Abstract
Knee osteoarthritis (OA) is a chronic musculoskeletal condition that imposes a significant personal and societal burden worldwide. Contemporary management of the condition involves a range of non-pharmacological conservative rehabilitation strategies. Exercise, in particular, is integral for patients with knee OA. However, there has also been increasing interest in the role of gait retraining, footwear and insoles for managing knee OA because of their biomechanical effects at the knee joint and potential for altering disease progression. This review will highlight recent research findings and trends in these areas of exercise, gait retraining, footwear and insoles for managing knee OA.
Similar content being viewed by others
Introduction
Knee osteoarthritis (OA) is a chronic joint disorder that primarily affects older people. As there is no cure for OA, contemporary management of the condition aims to reduce pain, improve function and enhance quality-of-life whilst minimising progression of disease over time. Clinical guidelines recommend a range of non-pharmacological conservative interventions that may assist in the rehabilitation of people with knee OA. Importantly, such interventions are considered the first-line approach to disease management and, in particular, exercise is considered an integral component of conservative management of knee OA. However, over recent years there has also been a rapid increase in interest in the use of other conservative management strategies for knee OA, such as gait retraining, footwear and insoles (foot orthoses), given the potential for these treatments to influence disease course. This review will highlight recent research findings and trends in the areas of exercise, gait retraining, footwear and insoles for managing knee OA.
Exercise is Integral in Managing Knee OA
Exercise is essential for all patients with knee OA, irrespective of radiographic disease severity, age, co-morbidity, pain severity or physical disability. Meta-analyses demonstrate small to moderate effect sizes with exercise for pain and function [1], similar to those achieved with analgesics and non-steroidal anti-inflammatory drugs [2]. More recently, a meta-analysis conducted specifically in patients awaiting knee joint replacement surgery found moderate quality evidence that a pre-operative exercise program reduced pain [3•], providing evidence of beneficial outcomes for exercise even in people with severe osteoarthritic disease.
Consistent with the research findings, clinical guidelines unanimously recommend exercise as a core management strategy for knee OA [2, 4, 5]. The importance of exercise has been further reinforced in the most recent guidelines published in April 2012 from the American College of Rheumatology (ACR), which were developed on the basis of a systematic literature review (conducted up to the end of the third quarter in 2009) and expert opinion. These guidelines strongly recommend that all patients with symptomatic knee OA be enrolled in an exercise program commensurate with their ability to perform these activities [6••]. However, due to a lack of quality evidence, there are currently still no specific recommendations as to the intensity of the program or the number of treatments required to optimize clinical outcomes from exercise.
With regards to specific exercise prescription principles, an individualised approach is required. Both aquatic and land-based exercises are strongly recommended in the ACR clinical guidelines, and the decision on the choice of exercise approach should be based on patient preferences and the functional ability to perform the exercises [6••]. This recommendation is supported by a recent meta-analysis that found comparable clinical outcomes in 10 randomised controlled trials (RCTs) comparing land and aquatic exercise in adults with arthritis [7]. Similarly, different types of land-based exercise appear to be equally effective. Although it has been previously proposed that adding agility and perturbation training to standard exercise programs may improve outcomes in people with knee OA, this was not supported by the results of a recent large RCT involving 183 people with a 12-month follow-up published in 2011 [8•].
A recent update of Dutch physiotherapy practice guidelines for management of knee OA stated that exercise programs should comprise at least muscle strengthening exercises, exercises to improve aerobic capacity, functional exercises, and gait training, either as standalone treatments or combined with each other, depending on treatment goals [9]. Furthermore, it has been recommended that all exercise programs for knee OA should focus on limitations of activities and restrictions in participation based on the International Classification of Functioning, Disability and Health (ICF) Core Set for OA [10].
While the short-term benefits of exercise are well established, an understanding of the longer-term effects of exercise as well as its cost-effectiveness, is important to help inform clinical practice. A recent RCT has contributed to current knowledge in this area. In a pragmatic cluster RCT in 418 people with chronic knee pain [11], long-term clinical and cost benefits were found 30 months after the completion of a rehabilitation program that combined self-management and exercise. The authors reported improvements in symptoms, as well as reductions in community-based health care costs, medication costs, and total health and social care costs, compared to usual care. The cost-effectiveness of this program supports the cost savings reported in the limited number of exercise studies identified in a recent systematic review of cost-effectiveness of nonpharmacological, nonsurgical interventions for hip and knee OA [12]. Despite these initial positive findings, the review recommended that more high-quality economic evaluations are needed.
Recent exercise research has also focused on the role of exercise in weight loss for overweight and obese people with knee OA. Published in 2011, Ottawa Panel Guidelines specifically for overweight or obese people with OA demonstrate that a combination of physical activity (aerobic exercise with or without strength training) and dietary modification produce the most beneficial results compared with either intervention alone or education control on a range of clinical outcomes [13]. The panel recommends weight loss prior to implementing weight-bearing exercise to maintain joint integrity. Given that a recent longitudinal study found significant weight loss is accompanied by loss of leg muscle tissue and strength, it is logical that strengthening exercise be undertaken alongside weight loss strategies [14].
Exercise is under-utilized as a treatment strategy for OA. A recent systematic review found that although 99 % of general practitioners agreed that exercise should be used for chronic knee pain/knee OA and had provided advice or referred to a physiotherapist at some stage, up to 29 % believed that rest was the optimum management approach [15]. The frequency of actual provision of exercise advice or physiotherapy referral was lower. Another study evaluating the quality of non-pharmacological care received by 700 people with knee OA in the community found that advice on exercise was suboptimal and does not seem to be provided equally across age, sex, disability and education levels [16]. For example, a higher likelihood of receiving exercise advice was associated with having a university degree compared to a high school diploma, while receiving weight-loss advice was more likely to occur in female patients. Given the consistent benefits of exercise on clinical outcomes, research is urgently needed to identify barriers to exercise prescription by health professionals and to improve uptake and maintenance of exercise in patients.
In addition to symptomatic benefits of exercise in knee OA, there is continued interest into whether exercise may have disease-modifying effects. A recent systematic review evaluated relationships between physical activity and individual joint structures at the knee in people both with and without OA [17]. It found that the nature of the relationships depended on the specific joint structure. For example, when quantifying radiographic images there was strong evidence for a positive association between physical activity and tibiofemoral osteophytes, and strong evidence for no association with joint space narrowing. However, when using magnetic resonance imaging (MRI), there was limited evidence that greater physical activity was associated with increased cartilage volume and decreased cartilage defects. These MRI findings would suggest that physical activity is beneficial to structural joint health. However, in people with established knee OA, the limited number of clinical trials directly evaluating exercise effects on structural progression have not found any disease-modifying effect [18–20]. Similarly, a recent RCT with 54 female patients with knee OA, showed that a 6-month high-intensity progressive lower limb resistance training program did not reduce the knee adduction moment (KAM), an indirect measure of compartment-specific knee load, compared to a sham exercise program [21]. This lack of effect of exercise on knee load is consistent with previous RCTs evaluating quadriceps [22] and hip muscle [23] strengthening in people with knee OA. Thus, while exercise can reduce symptoms, there is currently little evidence to suggest that exercise can be disease-modifying in people with knee OA.
Gait Retraining—A Potential Strategy to Slow Disease Progression?
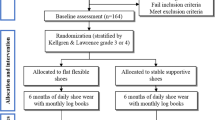
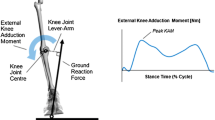
Emerging research suggests that gait retraining may offer potential benefits for people with knee OA by reducing compressive joint loads during weight-bearing activities. In the absence of a cure, interventions aimed at reducing joint loads are advocated for knee OA because of the integral role excessive loading plays in the pathogenesis of OA [24]. For research purposes, knee load is most commonly measured indirectly via three-dimensional gait analysis, and the KAM is generally accepted as a surrogate measure of medial tibiofemoral load [25]. The KAM occurs as the ground reaction force passes medial to the knee centre, thereby acting to force the tibia into a more varus position. The KAM is characterised by two peaks during the stance phase of gait (Fig. 1). In evaluating the effects of gait retraining strategies, most researchers focus on the early stance peak and/or the KAM impulse (the positive area under the KAM vs. time curve) because these two parameters have both been positively associated with an increased risk of disease progression [26, 27].
A recent systematic literature review of gait modification strategies (evaluating literature published until August 2010) identified 14 different strategies that have been evaluated for their effects on the KAM [28•]. Various gait strategies were assessed, including altering spatiotemporal characteristics (such as stride length), modification of a body segment position or motion (such as foot progression angle or trunk lean) or use of a gait aid. Reductions in the early stance peak KAM were successfully achieved with (i) use of a walking cane on the contralateral side to the diseased knee, (ii) increased lateral trunk lean, and (iii) by adopting a “medial knee thrust” gait pattern (which involves medializing the knee during the stance phase of gait). For the late stance peak KAM, altering the foot progression angle to a more toed-out position consistently reduced the late stance peak KAM in several studies. Effects of gait modifications on the KAM impulse were not assessed in all studies, however reductions were identified when participants walked with shorter stride lengths, with increased toe-out or with medial knee thrust gait. Importantly, three gait modification strategies were found to increase the KAM and hence may be detrimental for people with medial knee OA. The strategies, which increased knee load, were cane use on the ipsilateral side of the diseased knee, use of Nordic walking poles, and Tai-Chi gait.
Achievement of significant reductions in knee load may require very large and unfeasible modifications to gait. Consequently, researchers have hypothesised that summation of several gait modification strategies may yield large reductions in knee load with modest variations in gait. The effect of combining toe-out, trunk lean and medial knee thrust gait patterns was recently investigated in a study of nine healthy subjects [33]. Participants were provided with haptic biofeedback and encouraged to alter their toe-out angle to 13–25 % higher than natural, increase their lateral trunk lean to 7–17° from vertical and increase their tibial angle by 13–25° to obtain the target 30 % reduction in the early stance peak KAM. Although promising, results from this study require confirmation in people with knee OA.
Use of a walking cane is conditionally recommended in the newest ACR clinical guidelines for knee OA [6]. However, the biomechanical and symptomatic effects of canes in people with knee OA have only recently been investigated. Use of a cane in the contralateral hand was evaluated in a study of 23 participants with medial knee OA [34] and reductions in KAM parameters of 6–17 % were found. Participants achieved greatest knee offloading when greater magnitudes of body weight were placed through the cane, when they placed peak body weight through the cane earlier (rather than later) during stance, and when the cane was placed at a greater lateral distance away from the affected limb. Based on this research, appropriate training in the use of a cane should be conducted by health professionals to yield the greatest benefit for patients. The first RCT of cane use, involving 64 participants with knee OA, has only recently been published [35••]. In this study, participants were encouraged to use a cane daily over 60 days, at which point they reported average cane use of 74 min per day. Researchers found that 60 days of cane use significantly reduced pain, improved physical function and reduced analgesic medication use. Further research is now required to determine whether long-term use of a cane can have disease-modifying effects.
Role of Footwear and Insoles in the Management of Knee OA
Over recent years, there has been increasing research attention focussed on the role of nonsurgical foot interventions, such as footwear and shoe insoles, in the management of people with knee OA [36]. Given that knee OA is likely to be mechanically driven [24], and that footwear and insoles have been shown to influence knee joint loading [37••], these rehabilitation strategies may offer great potential in the management of patients with knee OA.
ACR clinical guidelines conditionally recommend medially wedged insoles for patients with valgus knee OA, based on beneficial findings regarding pain and function in a RCT and a single systematic review [38, 39]. Given that no new research regarding medial-wedged insoles for knee OA has been published recently, the ACR recommendations regarding this orthotic intervention reflects the body of knowledge as it currently stands.
In contrast to OARSI and EULAR guidelines which suggested that laterally wedged insoles could benefit people with medial knee OA [2, 4, 5], the ACR guidelines were unable to form a recommendation regarding the use of lateral-wedge insoles [6]. The American Academy of Orthopaedic Surgeons (AAOS) guideline, published in 2008, takes a more definitive stance and recommends that lateral heel wedges NOT be prescribed for people with medial knee OA [40]. The discrepancy in recommendations regarding lateral wedges is largely related to the conflicting findings between biomechanical studies and clinical trials. Early research into lateral wedges was primarily confined to biomechanical evaluations. A recent systematic review (of literature published until January 2011) evaluated the effect of insoles on the external KAM in people with medial knee OA [37••]. This review demonstrated that lateral wedging was associated with a reduction in the peak KAM in ten out of the twelve studies included in the review (mean reductions ranging from 2 to 12 %). Most new biomechanical evaluations of lateral wedges published since 2011 agree with these findings [41–43]. Unfortunately, the assumption that the load-reducing effects of lateral wedges will translate into clinically meaningful reductions in pain in people with knee OA has not been borne out in the clinical trials conducted to date [44–47]. Of note, the latest RCT, involving 200 people with medial knee OA and published in BMJ in 2011 [48••], demonstrated that lateral wedges worn over 12 months do not significantly reduce pain or slow structural disease progression (as measured via cartilage volume on MRI). On the basis of the latest research findings, it would appear that lateral wedges offer no clinical benefit to patients with knee OA.
Given the disappointing findings of clinical trials evaluating lateral wedges, attention has recently turned to alternative types of insoles for managing knee OA. Shock-absorbing insoles have been evaluated for their effects on biomechanics, pain and function in one small study in 16 people with knee OA [49•]. This study found no immediate effect of shock-absorbing insoles on any parameter of KAM; however, late stance peak KAM did reduce from baseline to follow-up after 1 month of wearing the insoles. There is currently no evidence that a reduction in late stance peak KAM is clinically relevant. Whilst this study showed that shock-absorbing insoles significantly reduced pain and improved function after 1 month of wear, it is not clear whether these changes in symptoms are due to a real treatment effect or a placebo response. Clinical trials are needed to evaluate the efficacy of shock-absorbing insoles for knee OA and to provide evidence for informing future clinical guidelines.
Research has shown that medial knee OA is associated with a flattened (pronated) foot posture [50]. Furthermore, recent data has linked the pronated foot type to a greater frequency of knee pain and medial tibiofemoral cartilage damage in older people [51]. Whilst medial arch supports could constitute a logical treatment choice for these patients, the causal relationship between flattened foot posture and knee OA is yet to be established. It is possible that medial arch supports may cause a medial shift in the centre of pressure, thereby increasing the distance between the ground reaction force and the knee centre and increasing the KAM during gait [52, 53], and could be potentially harmful rather than beneficial. There is currently limited research about the effects of medial arch supports in people with knee OA. One study [54] evaluated a combination orthotic comprising both a medial arch support and lateral wedging. However, because this study involved a combination orthotic and utilised a control condition that also comprised medial arch supports, no conclusions about the independent biomechanical effects of medial arch supports can be drawn. In contrast, a recent study [55••] evaluated the independent immediate effects of medial arch supports on the KAM in 21 people with medial knee OA, as well as effects on pain during gait analysis. Findings showed that the medial arches had no significant effect on the KAM, nor resulted in any immediate changes in pain. Further research in this area is needed, particularly with a focus on longer-term follow-up periods, in order to assist clinicians in deciding whether medial arch supports may be of benefit for patients with knee OA.
Clinical guidelines from OARSI recommend that every patient with knee OA should receive advice concerning appropriate footwear [5]. This recommendation was based on expert opinion given the lack of RCT evidence at the time the guidelines were developed. Regular off-the-shelf footwear increases parameters of medial knee load compared to barefoot walking in people with knee OA by 7–14 % depending on shoe type [37]. The types of shoes that are more likely to increase medial knee load include those with high heels, and those that promote foot stability rather than mobility [56–59, 60•]. It appears that lightweight, flat and flexible footwear options may be optimal for people with knee OA. This is supported by data from recent biomechanical studies [61, 62] that evaluated an inexpensive, flat canvas shoe with a flexible rubber sole (Moleca, Calcados Beira Rio). In elderly women with knee OA, these shoes resulted in lower knee loads during stair descent and walking compared to heeled shoes. In fact, the knee loads experienced with the flexible shoe approximated those of barefoot walking. Thus, biomechanical evidence suggests clinicians should assess the footwear of patients with knee OA, particularly those with medial compartment disease and/or varus malalignment who are at risk of higher knee loads (and more rapid structural disease progression [26, 27]), and advise them regarding optimal footwear choices to minimise loading across the knee.
Over the past few years, there has been much interest in the development and evaluation of novel innovative footwear, specially designed to reduce knee loads in people with knee OA. Shoes with “variable stiffness” soles, where the lateral sole is stiffer compared to the medial side, have been shown to reduce the KAM compared to shoes with a constant stiffness sole [63, 64]. In an RCT comparing variable stiffness shoes to constant stiffness control shoes, the variable stiffness shoes resulted in significant within-group pain reductions at 6 months (average 37 % pain reduction compared to 19 % in control group); however, the change in symptoms was not significantly different between groups at either 6 months or 1 year [65, 66••]. The nonsignificant findings of this study may be related to the small sample size. A “mobility” shoe specially engineered to mimic barefoot walking and incorporating a flexible grooved sole, can reduce the peak KAM by 8 % compared to self-selected walking shoes [67], however the efficacy of this novel shoe style in treating symptoms associated with knee OA has not yet been evaluated. Commercially available unstable shoes (Masai Barefoot Technology®), which have a multilayered sole that mimics walking on soft uneven ground, have been suggested as a treatment option for people with knee OA given their potential to improve gait stability and reduce joint load [68]. Recent kinematic and kinetic evaluations of these shoes have shown they reduce peak KAM by up to 13 % in overweight males (who are at risk of developing knee OA) [69]. However an RCT, which compared unstable shoes to control walking shoes over 12 weeks in a sample with symptomatic knee OA, showed no significant differences between groups regarding change in pain, balance, knee range of motion or ankle strength [68]. Thus at present it is not clear what role innovative shoe designs may play in managing symptoms associated with knee OA.
Conclusion
Non-pharmacological rehabilitation strategies play an important role in the management of patients with symptomatic knee OA and those at risk of developing the disease. In particular, exercise is considered a core component of rehabilitation, given its beneficial effects on pain and function. Currently, exercise programs do not appear to have a disease-modifying effect in people with established knee OA. Although there is biomechanical evidence that gait retraining, footwear and insoles can significantly reduce parameters of medial knee loading in people with knee OA, the clinical benefits of most of these interventions remain largely unproven.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
Fransen M, McConnell S. Land-based exercise for osteoarthritis of the knee: a meta-analysis of randomized controlled trials. J Rheumatol. 2009;36:1109–17.
Zhang W, Nuki G, Moskowitz RW, Abramson S, Altman RD, Arden NK, et al. OARSI recommendations for the management of hip and knee osteoarthritis: part III: changes in evidence following systematic cumulative update of research published through January 2009. Osteoarthr Cartil. 2010;18:476–99.
• Wallis JA, Taylor NF. Pre-operative interventions (non-surgical and non-pharmacological) for patients with hip or knee osteoarthritis awaiting joint replacement surgery-a systematic review and meta-analysis. Osteoarthritis Cartilage 2011, 19:1381–95.
Supports the inclusion of pre-operative exercise interventions for people undergoing joint replacement.
Jordan KM, Arden NK, Doherty M, Bannwarth B, Bijlsma JW, Dieppe P, et al. EULAR Recommendations 2003: an evidence based approach to the management of knee osteoarthritis: report of a Task Force of the Standing Committee for International Clinical Studies Including Therapeutic Trials (ESCISIT). Ann Rheum Dis. 2003;62:1145–55.
Zhang W, Moskowitz RW, Nuki G, Abramson S, Altman RD, Arden N, et al. OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines. Osteoar Cartil. 2008;16:137–62.
•• Hochberg MC, Altman RD, Toupin April K, Benkhalti M, Guyatt G, McGowan J et al. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res 2012;64:465–74.
Most recent clinical guidelines for the management of people with osteoarthritis.
Batterham SI, Heywood S, Keating JL. Systematic review and meta-analysis comparing land and aquatic exercise for people with hip or knee arthritis on function, mobility and other health outcomes. BMC Musculoskelet Disord. 2011;12:123.
• Fitzgerald GK, Piva SR, Gil AB, Wisniewski SR, Oddis CV, Irrgang JJ. Agility and perturbation training techniques in exercise therapy for reducing pain and improving function in people with knee osteoarthritis: a randomized clinical trial. Phys Ther 2011;91:452–69.
Largest randomised controlled trial investigating this form of exercise therapy.
Peter WF, Jansen MJ, Hurkmans EJ, Bloo H, Dekker J, Dilling RG, et al. Physiotherapy in hip and knee osteoarthritis: development of a practice guideline concerning initial assessment, treatment and evaluation. Acta Reumatol Port. 2011;36:268–81.
Dreinhofer K, Stucki G, Ewert T, Huber E, Ebenbichler G, Gutenbrunner C et al. ICF core sets for osteoarthritis. J Rehabil Med. 2004;75–80. doi:10.1080/16501960410015498.
Hurley MV, Walsh NE, Mitchell H, Nicholas J, Patel A. Long-term outcomes and costs of an integrated rehabilitation program for chronic knee pain: a pragmatic, cluster randomized, controlled trial. Arthritis Care Res. 2012;64:238–47.
Pinto D, Robertson MC, Hansen P, Abbott JH. Cost-effectiveness of nonpharmacologic, nonsurgical interventions for hip and/or knee osteoarthritis: systematic review. Value Health. 2012;15:1–12.
Brosseau L, Wells GA, Tugwell P, Egan M, Dubouloz CJ, Casimiro L, et al. Ottawa Panel evidence-based clinical practice guidelines for the management of osteoarthritis in adults who are obese or overweight. Phys Ther. 2011;91:843–61.
Henriksen M, Christensen R, Danneskiold-Samsøe B, Bliddal H. Changes in lower extremity muscle mass and muscle strength after weight loss in obese patients with knee osteoarthritis: a prospective cohort study. Arthritis Rheum. 2012;64:438–42.
Cottrell E, Roddy E, Foster NE. The attitudes, beliefs and behaviours of GPs regarding exercise for chronic knee pain: a systematic review. BMC Fam Pract. 2010;11:4.
Li LC, Sayre EC, Kopec JA, Esdaile JM, Bar S, Cibere J. Quality of nonpharmacological care in the community for people with knee and hip osteoarthritis. J Rheumatol. 2011;38:2230–7.
Urquhart DM, Tobing JF, Hanna FS, Berry P, Wluka AE, Ding C, et al. What is the effect of physical activity on the knee joint? A systematic review. Med Sci Sports Exerc. 2011;43:432–42.
Messier SP, Loeser RF, Miller GD, Morgan TM, Rejeski WJ, Sevick MA, et al. Exercise and dietary weight loss in overweight and obese older adults with knee osteoarthritis: the arthritis, diet, and activity promotion trial. Arthritis Rheum. 2004;50:1501–10.
Mikesky AE, Mazzuca SA, Brandt KD, Perkins SM, Damush T, Lane KA. Effects of strength training on the incidence and progression of knee osteoarthritis. Arthritis Rheum. 2006;55:690–9.
Ettinger WH Jr, Burns R, Messier SP, Applegate W, Rejeski WJ, Morgan T, et al. A randomized trial comparing aerobic exercise and resistance exercise with a health education program in older adults with knee osteoarthritis. The fitness arthritis and seniors trial (FAST). JAMA. 1997;277:25–31.
Foroughi N, Smith RM, Lange AK, Baker MK, Fiatarone Singh MA, Vanwanseele B. Lower limb muscle strengthening does not change frontal plane moments in women with knee osteoarthritis: a randomized controlled trial. Clin Biomech (Bristol, Avon). 2011;26:167–74.
Lim BW, Hinman RS, Wrigley TV, Sharma L, Bennell KL. Does knee malalignment mediate the effects of quadriceps strengthening on knee adduction moment, pain, and function in medial knee osteoarthritis? A randomized controlled trial. Arthritis Rheum. 2008;59:943–51.
Bennell KL, Hunt MA, Wrigley TV, Hunter DJ, McManus FJ, Hodges PW, et al. Hip strengthening reduces symptoms but not knee load in people with medial knee osteoarthritis and varus malalignment: a randomised controlled trial. Osteoarthr Cartil. 2010;18:621–8.
Andriacchi TP, Mundermann A. The role of ambulatory mechanics in the initiation and progression of knee osteoarthritis. Curr Opin Rheumatol. 2006;18:514–8.
Schipplein OD, Andriacchi TP. Interaction between active and passive knee stabilizers during level walking. J Orthop Res. 1991;9:113–9.
Bennell KL, Bowles KA, Wang Y, Cicuttini F, Davies-Tuck M, Hinman RS. Higher dynamic medial knee load predicts greater cartilage loss over 12 months in medial knee osteoarthritis. Ann Rheum Dis. 2011;70:1770–4.
Miyazaki T, Wada M, Kawahara H, Sato M, Baba H, Shimada S. Dynamic load at baseline can predict radiographic disease progression in medial compartment knee osteoarthritis. Ann Rheum Dis. 2002;61:617–22.
• Simic M, Hinman RS, Wrigley TV, Bennell KL, Hunt MA. Gait modification strategies for altering medial knee joint load: a systematic review. Arthritis Care Res 2011;63:405–26.
Systematic review of gait modification strategies and their effects on the knee adduction moment.
Hunt MA, Schache AG, Hinman RS, Crossley KM. Varus thrust in medial knee osteoarthritis: quantification and effects of different gait-related interventions using a single case study. Arthritis Care Res. 2011;63:293–7.
Hunt MA, Simic M, Hinman RS, Bennell KL, Wrigley TV. Feasibility of a gait retraining strategy for reducing knee joint loading: increased trunk lean guided by real-time biofeedback. J Biomech. 2011;44:943–7.
Mundermann A, Mundermann L, Andriacchi TP. Amplitude and phasing of trunk motion is critical for the efficacy of gait training aimed at reducing ambulatory loads at the knee. J Biomech Eng. 2012;134:011010.
• Simic M, Hunt MA, Bennell KL, Hinman RS, Wrigley TV. Trunk lean gait modification and knee joint load in people with medial knee osteoarthritis: The effect of varying trunk lean angles. Arthritis Care Res. 2012;64:1545–53.
First study to evaluate the ipsilateral trunk lean gait modification in people with knee osteoarthritis.
Shull PB, Lurie KL, Cutkosky MR, Besier TF. Training multi-parameter gaits to reduce the knee adduction moment with data-driven models and haptic feedback. J Biomech. 2011;44:1605–9.
Simic M, Bennell KL, Hunt MA, Wrigley TV, Hinman RS. Contralateral cane use and knee joint load in people with medial knee osteoarthritis: the effect of varying body weight support. Osteoarthr Cartil. 2011;19:1330–7.
•• Jones A, Silva PG, Silva AC, Colucci M, Tuffanin A, Jardim JR et al. Impact of cane use on pain, function, general health and energy expenditure during gait in patients with knee osteoarthritis: a randomised controlled trial. Ann Rheum Dis. 2012;71:172–9.
First randomised controlled trial investigating the effects of cane use on symptoms in people with knee osteoarthritis.
Riskowski J, Dufour AB, Hannan MT. Arthritis, foot pain and shoe wear: current musculoskeletal research on feet. Curr Opin Rheumatol. 2011;23:148–55.
•• Radzimski AO, Mundermann A, Sole G. Effect of footwear on the external knee adduction moment—A systematic review. Knee 2011;19(3):163–75.
Systematic review of studies evaluating the effect of footwear and orthotics on the knee adduction moment.
Brouwer R, Jakma T, Verhagen A, Verhaar J, Bierma-Zeinstra S. Braces and orthoses for treating osteoarthritis of the knee. Cochrane Lib. 2005. doi:10.1002/14651858.CD004020.pub2.
Rodrigues P, Ferreira A, Pereira R, Bonfa E, Borba E, Fuller R. Effectiveness of medial-wedge insole treatment for valgus knee osteoarthritis. Arthritis Care Res. 2008;59:603–8.
American Academy of Orthopedic Surgeons. Guideline on the treatment of osteoarthritis of the knee. 2008.
Hinman RS, Bowles KA, Metcalf BB, Wrigley TV, Bennell KL. Lateral wedge insoles for medial knee osteoarthritis: effects on lower limb frontal plane biomechanics. Clin Biomech (Bristol, Avon). 2012;27:27–33.
Leitch KM, Birmingham TB, Jones IC, Giffin JR, Jenkyn TR. In-shoe plantar pressure measurements for patients with knee osteoarthritis: reliability and effects of lateral heel wedges. Gait Posture. 2011;34:391–6.
Russell EM, Hamill J. Lateral wedges decrease biomechanical risk factors for knee osteoarthritis in obese women. J Biomech. 2011;44:2286–91.
Baker K, Goggins J, Xie H, Szumowski K, LaValley M, Hunter DJ, et al. A randomized crossover trial of a wedged insole for treatment of knee osteoarthritis. Arthritis Rheum. 2007;56:1198–203.
Butler RJ, Marchesi S, Royer T, Davis IS. The effect of a subject-specific amount of lateral wedge on knee mechanics in patients with medial knee osteoarthritis. J Orthop Res. 2007;25:1121–7.
Maillefert JF, Hudry C, Baron G, Kieffert P, Bourgeois P, Lechevalier D, et al. Laterally elevated wedged insoles in the treatment of medial knee osteoarthritis: a prospective randomized controlled study. Osteoarthr Cartil. 2001;9:738–45.
Pham T, Maillefert JF, Hudry C, Kieffert P, Bourgeois P, Lechevalier D, et al. Laterally elevated wedged insoles in the treatment of medial knee osteoarthritis. A two-year prospective randomized controlled study. Osteoarthr Cartil. 2004;12:46–55.
•• Bennell K, Bowles K, Payne C, Cicuttini F, Williamson E, Forbes A et al. Lateral wedge shoe insoles for medial knee osteoarthritis: 12 month randomised controlled trial. BMJ. 2011;342:2912.
The first randomised controlled trial to evaluate the effects of lateral wedge insoles on symptoms and joint structure in people with knee osteoarthritis.
• Turpin KM, De Vincenzo A, Apps AM, Cooney T, MacKenzie MD, Chang R et al. Biomechanical and clinical outcomes with shock-absorbing insoles in patients with knee osteoarthritis: immediate effects and changes after 1 month of wear. Arch Phys Med Rehabil. 2012;93:503–8.
First biomechanical evaluation of the effects of shock-absorbing insoles in people with knee osteoarthritis.
Levinger P, Menz HB, Fotoohabadi MR, Feller JA, Bartlett JR, Bergman NR. Foot posture in people with medial compartment knee osteoarthritis. J Foot Ankle Res. 2010;3:29.
Gross KD, Felson DT, Niu J, Hunter DJ, Guermazi A, Roemer FW, et al. Association of flat feet with knee pain and cartilage damage in older adults. Arthritis Care Res. 2011;63:937–44.
Haim A, Rozen N, Dekel S, Halperin N, Wolf A. Control of knee coronal plane moment via modulation of center of pressure: a prospective gait analysis study. J Biomech. 2008;41:3010–6.
Franz JR, Dicharry J, Riley PO, Jackson K, Wilder RP, Kerrigan DC. The influence of arch supports on knee torques relevant to knee osteoarthritis. Med Sci Sports Exerc. 2008;40:913–7.
Abdallah AA, Radwan AY. Biomechanical changes accompanying unilateral and bilateral use of laterally wedged insoles with medial arch supports in patients with medial knee osteoarthritis. Clin Biomech. 2011;26:783–9.
•• Hinman RS, Bardin L, Simic M, Bennell KL. Medial arch supports do not significantly alter the knee adduction moment in people with knee osteoarthritis. Osteoarthritis Cartilage 2012, Oct 24 (Epub ahead of print).
First study evaluating the independent immediate effects of medial arch supports on parameters of the knee adduction moment and pain in people with knee osteoarthritis.
Kerrigan D, Johansson J, Bryant M, Boxer J. Della Croce U, Riley P. Moderate-heeled shoes and knee joint torques relevant to the development and progression of knee osteoarthritis. Arch Phys Med Rehabil. 2005;86:871–5.
Kerrigan D, Karvosky M, Lelas J, Riley P. Men’s shoes and knee joint torques relevant to the development and progression of knee osteoarthritis. J Rheumatol. 2003;30:529–33.
Kerrigan D, Lelas J, Karvosky M. Women’s shoes and knee osteoarthritis. Lancet. 2001;357:1097–8.
Kerrigan DC, Todd MK, Riley PO. Knee osteoarthritis and high-heeled shoes. Lancet. 1998;351:1399–401.
• Shakoor N, Sengupta M, Foucher KC, Wimmer MA, Fogg LF, Block JA. Effects of common footwear on joint loading in osteoarthritis of the knee. Arthritis Care Res 2010;62:917–23.
This study highlights that different types of shoes have different effects on the knee adduction moment in people with knee osteoarthritis.
Sacco IC, Trombini-Souza F, Butugan MK, Passaro AC, Arnone AC, Fuller R. Joint loading decreased by inexpensive and minimalist footwear in elderly women with knee osteoarthritis during stair descent. Arthritis Care Res. 2012;64:368–74.
Trombini-Souza F, Kimura A, Ribeiro AP, Butugan M, Akashi P, Passaro AC, et al. Inexpensive footwear decreases joint loading in elderly women with knee osteoarthritis. Gait Posture. 2011;34:126–30.
Erhart JC, Dyrby CO, D’Lima DD, Colwell CW, Andriacchi TP. Changes in in vivo knee loading with a variable-stiffness intervention shoe correlate with changes in the knee adduction moment. J Orthop Res. 2010;28:1548–53.
Erhart JC, Mundermann A, Elspas B, Giori NJ, Andriacchi TP. A variable-stiffness shoe lowers the knee adduction moment in subjects with symptoms of medial compartment knee osteoarthritis. J Biomech. 2008;41:2720–5.
Erhart JC, Mundermann A, Elspas B, Giori NJ, Andriacchi TP. Changes in knee adduction moment, pain, and functionality with a variable-stiffness walking shoe after 6 months. J Orthop Res. 2010;28:873–9.
•• Erhart-Hledik JC, Elspas B, Giori NJ, Andriacchi TP. Effect of variable-stiffness walking shoes on knee adduction moment, pain, and function in subjects with medial compartment knee osteoarthritis after 1 year. J Orthop Res 2012, 30:514–21.
Randomised controlled trial evaluating the effects of a novel shoe design on symptoms and biomechanics in people with knee osteoarthritis.
Shakoor N, Lidtke RH, Sengupta M, Fogg LF, Block JA. Effects of specialized footwear on joint loads in osteoarthritis of the knee. Arthritis Rheum. 2008;59:1214–20.
Nigg B, Emery C, Hiemstra L. Unstable shoe construction and reduction of pain in osteoarthritis patients. Med Sci Sports Exerc. 2006;38:1701–8.
Buchecker M, Wagner H, Pfusterschmied J, Stoggl TL, Muller E. Lower extremity joint loading during level walking with Masai barefoot technology shoes in overweight males. Scand J Med Sci Sports. 2010;22(3):372–80.
Disclosure
RS Hinman: board membership for Physical Therapy EBM, an institutional grant from ARC/NHMRC, paid lecturer for APA, and royalties for the University of Melbourne OA DVD and Asics Gel University of Melbourne OA shoe; MA Hunt: institutional grant from Canadian Institutes of Health Research and royalties for the University of Melbourne OA DVD; M Simic: none; and KL Bennell: lecture payments from IASP and royalties for the Asics Gel University of Melbourne OA shoe.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hinman, R.S., Hunt, M.A., Simic, M. et al. Exercise, Gait Retraining, Footwear and Insoles for Knee Osteoarthritis. Curr Phys Med Rehabil Rep 1, 21–28 (2013). https://doi.org/10.1007/s40141-012-0004-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40141-012-0004-8