Abstract
Introduction
The objective of the present study is to describe the incidence of recently acquired hepatitis C (RAHCV) in a large cohort of people living with HIV (PLWHIV) and sexualized drug use and other related risk behaviours.
Methods
Observational study including all PLWHIV with a RAHCV episode between June 2005 and December 2019 at the Hospital Clinic of Barcelona, Spain. Incidence of RAHCV was determined per person calendar year (py) in those patients who were HCV RNA negative. Data were collected on high-risk sexual practices for HCV transmission focused on gay, bisexual and other men having sex with men (gbMSM).
Results
A total of 340 RAHCV were diagnosed in 290 PLWHIV; 274 (94%) of them were gbMSM and developed 324 RAHCV, mainly since 2010 (90%). Overall incidence rate (IR) of RAHCV in gbMSM was 0.10 py (95% CI 0.09–0.11), with a 40% decreased observed since 2017 (IR 0.06, 95% CI 0.03–0.09 in 2019). Sixty reinfections were detected in 50 gbMSM (n = 244, 20%). The overall reinfection IR was 0.17 per py (95% CI 0.12–0.23) and the proportion of reinfection among total RAHCV increased to 47% cases in 2019, mainly in patients engaged in sexualized substance use (76%), unprotected anal intercourse (94%), sex partying (80%), fisting (43%), slamming (14%) and 60% of concomitant sexually transmitted infections (STIs).
Conclusions
Despite RAHCV incidence decline in our cohort since 2017, HCV reinfection increased. High sexualized substance use and other risk behaviours are described in this context, indicating the need for public health tailored strategies to reduce this transmission and achieve HCV microelimination in gbMSM living with HIV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The present article describes our institutional experience of more than 15 years in recently acquired hepatitis C (RAHCV) among PLWHIV. |
A total of 340 RAHCV were diagnosed in 290 PLWHIV; 274 (94%) of them were gbMSM and developed 324 RAHCV, mainly since 2010 (90%). A decrease of 40% in RAHCV incidence was observed since 2017, but the proportion of reinfection among total RAHCV increased to 47% cases in 2019, mainly in patients engaged in sexualized substance use, unprotected anal intercourse, sex partying, fisting, slamming and 60% of concomitant STIs. |
Our results show the urgent need for public health tailored strategies to reduce this transmission and achieve HCV microelimination in gbMSM living with HIV. |
Digital Features
This article is published with digital features, including a summary slide, to facilitate understanding of the article. To view digital features for this article go to https://doi.org/10.6084/m9.figshare.14393888.
Introduction
In recent years, increasing evidence of sexually transmitted hepatitis C virus (HCV) infection has emerged worldwide among gay, bisexual and other men who have sex with men (gbMSM) living with HIV. Evidence is growing that the incidence of HCV infection is increasing in this group [1] but also the potential for HCV reinfection. The observed high rates of new infections have negative health consequences and compromise the efforts to limit the HCV epidemic and achieve the World Health Organization (WHO) elimination goals of reducing infections by 80% and mortality by 65% by 2030 [2].
Our centre was among the first to document the epidemic outbreak of acute hepatitis C infection among MSM living with HIV in Barcelona, Spain [3,4,5,6]. This trend has continued with the diagnosis of approximately 35 new episodes per year, of which an increasing number were reinfections. Of note, the NEAT consensus panel has recently proposed the use of the term “recently acquired hepatitis C infection” (RAHCV) to replace the term “acute hepatitis C infection” and the reasoning for the new terminology is discussed in detail in the corresponding publication [7]. In the era of expanded use of direct-acting antiviral agents (DAA) for chronic HCV infection, with the consequent decrease of HCV transmitters [8] and a global decline in HCV incidence, suggesting the effect of treatment-as-prevention strategy, is essential to expand current knowledge on HCV infection and reinfection in gbMSM living with HIV, mainly because a high incidence of HCV is still observed in this population compared to other populations [9,10,11,12].
Further, there is a need to characterize risk factors of HCV infection amongst gbMSM, and potential predictors for reinfection, with a special focus on the “chemsex” phenomenon, a subset of sexualized drug use to enhance sexual experience that emerged in modern gay culture around the world; and how the practice is impacting sex pleasure and sexual health in the community [13]. Studies have shown that people engaged in chemsex are more likely to engage in higher-risk sexual practices such as having sex with multiple partners, fisting and sharing sex toys, slamsex (injecting chemsex drugs), and to be diagnosed with concomitant sexually transmitted infections (STIs) [14,15,16,17]. This is worrisome, since all of these sexual behaviours associated with chemsex may facilitate the ongoing spread of HCV in this population [18].
The aim of the present article is to describe our institutional experience over 15 years in RAHCV among people living with HIV (PLWHIV), while highlighting the alarming incidence of reinfection, mainly in gbMSM, and the influence that sexualized drug use may have, among other vulnerability factors. A better understanding of the sexual risk factors related to HCV infection and reinfection is needed to implement public health strategies to prevent sexually transmitted HCV. To the best of our knowledge, the Hospital Clinic of Barcelona has the largest Spanish cohort of PLWHIV with almost 6000 patients on follow-up. The subset of 63% describing themselves as gbMSM is one of the largest cohorts in Europe. This centre is in an area with a large gay community, which contributes to the higher detection rate of HCV episodes among gbMSM compared with other centres.
Methods
We included all PLWHIV who were diagnosed with RAHCV between June 2005 and December 2019 at the Hospital Clinic in Barcelona, Spain. The study was approved by the Hospital Clinic Ethics Committee and all patients gave their written informed consent to use their data for health research purposes.
PLWHIV in our centre were routinely followed up every 6 months. Testing for antibodies to HCV was requested at diagnosis of HIV and then every 2 years, or more frequently (every 6 months or less) in case of high-risk HCV infection behaviours.
RAHCV was defined as positive anti-HCV IgG and a documented negative anti-HCV IgG in the previous 12 months OR positive HCV-RNA and a documented negative HCV-RNA or negative anti-HCV IgG in the previous 12 months.
In addition, patients with evidence of symptomatic infection or unexplained increase in alanine aminotransferase were examined to rule out RAHCV. If diagnosis was confirmed, patients were followed and treated as per current clinical guidelines. To estimate the date of primary infection and confirm RAHCV, all plasma samples available 12 months before diagnosis were tested for HCV antibodies and HCV-RNA. Incidence of recently acquired infection was determined each calendar year in the subgroups of patients who were HCV RNA negative, considering that subjects with a negative HCV RNA in a specific year were at risk during the whole year. Until December 2016, all RAHCV episodes were treated with peginterferon plus ribavirin. As of January 2017, patients were started on DAA regimens.
We defined spontaneous HCV clearance as at least two HCV RNA detections 12 weeks apart, without having undergone any specific HCV treatment.
HCV reinfection was defined as detectable HCV-RNA after achieving a sustained virological response (SVR) 12 weeks after the end of treatment or following a spontaneous clearance, or HCV infection with a different genotype/subtype regardless of the period. Follow-up time at-risk for reinfection started at the end of HCV treatment for patients achieving SVR, and at the time of the second negative HCV-RNA for patients who spontaneously cleared their infection. And it ended when a reinfection was detected or on the last visit, whichever occurred first.
Data Collection
To screen HCV-infected patients, available plasma samples were tested for anti-HCV antibodies using the third-generation ADVIA Centaur HCV assay (Siemens Healthcare Diagnostics Inc. Tarrytown, NY 10591-5097, USA). Detection of HCV-RNA was performed with the Siemens VERSANT or the Roche Cobas® 6800 since 2017, both with a lower limit of quantification of 15 IU/mL to an upper limit of 1.0E + 08 IU/mL (linear range). A real-time RT-PCR by restriction fragment length polymorphism (RFLP) was used to determine HCV genotypes.
Data on patient demographics, concomitant STIs, HCV infection, treatment history, symptoms, and virological and biochemical parameters were recorded. We also collected known risk behaviours for HCV transmission such as high-risk sexual practices (unprotected anal intercourse, fisting, sharing of sex toys, frequent casual sex with different partners) and substance use in sexual context, including slam practices of injecting drug during sex.
Statistical Analysis
Socio-demographic, clinical and risk behaviour data were summarized using descriptive statistics. Quantitative variables were described with measures of central tendency and dispersion [mean (standard deviation), or median (interquartile range)], and qualitative variables with absolute (n) and relative (%) frequencies. Incidence of HCV infection and reinfection and 95% confidence intervals (CIs) were estimated using a Poisson regression model. Incidence rate ratio (IRR) was used to compare incidence rate (IR) between different periods. Data about sexual behaviour in gbMSM were available for the period 2018–2019, and associated risk factors were compared between individuals with acute HCV infection and those with reinfection using Fisher’s exact test or chi-square test. All tests were two-tailed with a significance level of 0.05. Statistical analyses were conducted using Stata (StataCorp. 2017. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC).
Results
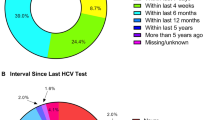
Between June 2005 and December 2019, a total of 340 episodes of RAHCV were diagnosed in 290 PLWHIV, most of them (305 [90%] episodes in 256 patients) from 2010 onwards. Overall, 274 (94%) patients were gbMSM (median age of 39 years) and 4 (1.4%) people who inject drugs (PWID) out of sexual context. Of the 324 episodes reported within the cohort of 274 gbMSM, 293 episodes (90%) in 244 patients were reported from 2010 onwards (Fig. 1a). The overall IR of RAHCV in gbMSM was 0.09 (95% CI 0.08–0.10) during the study period and 0.10 (95% CI 0.09–0.11) from 2010 to 2019. Interestingly, the RAHCV IR decreased by 40% from 2017 (0.10, 95% CI 0.07–0.14) to 2019 (0.06, 95% CI 0.03–0.09), with an IRR of 0.60 (95% CI 0.34–1.07), coinciding with the introduction and generalization of DAA treatment. The main characteristics of RAHCV episodes and prescribed HCV treatment are shown in Table 1.
Information on recreational drug use was available for 85 of the 293 episodes (29%) diagnosed in gbMSM from 2010, of which 62 (73%) were diagnosed in a period of drug use during sex, mainly cocaine (30, 48%), GHB/GBL (30, 48%), methamphetamine (30, 48%), poppers (33, 53%), erection-enhancing medication (17, 27%), mephedrone (14, 23%) and ecstasy/MDMA (13, 21%). Sixty-five of these 293 episodes (22%) occurred concomitantly with other STIs, mainly syphilis (46, 71%), but also condyloma/human papillomavirus (HPV) (18, 28%), chlamydia and chlamydia/lymphogranuloma venereum (LGV) (14, 22%).
Hepatitis C Virus Reinfection
Of the 244 gbMSM diagnosed with HCV from 2010, 60 episodes of HCV reinfection were detected in 50 patients (20%), with an overall reinfection rate of 0.17 per patient year of follow-up (py) (95% CI 0.12–0.23). Patients with reinfections were all male and none of them self-described as PWID. The median age of these patients was 44 years (range 38–49). The main characteristics of reinfections and prescribed therapy are given in Table 2.
In 41 of 54 episodes of reinfection with available information on the use of recreational drugs, patients reported having chemsex (76%), especially with cocaine (49%), gamma-hydroxybutyrate/gamma-butyrolactone (GHB/GBL) (44%), methamphetamine (39%) and poppers (61%) (Table 3). The median number of sexual partners reported in the last month in 18 episodes of reinfections was 6.5 (range 3–34). Regarding sexual practices, in 48 cases (94%) of reinfection, patients acknowledged engaging in unprotected anal intercourse, 13 (43%) fisting, 33 (80%) sex partying and 6 (14%) slamming (Table 3). Second, third and fourth reinfections were detected in five, two and two patients, respectively, and the incidence of second infection was 0.09 per py (95% CI 0.03–0.15) and the incidence of third infection 0.11 per py (95% CI 0.04–0.17). All cases of second and third reinfections occurred in gbMSM who reported unprotected anal intercourse.
Before 2018, the yearly proportion of reinfection among the RAHCV infections ranged from 5% to 32%, while in 2019 it increased to 47% despite a lower number of RAHCV cases diagnosed in that year (Fig. 1b). Table 4 compares sexual behaviour risk factors between patients with new RAHCV and those with reinfection diagnosed in 2018 and 2019. A higher proportion, although not significant, of gbMSM with reinfection reported high-risk sexual practices such as fisting (67%) and slamming (23%), compared to those with new infections (50% and 15%, respectively). Drugs used for chemsex did not vary significantly, but STIs were reported significantly more often by gbMSM with reinfection (10% vs 53%; p = 0.0019) (Table 4).
Discussion
This study shows that the incidence of RAHCV infection among HIV-positive gbMSM in our cohort of PLWHIV in Barcelona was substantially high, especially from 2010 onwards, which is consistent with the increasing trends seen worldwide over the last decade [19,20,21,22,23,24].
However, the 40% decline in the cases of RAHCV infections in our cohort from 2017 to 2019 is remarkable and comparable to the 49%, 51% and 61% decrease in HCV incidence described in a real-life cohort in Switzerland [10] and two real-life cohorts in the Netherlands [9, 25], respectively; but lower than that reported by Garvey et al. in UK [26], with a 78% decline for first HCV episode and 68% decline in overall HCV incidence. Similarly, HCV viraemic prevalence declined from 82% in 2014 to 8% in 2018 in the Australian CEASE cohort study [27]. All these findings are coincident with the introduction and generalization of DAA use, which supports the efficacy of generalized hepatitis C treatment as a prevention strategy for new HCV infections by reducing virus circulation within the gbMSM population. In relation to the time we take to treat patients from diagnosis, as can be observed, in general it is a short time, being the shortest time after 2017, when treatment in Spain with DDA was generalized, regardless of the degree of fibrosis or the time of diagnosis. Therefore, we do not think that reinfections or not new episodes may be due to untreated patients who remain viraemic.
In contrast to the decline of RAHCV, an increased rate of reinfection was observed at the end of the study period (2019), which reflects the heterogeneous risk of HCV infection and reinfection in this population [20]. The number of reinfections reported in our single centre study is high compared to those of recent large multicentre cohort studies in other regions of Europe. In our centre, 60 reinfections were detected in 244 gbMSM (24.5%). In the region of Madrid (Madrid CoRE cohort), reinfections were detected in 6.8% of gbMSM during the period 2014–2017 [11], while in Germany (GECCO cohort), 14.7% of MSM had become reinfected between 2014 and 2018 [12]. The MOSAIC cohort in the Netherlands showed the highest incidence rate in gbMSM among these multicentre cohorts (38.5 per 1000 py between 2000 and 2019 [95% CI 33.9–43.7] and declining to 11.4 per 1000 py in 2019) [9]. Similar findings were reported in the UK study by Garvey et al. [26]. In contrast, the Australian CEASE cohort study only describes five reinfections in the period studied (2014–2017) [27]. One of the potential reasons for this low incidence is that 81% of the patients included in the CEASE cohort were PWID, showing an epidemiological scenario different from ours. The overall reinfection incidence after SVR of 0.17 per py in our study, which is approximately twice that of the Madrid-CoRe estimate (0.06 per py) [11] in the same setting of higher risk-taking behaviours, highlights the need for more effective application of risk-reducing strategies in our population.
The lack of PWID becoming reinfected in our cohort demonstrates the ongoing risk of repeated HCV transmission in gbMSM who engage in high-risk sexual practices and sexualized substance use [9, 11, 12, 18, 28]. The published information about specific risk factors associated with reinfection among MSM is scarce [12, 28]. Recently, the MOSAIC cohort [18] in a smaller group of patients in the Netherlands found an association between some sexual practices, such as receptive condomless anal intercourse, sex toy sharing, group sex, or at least 10 casual sex partners in the last 6 months, and reinfection. In our study almost all reinfections occurred during unprotected anal intercourse, chemsex, and sex toy sharing, as reported elsewhere [11, 18]. When we compare the reinfections and the new episodes that occurred in the last 2 years of our study, patients with reinfection presented a significantly higher proportion of STIs, and a higher non-significant trend of high prevalence of sexualized substance use, included slamming. The percentage of gbMSM practicing slam in our study (14%) was lower than that observed in Madrid-Core (33%) [11], reflecting the different epidemiological profiles of chemsex between studied cohorts and the dynamic and changing nature of the phenomenon.
Chemsex culture is spreading among gbMSM [15, 16] and had an impact on both new infections and reinfection episodes in our study. Chemsex practice is likely an indicator of the type of setting where sexual behaviours associated with HCV take place, and we found a high prevalence in our cohort in new RAHCV and reinfection episodes. Unlike other studies, we asked specifically about the use of individual chemsex drugs and found a very common use of poppers, cocaine, methamphetamine and GHB/GBL. These results differ slightly from those observed in other countries and other Spanish regions, where mephedrone was one of the main sexualized drugs among MSM [29, 30], and demonstrate the dynamic nature and cultural variation of chemsex phenomenon, a fact that has to be taken into account when designing specific prevention strategies [31]. The social and personal factors involved in chemsex are as diverse as the barriers to reduce HCV-related sexual risk behaviour in this population, including social pressure, and HCV-HIV and drug consumption stigma [32]. This points to the importance of thorough characterization of risk factors in patients attending our clinics to offer effective prevention interventions. Chemsex and high-risk sexual practices are likely the current barriers to HCV elimination in our setting. The decline in prevalence of chemsex over time among MSM observed in the AURAH2 study, which has been attributed to the participation of specialized centres for chemsex support [33], is a reflection on the effectiveness of tailored prevention strategies.
Our population does not appear to be at elevated risk of subsequent reinfection, with a second reinfection incidence that is twofold lower than the first.
Another interesting scenario that we will have to assess for HCV microelimination in our setting will be in MSM users of HIV pre-exposure prophylaxis (PrEP). The approval of the use of PrEP by the Spanish national health system is effective from November 2019. Currently in our hospital we have more than 250 users in follow-up. We will have to closely monitor what happens with this group, especially with PrEP users who present a risk profile for hepatitis C similar to the one described in our work.
The strengths of this study include a large real-life cohort in a single centre, thus minimizing variations in clinical practice, and the information provided on drug use and risk behaviours of a reinfection sample size that is larger than in other published studies. The information generated can be extrapolated and used in other medical centres of European cities with an important gay community similar to that of our centre. The study has some limitations, including its descriptive and retrospective nature and the fact that the risk of determinants for HCV infection was not analysed. Therefore, conclusions on risk factors in patients with a single episode of RAHCV versus those who became reinfected over the studied period cannot be drawn; being aware of this will aid us in designing a prospective study addressing the weakness of this analysis. Nonetheless, this study defines factors associated with a higher risk of HCV infection and reinfection to anticipate new RAHCV episodes. The magnitude of recreational drug use during sex and sexual risk-taking behaviours in gbMSM, as well as the increased prevalence of STIs, must be kept in mind when designing public harm-reduction and prevention approaches in this population. Moreover, screening strategies for STIs and frequent testing for HCV-RNA in high-risk groups should be promoted to ensure diagnosis and early treatment.
In conclusion, despite the decline in the incidence of HCV episodes observed in our cohort, HCV reinfection has increased in recent years in gbMSM living with HIV, indicating the high risk for HCV transmission in this population. The high frequency of chemsex use and other sexual risk-taking behaviours demand tailored public health harm-reduction interventions.
Change history
16 February 2022
A Correction to this paper has been published: https://doi.org/10.1007/s40121-022-00601-3
References
Martin TCS, Rauch A, Salazar-Vizcaya L, Martin NK. Understanding and addressing hepatitis C virus reinfection among men who have sex with men. Infect Dis Clin North Am. 2018;32:395–405.
Global Hepatitis Programme. Global health sector strategy on viral hepatitis 2016–2021. 2016. https://www.who.int/hepatitis/strategy2016-2021/ghss-hep/en/. Accessed Jan 2021.
Laguno M, Martínez-Rebollar M, Perez I, et al. Low rate of sustained virological response in an outbreak of acute hepatitis C in HIV-infected patients. AIDS Res Hum Retroviruses. 2012;28(10):1294–300.
Martínez-Rebollar M, Mallolas J, Pérez I, et al. Acute outbreak of hepatitis C in human immunodeficiency virus-infected patients. Enferm Infecc Microbiol Clin. 2015;33(1):3–8.
Caro-Pérez N, Martínez-Rebollar M, Gregori J, et al. Phylogenetic analysis of an epidemic outbreak of acute hepatitis C in HIV-infected patients by ultra-deep pyrosequencing. J Clin Virol. 2017;92:42–7.
Laguno M, Martínez-Rebollar M, de la Mora L, Pérez-del-Pulgar S, Mallolas J. Barriers to hepatitis C virus elimination in MSM living with HIV: the high risk of reinfection. Case study: a patient with 6 episodes. Gastroenterol Hepatol. 2019;42(9):555–6.
European Treatment Network for HIV, Hepatitis and Global Infectious Diseases (NEAT-ID) Consensus Panel. Recently acquired and early chronic hepatitis C in MSM: Recommendations from the European treatment network for HIV, hepatitis and global infectious diseases consensus panel. AIDS. 2020;34(12):1699–1711.
Falade-Nwulia O, Suarez-Cuervo C, Nelson DR, Fried MW, Segal JB, Sulkowski MS. Oral direct-acting agent therapy for hepatitis C virus infection: a systematic review. Ann Int Med. 2017;166:637–48.
Smit C, Boyd A, Rijnders BJA, et al. HCV micro-elimination in individuals with HIV in the Netherlands 4 years after universal access to direct-acting antivirals: a retrospective cohort study. Lancet HIV. 2021;8(2):e96–105.
Braun DL, Hampel B, Martin E, et al. High number of potential transmitters revealed in a population-based systematic hepatitis C Virus RNA screening among human immunodeficiency virus-infected men who have sex with men. Clin Infect Dis. 2019;68(4):561–8.
Berenguer J, Gil-Martin Á, Jarrin I, et al. Reinfection by hepatitis C virus following effective all-oral direct-acting antiviral drug therapy in HIV/hepatitis C virus coinfected individuals. AIDS. 2019;33(4):685–9.
Ingiliz P, Wehmeyer MH, Boesecke C, et al. Reinfection with the hepatitis C virus in men who have sex with men after successful treatment with direct-acting antivirals in Germany: current incidence rates, compared with rates during the interferon era. Clin Infect Dis. 2020;71(5):1248–54.
Forum EC. European chemsex forum: Fo. 2018; https://ihp.hiv/chemsex-position-paper/. Accessed Jan 2021.
Daskalopoulou M, Rodger A, Phillips AN, et al. Recreational drug use, polydrug use, and sexual behaviour in HIV-diagnosed men who have sex with men in the UK: results from the cross-sectional ASTRA study. Lancet HIV. 2014;1(1):e22-31.
Hegazi A, Lee MJ, Whittaker W, et al. Chemsex and the city: sexualised substance use in gay bisexual and other men who have sex with men attending sexual health clinics. Int J STD AIDS. 2017;28(4):362–6.
Page EE, Nelson M. Hepatitis C and sex. Clin Med (Lond). 2016;16(2):189–92.
Pakianathan M, Whittaker W, Lee MJ, et al. Chemsex and new HIV diagnosis in gay, bisexual and other men who have sex with men attending sexual health clinics. HIV Med. 2018;19(7):485–90.
Newsum AM, Matser A, Schinkel J, et al. Incidence of HCV reinfection among HIV-positive MSM and its association with sexual risk behavior: a longitudinal analysis. Clin Infect Dis. 2020. https://doi.org/10.1093/cid/ciaa645.
Pradat P, Huleux T, Raffi F, et al. Incidence of new hepatitis C virus infection is still increasing in French MSM living with HIV. AIDS. 2018;32(8):1077–82.
Pradat P, Pugliese P, Poizot-Martin I, et al. Direct-acting antiviral treatment against hepatitis C virus infection in HIV-infected patients—“En route for eradication”? J Infect. 2017;75(3):234–41.
van Santen DK, van der Helm JJ, Del Amo J, et al. Lack of decline in hepatitis C virus incidence among HIV-positive men who have sex with men during 1990–2014. J Hepatol. 2017;67(2):255–62.
Ingiliz P, Martin TC, Rodger A, et al. HCV reinfection incidence and spontaneous clearance rates in HIV-positive men who have sex with men in Western Europe. J Hepatol. 2017;66(2):282–7.
van de Laar T, Pybus O, Bruisten S, et al. Evidence of a large, international network of HCV transmission in HIV-positive men who have sex with men. Gastroenterology. 2009;136(5):1609–17.
Salazar-Vizcaya L, Kouyos RD, Zahnd C, et al. Hepatitis C virus transmission among human immunodeficiency virus-infected men who have sex with men: modeling the effect of behavioral and treatment interventions. Hepatology. 2016;64(6):1856–69.
Boerekamps A, van den Berk GE, Lauw FN, et al. Declining Hepatitis C Virus (HCV) incidence in Dutch human immunodeficiency virus-positive men who have sex with men after unrestricted access to HCV therapy. Clin Infect Dis. 2018;66(9):1360–5.
Garvey LJ, Cooke GS, Smith C, et al. Decline in hepatitis C virus (HCV) incidence in men who have sex with men living with human immunodeficiency virus: progress to HCV microelimination in the United Kingdom? Clin Infect Dis. 2021;72(2):233–8.
Martinello M, Yee J, Bartlett SR, et al. Moving towards hepatitis C microelimination among people living with human immunodeficiency virus in Australia: the CEASE study. Clin Infect Dis. 2020;71(6):1502–10.
Young J, Rossi C, Gill J, et al. Risk factors for hepatitis C virus reinfection after sustained virologic response in patients coinfected with HIV. Clin Infect Dis. 2017;64(9):1154–62.
Blomquist PB, Mohammed H, Mikhail A, et al. Characteristics and sexual health service use of MSM engaging in chemsex: results from a large online survey in England. Sex Transm Infect. 2020;96(8):590–5.
González-Baeza A, Dolengevich-Segal H, Pérez-Valero I, et al. Sexualized drug use (chemsex) is associated with high-risk sexual behaviors and sexually transmitted infections in HIV-positive men who have sex with men: data from the U-SEX GESIDA 9416 study. AIDS Patient Care STDS. 2018;32(3):112–8.
Maxwell S, Shahmanesh M, Gafos M. Chemsex behaviours among men who have sex with men: a systematic review of the literature. Int J Drug Policy. 2019;63:74–89. https://doi.org/10.1016/j.drugpo.2018.11.014.
Lambers F, Van Der Veldt W, Prins M, Davidovich U. Changing the odds: motives for and barriers to reducing HCV-related sexual risk behaviour among HIV-infected MSM previously infected with HCV. BMC Infect Dis. 2018. https://doi.org/10.1186/s12879-018-3571-1.
Sewell J, Cambiano V, Speakman A, et al. Changes in chemsex and sexual behaviour over time, among a cohort of MSM in London and Brighton: findings from the AURAH2 study. Int J Drug Policy. 2019;68:54–61. https://doi.org/10.1016/j.drugpo.2019.03.021.
Acknowledgments
Funding
This work was supported by a grant from the Spanish Ministry of Economy, Industry and Competitiveness (grant contract PI18/00583). Source of funding for the journal’s Rapid Service Fee is supported by this specific grant.
The medical writing assistance for this manuscript was funded by AbbVie in the context of a contract of service. AbbVie did not select authors for participation in the manuscript. No payments were made to the authors for the development of this manuscript either. The authors maintained complete control over the manuscript content, and it reflects their opinions. AbbVie did not review the final manuscript draft for scientific accuracy, and was not involved in methodology, data collection and analysis, or drafting.
Medical Writing and Editorial Assistance
Writing and editorial assistance was provided partially by Isabel Caballero, of Dynamic Science S.L., Spain, and was funded by AbbVie.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article.
Authorship Contributions
M.M.R., L.D.M., B.C., M.C. M.L. and A.B. collected the data. M.M.R., E.D.L., J.M., X.F. and M.L. analyzed and interpreted the data. M.M.R., L.D.M. and M.L. were involved in drafting the manuscript. B.T., A.G.C., A.I., J.A., E.M. J.B. and J.L.B. recruited patients to the study. M.L. and J.M. contributed equally. All authors contributed to the reviewing of the article and have given final approval of the version to be published.
Disclosures
María Martínez-Rebollar, Lorena De La Mora and Berta Torres have received fees for lectures from Gilead, MSD, ViiV, AbbVie and Janssen-Cilag. Ana González-Cordón has received fees for lectures and advisory board from Gilead, MSD, ViiV, AbbVie and Janssen-Cilag. Alexy Inciarte has received educational grants from MSD and Gilead. Juan Ambrosioni has participated in advisory boards and received consultancy honoraria and research grants from Gilead Sciences, Janssen Pharmaceuticals, and ViiV Healthcare, all outside of this work. Esteban Martínez has received honoraria for lectures or advisory boards from Gilead and Janssen and his institution has received research grants from MSD and ViiV. José Luís Blanco has received honoraria for lectures or advisory boards from Gilead, Janssen, MSD. Xavier Forns has served as an advisor for Gilead and AbbVie. Jordi Blanch has received honoraria for lectures or advisory boards from Ferrer Internacional, Gilead, Janssen, MSD and ViiV. Josep Mallolas has received honoraria, speaker and consultancy fees or funding for research from MSD, Roche, Boehringer-Ingelheim, ViiV, Gilead, Janssen, BMS, AbbVie. Montserrat Laguno received fees to give lectures from Gilead, MSD, ViiV, AbbVie and Janssen-Cilag. The authors have no other relevant affiliations or financial involvement with any organization or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed. Miriam Campistol, Bruno Cabrera, Albert Bagué and Elisa De Lazzari have nothing to disclose.
Compliance with Ethics Guidelines
The study was approved by the Hospital Clinic Ethics Committee and all patients gave their written informed consent to use their data for health research purposes.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Martínez-Rebollar, M., De La Mora, L., Campistol, M. et al. Impact of Sexualized Substance Use and Other Risk Practices on HCV Microelimination in gbMSM Living with HIV: Urgent Need for Targeted Strategies. Results of a Retrospective Cohort Study. Infect Dis Ther 10, 1253–1266 (2021). https://doi.org/10.1007/s40121-021-00448-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-021-00448-0