Abstract
Purpose
Information technology (IT)-based interventions, especially mobile health (mHealth), possess a great potential for promoting self-management in patients with chronic diseases, including diabetes type II. The present study was aimed to design and develop a smartphone-based application (app) for nutrition management in patients with type II diabetes and evaluation of its usability.
Methods
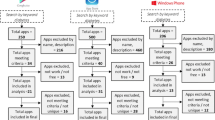
In this study, a three-phase research approach was followed; (1) To determine the information content and functionalities of the app, a five-point Likert scale checklist including six parts was developed based on reviews of clinical practice guidelines and specialized databases. The checklist was then given to ten experts in endocrinology and metabolism, internal medicine, and nutrition, and those items with a mean score higher than 3.75 were approved. (2) In Android Studio, the app was designed and developed using Java language. (3) The Questionnaire for User Interaction Satisfaction (QUIS) was used to assess the app’s usability by 21 patients with type II diabetes, ten IT experts, and seven endocrinologists, internal medicine practitioners, and nutritionists over one month. Mean scores were divided into three levels: weak (0–3), average (3–6), and good (6–9).
Results
According to experts’ view, 17 out of 22 educational content and 17 out of 27 functionalities were approved. The app’s most important educational content was the timing of meals for insulin patients and the definition of diabetes and its complications. The designed app had the following functionalities: providing educational information, recording information, performing calculations, representing data graphically, setting reminders, and communicating with physicians. The most important features of the app were the insulin dose calculation, reminders for doctors’ appointments, setting times for tests and blood glucose measurements, and also tracking weight, blood glucose levels, and blood pressure. In terms of usability evaluation, the app was rated “good” level by diabetic patients (7.83 ± 0.74), IT experts (8.1 ± 0.66), and physicians (8.03 ± 0.95).
Conclusion
Given the desirable evaluation of the app by patients, physicians, and IT experts, it can be concluded that the developed app has the required functionalities for nutrition management of patients with type II diabetes. Smartphone-based apps appear to be able to improve self-management, the quality of care and health in patients with diabetes, and reduce many of their unnecessary visits to healthcare centers, and costs.

Similar content being viewed by others
Data Availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Shrivastava SR, Shrivastava PS, Ramasamy J. Role of self-care in management of diabetes mellitus. J Diabetes Metabolic Disorders. 2013;12(1):14.
World Health Organization, Global report on diabetes. 2016. p. 88.
Whiting DR, et al. IDF diabetes atlas: global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract. 2011;94(3):311–21.
Xu J, et al., Deaths: Final data for 2016. 2018.
Papatheodorou K, et al., Complications of Diabetes 2017. Journal of diabetes research, 2018. 2018.
Nadkarni A. Implementation Plans and Self-Monitoring of Blood Glucose in Diabetics, in Social and Administrative Sciences. University of Michigan; 2009.
Stiffler D, Cullen D, Luna G. Diabetes barriers and self-care management: the patient perspective. Clin Nurs Res. 2014;23(6):601–26.
Yasa I, et al. Barrier of Self Care Management on Urban Type 2 Diabetic Patients in Bali. Indian J Public Health Res Dev. 2018;9(5):363–7.
Dunning T. Care of people with diabetes: A manual of nursing practice. John Wiley & Sons; 2013.
Parizad N, Khalkhali H. Promoting self-care in patients with type 2 diabetes: tele-education. Hakim Res J. 2013;16(3):220–7.
Peck A. Changing the face of standard nursing practice through telehealth and telenursing. Nurs Adm Q. 2005;29(4):339–43.
Zolfaghari M, Mousavifar SA, Haghani H. Mobile phone text messaging and Telephone follow-up in type 2 diabetic patients for 3 months: a comparative study. J Diabetes Metabolic Disorders. 2012;11(1):7.
Muralidharan S, et al. Mobile health technology in the prevention and management of type 2 diabetes. Indian J Endocrinol Metabol. 2017;21(2):334.
Williams JLS, et al. Effective interventions to improve medication adherence in Type 2 diabetes: a systematic review. Diabetes Manage (London England). 2014;4(1):29.
Zamanzadeh V, et al. Distance education and diabetes empowerment: A single-blind randomized control trial. Diabetes & Metabolic Syndrome: Clinical Research & Reviews. 2017;11:S247–51.
Holtz B, Lauckner C. Diabetes management via mobile phones: a systematic review. Telemedicine and e-Health. 2012;18(3):175–84.
Schnall R, et al., Comparison of a user-centered design, self-management app to existing mHealth apps for persons living with HIV. JMIR mHealth and uHealth, 2015. 3(3): p. e91.
Martinez PR, A qualitative study on patient perceptions towards mHealth technology among high risk, chronic disease patients. 2015.
Park S, et al. An integrated mHealth model for type 2 diabetes patients using mobile tablet devices. J Mob Technol Med. 2016;5(2):24–32.
Hoque R, Sorwar G. Understanding factors influencing the adoption of mHealth by the elderly: An extension of the UTAUT model. Int J Med Informatics. 2017;101:75–84.
Goyal S, et al. The systematic design of a behavioural mobile health application for the self-management of type 2 diabetes. Can J diabetes. 2016;40(1):95–104.
Ahn Y, Bae J, Kim H-S. The development of a mobile u-Health program and evaluation for self-diet management for diabetic patients. Nutr Res Pract. 2016;10(3):342–51.
Nie L, et al. Characteristics of Chinese m-Health applications for diabetes self-management. Telemedicine and e-Health. 2016;22(7):614–9.
Drumm S, Bradley C, Moriarty F. ‘More of an art than a science’? The development, design and mechanics of the Delphi Technique. Res Social Administrative Pharm. 2022;18(1):2230–6.
Lawshe CH. A quantitative approach to content validity. Pers Psychol. 1975;28(4):563–75.
Polit DF, Beck CT, Owen SV. Is the CVI an acceptable indicator of content validity? Appraisal and recommendations. Res Nurs Health. 2007;30(4):459–67.
Veneziano L. A method for quantifying content validity of health-related questionnaires. Am J Health Behav. 1997;21(1):67–70.
Waltz CF, Bausell BR. Nursing research: design statistics and computer analysis. Davis Fa; 1981.
Chin JP, Diehl VA, Norman KL. Development of an instrument measuring user satisfaction of the human-computer interface. in Proceedings of the SIGCHI conference on Human factors in computing systems. 1988.
Alexandru C-A. Usability testing and improvement of telemedicine websites. M. Sc. diss. University of Edinburgh. Edinburgh; 2010.
Alliance. I.D.F.a.t.D.I., Diabetes and Ramadan: practical guidelines. International Diabetes Federation: Brussels, Belgium; 2016.
Sciences T. E.a.M.R.C.o.T.U.o.M., Diabetes clinical guideline abstract. Iran: Tehran; 2015.
Biernatzki L, et al. Information needs in people with diabetes mellitus: a systematic review. Syst reviews. 2018;7(1):27.
Kalantzi S, et al. Information seeking behavior of patients with diabetes mellitus: a cross-sectional study in an outpatient clinic of a university-affiliated hospital in Athens. Greece BMC research notes. 2015;8(1):48.
Salehi F, et al. The role of information resources used by diabetic patients on the management of their disease. Med J mashhad Univ Med Sci. 2016;59(1):17–25.
Shahrakivahed A, et al. A study on the assessment of educational needs of diabetic patients. J Diabetes Nurs. 2013;1(1):31–7.
Weymann N, Härter M, Dirmaier J. Information and decision support needs in patients with type 2 diabetes. Health Inf J. 2016;22(1):46–59.
Buijink AWG, Visser BJ, Marshall L. Medical apps for smartphones: lack of evidence undermines quality and safety. BMJ Evidence-Based Medicine. 2013;18(3):90–2.
Boyle L, et al., Use of and beliefs about mobile phone apps for diabetes self-management: surveys of people in a hospital diabetes clinic and diabetes health professionals in New Zealand. JMIR mHealth and uHealth, 2017. 5(6): p. e85.
Safdari R, et al. Design and evaluation of a mobile-based application for patients with type 2 diabetes: Case study of Shariati hospital in Tehran, Iran. Hosp Practices Res. 2018;3(4):130–6.
Izahar S, et al. Content analysis of mobile health applications on diabetes mellitus. Front Endocrinol. 2017;8:318.
Antoun J. Electronic mail communication between physicians and patients: a review of challenges and opportunities. Fam Pract. 2016;33(2):121–6.
Patt MR, et al. Doctors who are using e-mail with their patients: a qualitative exploration. J Med Internet Res. 2003;5(2):e9.
Ghazisaeedi M, et al. Designing a mobile-based self-care application for patients with heart failure. J Health Biomedical Inf. 2016;3(3):195–204.
Ghazisaeedi M, et al., Design and evaluation of an applied educational smartphone-based program for caregivers of children with cerebral palsy. 2015.
Lee T-I, et al. Development and evaluation of a patient-oriented education system for diabetes management. Int J Med Informatics. 2007;76(9):655–63.
Shahmoradi L. L.M., Design and implementation of mobile applications to predict survival in kidney transplant patients. Tehran University of Medical Sceinces: Tehran, Iran; 2015.
Garnweidner-Holme LM, et al. Designing and developing a mobile smartphone application for women with gestational diabetes mellitus followed-up at diabetes outpatient clinics in Norway. In: Healthcare. Multidisciplinary Digital Publishing Institute; 2015.
Langarizadeh m, Behzadian H, Samimi M. Development of personal health record application for gestational diabetes, based on smart phone. The J Urmia Nurs Midwifery Fac. 2016;14(8):714–27.
Hamborg K-C, Vehse B, Bludau H-B. Questionnaire based usability evaluation of hospital information systems. Electron J Inform Syst evaluation. 2004;7(1):21–30.
Joshi A, et al. An interactive, bilingual touch screen program to promote breastfeeding among Hispanic rural women: usability study. JMIR Res Protocols. 2013;2(2):e47.
Acknowledgements
The present article is part of an MSc thesis in health information technology. The authors wish to thank the Research and Technology Deputy of Kashan University of Medical Sciences for their support.
Author information
Authors and Affiliations
Contributions
Conception and design of study (EN, FR), Development of materials (EN, RH), Data collection (ST, RH), Data analysis and interpretation (RH, RSh), Drafting the article (EN, RSh, RH), Revising article critically for important intellectual content (EN, RSh), Final approval of the version to be published (EN, FR, ST, RH, RSh).
Corresponding author
Ethics declarations
Statements and declarations
Funding.
This study was supported by a grant from Kashan University of Medical Sciences Research Council (Number: 96104) and did not receive any grants from non-profit organizations and funding agencies in the public and commercial sectors.
Competing interests
The authors declare that they have no competing interests.
Ethics approval and consent to participate
The present study was approved by the Ethics Committee of Kashan University of Medical Sciences (Code: IR.KAUMS.NUHEPM.REC.1396.21). The researcher obtained the necessary permission to conduct the study from the university officials. The study objectives were explained to the participants and their informed consent was obtained. The participants’ independence was maintained by assuring them about their voluntary participation, non-participation, and withdrawal. Data were confidentially kept by the researcher and were only used for the study purposes. Regarding the use of scientific references and translation, copyrights were entirely observed.
List of abbreviations
Type II diabetes mellitus (T2DM), World Health Organization (WHO), electronic Health (eHealth), mobile Health (mHealth), Applications (apps), Information Technology (IT), electronic Health (eHealth), Content Validity Index (CVI), Content Validity Ratio (CVR), Statistical Package for Social Sciences (SPSS), Graphical User Interface (GUI), Questionnaire for User Interaction Satisfaction (QUIS).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nabovati, E., Rangraz Jeddi, F., Tabatabaeizadeh, S.M. et al. Design, development, and usability evaluation of a smartphone-based application for nutrition management in patients with type II diabetes. J Diabetes Metab Disord 22, 315–323 (2023). https://doi.org/10.1007/s40200-022-01140-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40200-022-01140-x