 9.6%, and cardioprotective GLP-1 RA from 3.5 to 8.9% (Fig. 3A and B).
Glucose-lowering agent use in patients aged ≥ 65 and 50–64 years with T2D and risk factors for ASCVD/heart failure (CVD risk cohort). A, B Usage of glucose-lowering agents in patients aged ≥ 65 years and 50–64 years, respectively. Cardioprotective GLP-1 RA includes liraglutide, injectable semaglutide, or dulaglutide. Others include amylin agonists, meglitinides, and alpha-glucosidase inhibitors. Fixed-dose combinations including insulin degludec-liraglutide (subcutaneous) and insulin glargine-lixisenatide (subcutaneous) were not shown since usage was < 0.4%. ASCVD atherosclerotic cardiovascular disease, CDPT GLP-1RAs cardioprotective glucagon-like peptide-1 receptor agonists, CVD cardiovascular disease, DPP-4is dipeptidyl peptidase-4 inhibitors, GLP-1 RAs glucagon-like peptide-1 receptor agonists, SGLT-2is sodium-glucose Co-transporter-2 inhibitors, TZD thiazolidinediones
Discussion
The current study adds to the limited evidence on use of GLAs among patients with T2D and ASCVD/HF or with risk factors for these conditions in the US. Additionally, in line with several clinical guidelines recommending SGLT-2is and GLP-1 RAs as first-line therapy in patients with or at high risk for ASCVD/HF [12, 13], this study evaluated the usage of SGLT-2is and GLP-1 RAs with proven cardiovascular benefit over a 5-year time period.
Across both CVD and CVD risk cohorts, biguanide and sulfonylurea use reduced over time in both age groups, while SGLT-2i and GLP-1 RA use increased, probably due to greater knowledge and uptake of the latter in recent years. In the CVD cohort, use of SGLT-2i and GLP-1 RA was higher among patients aged 50–64 years than ≥ 65 years. This is consistent with Weng et al.’s 2015 study [18] wherein use among patients aged 45–64 years was higher than patients aged ≥ 65 years for both SGLT-2i (13.1 vs. 3.8%) and GLP-1 RA (10.9 vs. 4.5%). Similarly, in the CVD risk cohort, use of SGLT-2i and GLP-1 RA was also higher among patients aged 50–64 years than ≥ 65 years, which is in line with Weng et al. [18], wherein use of SGLT-2i (12.9 vs. 4.9%) and GLP-1 RA (9.8 vs. 4.9%) was higher among patients without ASCVD aged 45–64 years than ≥ 65 years in 2015.
Although we observed increased use of SGLT-2i and GLP-1 RA over the study period, overall utilization of these agents was low, particularly among the elderly. A similar trend was noted by Mahtta et al. [16] among patients with T2D and ASCVD, and by Hamid et al. [19] in a study on patients with T2D, with and without CVD. In the former, only 11.2% and 8.0% of patients received SGLT-2is and GLP-1 RAs, respectively, across 130 Veterans Affairs facilities in the US. In Hamid et al.’s study [19], expanded indications for empagliflozin and liraglutide resulted in higher new quarterly prescriptions. Primary care physicians and endocrinologists, but not cardiologists, accounted for majority of the increased prescriptions of SGLT-2is and GLP-1 RAs. Cardiologists may be hesitant to prescribe these classes as they may still consider these medications as first-line glucose-lowering agents rather than cardioprotective agents [19] and do not want to interfere with the treatment of T2D which is usually owned by the primary care physician or endocrinologist. Although our study did not evaluate the reasons for low use of SGLT-2is and GLP-1 RAs, it could be associated with the route of administration (injectable route for GLP-1 RAs), adverse effects, and relatively higher cost of these agents [20]. Adverse events such as volume depletion due to SGLT-2is also needs to be considered. Finally, these agents may not be affordable for the elderly, who may already be on multiple medications. It should also be noted that a greater proportion of adults aged ≥ 65 years in both cohorts of our study did not fill a prescription for any GLA.
Large cardiovascular outcomes trials [6,7,8,9,10] and meta-analyses [21, 22] have reported the cardiovascular benefit granted by specific SGLT-2is and GLP-1 RAs in patients with T2D who are at risk for or have ASCVD. However, the low utilization of these agents, as shown in the current study, by Mahtta et al. [16] and by Hamid et al. [19], underscores the need for changes in therapeutic strategies, wider dissemination of benefits of SGLT-2is and GLP-1 RAs, and exploration of the reasons for low use.
A major strength of this study is that it provides a snapshot of the demographic characteristics and treatment patterns of GLAs among patients with T2D with or at risk for ASCVD/HF. Moreover, this study analyzed administrative claims data of patients enrolled in a MAPD plan administered by Humana, which is one of the largest MAPD providers of health plans in the US with broad reach and enrolment across the country. However, since the study utilized data from a US Medicare population, the results may not be generalizable for younger patients enrolled in commercial plans or patients outside of the US. Additionally, administrative claims data are subject to certain limitations, such as potential errors in coding and missing data. We also could not present laboratory results in detail as these results are only available for a limited proportion of individuals in the database. Limited information was available on diagnoses that occurred before the start of the database; therefore, it was not possible to ensure patients in the CVD risk cohort had not had a CVD event before the start of the study period. Among the risk factors used to distinguish the CVD risk cohort, smoking and obesity were identified based on claims for smoking cessation products and counseling, and diagnosis codes, respectively, and hence may be underreported. We also did not consider the length of therapy while assessing the use of SGLT-2is and/or GLP-1 RAs.
Conclusions
This study provides a yearly cross-sectional view from 2015 to 2019 of the use of various classes of GLAs among patients with T2D with established ASCVD/HF or at risk for ASCVD/HF. Despite an increase in usage during the study period, the overall utilization of GLAs with proven cardioprotective benefits (SGLT-2is and GLP-1 RAs) remained low, especially in the elderly. Greater awareness among healthcare providers about recommended therapies, especially proven cardioprotective benefits of SGLT-2is and GLP-1 RAs, and addressing potential barriers to treatment can assist in cardiovascular management and improve patient outcomes among patients with T2D. As most recent guidelines further support the use of GLP-1 RAs and SGLT-2is, future studies should be conducted to evaluate the change in the usage of these medications among patients with T2D and CVD or at risk for CVD.
References
National Diabetes Statistics Report, 2020. Atlanta, GA: Centers for Disease Control and Prevention, U.S. Dept of Health and Human Services; 2020.
American Diabetes Association. 10. Cardiovascular disease and risk management: standards of medical care in diabetes-2021. Diabetes Care. 2021;44:S125–50.
Einarson TR, Acs A, Ludwig C, Panton UH. Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007–2017. Cardiovasc Diabetol. 2018;17:83.
Emerging Risk Factors Collaboration, Sarwar N, Gao P, Seshasai SR, Gobin R, Kaptoge S, et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet. 2010;375:2215–22.
Wan EYF, Chin WY, Yu EYT, Wong ICK, Chan EWY, Li SX, et al. The impact of cardiovascular disease and chronic kidney disease on life expectancy and direct medical cost in a 10-year diabetes cohort study. Diabetes Care. 2020;43:1750–8.
Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015;373:2117–28.
Marso SP, Daniels GH, Brown-Frandsen K, Kristensen P, Mann JF, Nauck MA, et al. Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2016;375:311–22.
Neal B, Perkovic V, Mahaffey KW, de Zeeuw D, Fulcher G, Erondu N, et al. Canagliflozin and cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017;377:644–57.
Marso SP, Bain SC, Consoli A, Eliaschewitz FG, Jodar E, Leiter LA, et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2016;375:1834–44.
Gerstein HC, Colhoun HM, Dagenais GR, Diaz R, Lakshmanan M, Pais P, et al. Dulaglutide and cardiovascular outcomes in type 2 diabetes (REWIND): a double-blind, randomised placebo-controlled trial. Lancet. 2019;394:121–30.
American Diabetes Association. 8. Pharmacologic approaches to glycemic treatment. Diabetes Care. 2017;40:S64–74.
American Diabetes Association. 9. Pharmacologic approaches to glycemic treatment: standards of medical care in diabetes-2020. Diabetes Care. 2020;43:S98–110.
American Diabetes Association. 9. Pharmacologic approaches to glycemic treatment: standards of medical care in diabetes-2021. Diabetes Care. 2021;44:S111–24.
Garber AJ, Handelsman Y, Grunberger G, Einhorn D, Abrahamson MJ, Barzilay JI, et al. Consensus statement by the American Association of Clinical Endocrinologists and American College of Endocrinology on the comprehensive type 2 diabetes management algorithm—2020 executive summary. Endocr Pract. 2020;26:107–39.
Koutroumpakis E, Hamden R, Deswal A, Tung P, Nambi V, Krause T, et al. Contemporary treatment patterns for newly diagnosed type 2 diabetes mellitus in patients with and without cardiovascular disease. Am College Cardiol. 2020;75:2041.
Mahtta D, Ramsey DJ, Lee MT, Chen L, Al Rifai M, Akeroyd JM, et al. Utilization rates of SGLT2 inhibitors and GLP-1 receptor agonists and their facility-level variation among patients with atherosclerotic cardiovascular disease and type 2 diabetes: insights from the Department of Veterans Affairs. Diabetes Care. 2022;45:372–80.
Vaduganathan M, Fonarow GC, Greene SJ, DeVore AD, Kavati A, Sikirica S, et al. Contemporary treatment patterns and clinical outcomes of comorbid diabetes mellitus and HFrEF: the CHAMP-HF registry. JACC Heart Fail. 2020;8:469–80.
Weng W, Tian Y, Kong SX, Ganguly R, Hersloev M, Brett J, et al. The prevalence of cardiovascular disease and antidiabetes treatment characteristics among a large type 2 diabetes population in the United States. Endocrinol Diabetes Metab. 2019;2: e00076.
Hamid A, Vaduganathan M, Oshunbade AA, Ayyalasomayajula KK, Kalogeropoulos AP, Lien LF, et al. Antihyperglycemic therapies with expansions of US food and drug administration indications to reduce cardiovascular events: prescribing patterns within an academic medical center. J Cardiovasc Pharmacol. 2020;76:313–20.
American Diabetes Association. 12. Older adults: standards of medical care in diabetes-2020. Diabetes Care. 2020;43:S152–62.
Zelniker TA, Wiviott SD, Raz I, Im K, Goodrich EL, Furtado RHM, et al. Comparison of the effects of glucagon-like peptide receptor agonists and sodium-glucose cotransporter 2 inhibitors for prevention of major adverse cardiovascular and renal outcomes in type 2 diabetes mellitus. Circulation. 2019;139:2022–31.
Pinto LC, Rados DV, Remonti LR, Viana LV, Pulz GT, Carpena MP, et al. Patient-centered management of type 2 diabetes mellitus based on specific clinical scenarios: systematic review, meta-analysis and trial sequential analysis. J Clin Endocrinol Metab. 2020;105:3588–99.
Acknowledgements
Funding
The study was sponsored by Eli Lilly and Company and conducted in partnership with Humana Inc. Eli Lilly and Company also provided the Rapid Service Fee. The analysis was conducted independently by Humana Healthcare Research, Inc.
Medical Writing, Editorial, and Other Assistance
The authors would like to thank Leo J Philip Tharappel, an employee of Eli Lilly Services India Pvt. Ltd for medical writing support.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Author Contributions
Study concept and design: Radhika Nair, Reema Mody, Maria Yu, Manige Konig, Todd Prewitt. Data curation and statistical analysis: Stuart Cowburn. Data interpretation: Radhika Nair, Reema Mody, Stuart Cowburn, Maria Yu. Writing—original draft: Reema Mody, Stuart Cowburn. Writing—review and editing: Radhika Nair, Reema Mody, Maria Yu, Stuart Cowburn, Manige Konig, Todd Prewitt.
Disclosures
Reema Mody, Maria Yu, and Manige Konig are employees and shareholders of Eli Lilly and Company. Stuart Cowburn is an employee of Humana Healthcare Research, Inc. Todd Prewitt is an employee of Humana Inc. At the time that this study was conducted, Radhika Nair was an employee of Humana Healthcare Research, Inc. She is now an employee of Sanofi.
Compliance with Ethics Guidelines
The Humana Healthcare Research Human Subject Protection Office reviewed this study and determined that it did not constitute human subject research and hence formal patient consent was not required. A formal determination letter is available upon request.
Data Availability
The datasets generated during and/or analyzed during the current study are not publicly available due to state and federal regulations and contractual obligations related to privacy.
Author information
Authors and Affiliations
Corresponding author
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Nair, R., Mody, R., Yu, M. et al. Real-World Treatment Patterns of Glucose-Lowering Agents Among Patients with Type 2 Diabetes Mellitus and Cardiovascular Disease or At Risk for Cardiovascular Disease: An Observational, Cross-Sectional, Retrospective Study. Diabetes Ther 13, 1921–1932 (2022). https://doi.org/10.1007/s13300-022-01320-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-022-01320-1