Abstract
Multifaceted international and national collaborative responses and progress have sustained the world’s largest densely populated refugee camps in the Cox’s Bazar district, Bangladesh. Yet, the Rohingyas remain in an extremely precarious situation during the COVID-19 pandemic. The refugees are living in highly challenging circumstances of water, sanitation, and hygiene (WASH), natural disasters of the monsoon season as well as existing health and educational challenges of HIV, malnutrition and other diseases. Particulate matter PM2.5 in the sampling camps varied from 44 μg/m3 to 546 μg/m3, whereas PM10 in the sampling camps varied from 125 μg/m3 to 1122 μg/m3. Due to lock-down of Cox’s Bazar, aid workers in and out of the camps were restrained with the only continuation of emergency food and medical service supplies. Largely dependent on aid during the ongoing pandemic, an investigation of the socio-environmental challenges of the refugee camps will identify the anticipatory impacts and needs.
Similar content being viewed by others
Introduction
Bangladesh hosts nearly 1 million Rohingya refugees from the neighbouring country Myanmar, who fled the persecution of the Myanmar junta from the Northern Rakhine State to the district of Cox’s Bazar, which is the second poorest district of Bangladesh. Approximately 744,000 Rohingya refugees arrived since August 2017 creating a humanitarian emergency for shelter, food and other life-saving needs. Besides, this number also includes many unregistered Rohingya refugees who had settled before 2017 and registered refugees of 34,172 who arrived in the 1990s. Most of the refugees reside in Ukhiya and Teknaf Upazilas in 34 extremely congested camps, including the largest single-site, the Kutupalong-Balukhali Expansion Site, residing approximately 626,500 Rohingyas [1]. Children make up 52% of the total refugee population and women and girls makeup 51% [2]. The camp population density is approximately 8 m2/person compared to the international standard of 45 m2/person [1]. Whilst the pace of arrivals has decreased, refugees continue to arrive in Bangladesh even during the COVID-19 pandemic as 396 Rohingyas were rescued from the Teknaf coast by the Bangladeshi coast guards and kept in quarantine [3]. As of today the number of COVID-19 patients in the Cox’s Bazar district is 5 [4]. Now, as the number of COVID-19 cases inclines up in Bangladesh, the Rohingya refugees fear that they could be hard hit.
Rohingya refugees work in jobs generated inside the camps by the UNHCR and its related organizations with a meagre income to support their family’s health and wellbeing [5]. According to UNHCR [2], one in three refugee families has at least one easily identifiable protection vulnerability. Denied of the citizenship of Myanmar, Rohingyas were also deprived of education, healthcare and contraception knowledge, and other living services. In a study conducted in 2019, most refugees (84%) were not concerned about water, sanitation, and hygiene (WASH) [6]. Moreover, during the crises period, Rohingya females and children were sexually exploited, increasing the risk of exposure to HIV and other sexually transmitted diseases (STDs) [5]. Furthermore, diphtheria which is a respiratory disease, eliminated by the government of Bangladesh (GOB), were outbreak in the camps and killed more than 30 and affected more than 500, were primarily children [1]. More than a year of multifaceted collaborative response, the situation gradually stabilized in the camps with the basic assistance being provided, living conditions improved somewhat and disaster risk mitigation measures have been largely successful [1]. On April 9, 2020, GOB lockdown Cox’s Bazar due to the detection of a COVID-19 patient in the district and thus ordering restriction for aid workers in and out of the camps and only continuation of emergency food and medical service supplies. In these circumstances, the aim of this article is, therefore, to explore how the largest refugee camp can fight back the COVID-19 pandemic and what are the socio-environmental challenges for them.
Methods
WASH scenario of the Rohingya refugee camps were collected from the UNHCR documents. Air Particulate matter (PM2.5 & PM10) was collected by field survey in 2019 from Balukhali Rohingya refugee camp No- 7, 9 and 13 in Ukhia, Coxsbazar District. Perfect Prime Air quality detector AQ9600) has been used for determining the measurement of PM2.5 and PM10 during the cooking time at morning 7–11 am and after 4 h.
Results and discussions
In resource-deprived refugee camps during the outbreak of pandemic, social-distancing, isolation and treatment of patients, social stigmatizations, maintaining frequent washing hands and basic hygiene is a challenge. It’s an arduous task endorsed by WHO for increasing COVID-19 protection. The WASH Sector has installed 2600 handwashing locations in the communities and at the household level (Table 1). All refugees were supplied with soaps and stocked for up to 6 weeks. As the end of the dry season created severe water scarcity in the Teknaf area, WASH sector stored clean water for up to 1–6 weeks to supply in a truck if needed. Besides, approximately 1500 hygiene promoters worked to send key hygiene messages on COVID-19 to 35,000 households per week [2]. Moreover, the confines of WASH facilities may triggering the overall health conditions of the Rohingya refugees, specially, waterborne and infectious diseases.
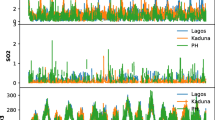
In the sampling camps where cleaner fuel liquid petroleum gas (LPG) use was less, fuelwood, kerosene cooking stoves and biomass burning increased the PM pollution. PM2.5 in the sampling camps varied from 44 μg/m3 to 546 μg/m3, whereas PM10 in the sampling camps varied from 125 μg/m3 to 1122 μg/m3, which was extremely higher than the guideline values (Fig. 1). Rohingya refugees, therefore, suffer from poor air quality as there is no separated kitchen area from the living space and inexistence of ventilation. Furthermore, the previous study confirmed that higher air pollution was related to patients with SARS death twice times likely [7]. People living with poor air quality may be more susceptible to COVID-19 [8]. Airborne PM2.5 & PM10 may put further risk of bioaerosols and airborne transmission of the COVID-19 virus. The overpopulated camps with the challenging physical, environmental and psychological conditions, social distancing is a hard job. The formation of isolation units and treatment services remains urgent precedence in and around the camps in Ukhiya and Teknaf. 329 isolation beds for the potential COVID-19 patients with 636 general beds for other health issues are prepared to address any outbreak responses [9]. In addition, there are no ventilators in the entire Cox’s Bazar district. This also means that there are no ventilators for the refugees and the lives will be lost when COVID-19 starts to spread widely in the community.
Measurement of particulate matter PM2.5 (a) and PM10 (b) collected from the kitchen and outside the house over a 4 h interval from 7 to 11 am cooking period from Rohingya camps 7, 9 and 13 from Ukhia, Cox’s Bazar District (c). The people who use LPG have significantly lower PM concentrations than the households using biomass fuel or kerosene. (d) Number of COVID-19 patients by districts in Bangladesh which include 5 patients detected in Cox’s Bazar District
Conclusion
Population density and social distancing is the key to combat COVID-19 pandemic. With the previous health conditions like HIV, STDs and other existing health conditions such as malnutrition, insufficient space accommodation, inadequate WASH resources in the refugee camps will widely and faster transmit the COVID-19 pandemic. The existing PM pollution may intensify the outbreak of COVID-19 pandemic in the camps, which will very likely diminish the entrée to the basic healthcare needs continuously being confronted with international and political interventions and tenacious disruption of the poor healthcare systems of Bangladesh. In this regard, the aid agencies have focused on supplying WASH kits and WASH training to the refugee children and adults which will likely to be effective. Moreover, the aid agencies and the GOB should focus on fast, easy and effective low-cost ventilators development using local resources as well as focus on the air pollution and nutritional management of the refugees to overcome the pandemic.
References
Cousins S. Rohingya threatened by infectious diseases. Lancet infect. Dis. 2018;18(6):609–10. https://doi.org/10.1016/s1473-3099(18)30304-9.
UNHCR 2020. Rohingya refugee response-Bangladesh operational dashboard: 2020 indicators monitoring.
Prothom Alo. 2020. Rohingyas at sea for 2 months, 32 die. https://en.prothomalo.com/bangladesh/rohingyas-at-sea-for-2-months-32-die accessed 20 April, 2020.
IEDCR/DGHS/GOB. 2020. Coronavirus COVID-19 Dashboard, 2020 http://103.247.238.81/webportal/pages/covid19.php?fbclid=IwAR0fvp1tINehCpQfHn8c6lCqwqMmjNncdLdhNqYLIsMAhaSxD2nM4Jd043Y
Hsan K, Griffiths MD, Gozal D, Rahman MA. HIV infection in Rohingya refugees in Bangladesh. Lancet HIV. 2019;6(7):e419. https://doi.org/10.1016/s2352-3018(19)30156-0.
Rahman MA, Shamol HH, Griffiths MD, Naher S, Hsan K. Factors associated with the practice of water, sanitation, and hygiene (WASH) among the Rohingya refugees in Bangladesh. J Water Sanit Hyg Dev. 2019;9(4):794–800. https://doi.org/10.2166/washdev.2019.038.
Cui Y, Zhang ZF, Froines J, Zhao J, Wang H, Yu SZ, et al. Air pollution and case fatality of SARS in the People’s Republic of China: an ecologic study. Environ Health. 2003;2(1):15. https://doi.org/10.1186/1476-069X-2-15.
WEF 2020. The deadly link between COVID-19 and air pollution. https://www.weforum.org/agenda/2020/04/the-deadly-link-between-covid-19-and-air-pollution/
Intersector Coordination group (ISG). 2020. COVID-19: Preparedness and response for the Rohingya refugee camps and host communities in Cox’s Bazar District Update #3. https://www.humanitarianresponse.info/sites/www.humanitarianresponse.info/files/documents/files/coxs_bazar_update_3_-_covid19_preparedness_and_response_final.pdf accessed 21 April 2020.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Highlights
•Densely populated Rohingya refugee camps are vulnerable amidst the COVID-19 pandemic
•Water, sanitation, and hygiene (WASH) education in the camps are a challenge
•Biomass burning in the camps increases airborne particulate matter (PM2.5 & 10) pollution
•PM, malnutrition and presence of HIV likely to increase the COVID-19 infections
Rights and permissions
About this article
Cite this article
Shammi, M., Robi, M.R. & Tareq, S.M. COVID-19: socio-environmental challenges of Rohingya refugees in Bangladesh. J Environ Health Sci Engineer 18, 1709–1711 (2020). https://doi.org/10.1007/s40201-020-00489-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40201-020-00489-6