Abstract
As part of its Medical Technology Evaluation Programme, the National Institute for Health and Care Excellence (NICE) invited a manufacturer to provide clinical and economic evidence for the evaluation of the Debrisoft® monofilament debridement pad for use in acute or chronic wounds. The University of Birmingham and Brunel University, acting as a consortium, was commissioned to act as an External Assessment Centre (EAC) for NICE, independently appraising the submission. This article is an overview of the original evidence submitted, the EAC’s findings and the final NICE guidance issued. The sponsor submitted a simple cost analysis to estimate the costs of using Debrisoft® to debride wounds compared with saline and gauze, hydrogel and larvae. Separate analyses were conducted for applications in home and applications in a clinic setting. The analysis took an UK National Health Service (NHS) perspective. It incorporated the costs of the technologies and supplementary technologies (such as dressings) and the costs of their application by a district nurse. The sponsor concluded that Debrisoft® was cost saving relative to the comparators. The EAC made amendments to the sponsor analysis to correct for errors and to reflect alternative assumptions. Debrisoft® remained cost saving in most analyses and savings ranged from £77 to £222 per patient compared with hydrogel, from £97 to £347 compared with saline and gauze, and from £180 to £484 compared with larvae depending on the assumptions included in the analysis and whether debridement took place in a home or clinic setting. All analyses were severely limited by the available data on effectiveness, in particular a lack of comparative studies and that the effectiveness data for the comparators came from studies reporting different clinical endpoints compared with Debrisoft®. The Medical Technologies Advisory Committee made a positive recommendation for adoption of Debrisoft® and this has been published as a NICE medical technology guidance (MTG17).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Debrisoft® is convenient and easy to use, is well-tolerated by adults and children, and can result in quicker debridement of chronic or acute wounds with fewer nurse visits needed than other debridement methods. Debridement is an important component of standard wound care management, as described in clinical guidelines on pressure ulcers [National Institute for Health and Care Excellence (NICE) clinical guideline 179] and diabetic foot problems (NICE clinical guideline 119). |
Debrisoft® is estimated to be cost saving for complete debridement compared to other methods such as hydrogel, gauze and bagged larvae. |
1 Introduction
The National Institute for Health and Care Excellence (NICE) produces evidence-based medical technologies guidance with the overall aim of evaluating, and where appropriate encouraging, the adoption of novel and innovative medical devices and diagnostics within the National Health Service (NHS) in England. Manufacturers or distributors of potentially eligible technologies notify their products to NICE’s Medical Technologies Evaluation Programme (MTEP). Technologies are selected for evaluation by MTEP if they have the potential to offer significant clinical benefits to patients and the NHS or reduce the cost compared with current standard practice. Guidance is produced after clinical and cost evidence submitted by the sponsor is independently assessed by an External Assessment Centre (EAC) and after a public consultation period. Devices and diagnostic tools with more complex value propositions can be routed for evaluation through other NICE programmes such as the Diagnostics Assessment Programme or Technology Appraisals. Campbell and Campbell (2012) describe the methods of MTEP in more detail [1].This article presents a summary of the EAC report for the Debrisoft® monofilament debridement pad (Lohmann & Rauscher GmbH & Co. KG, Neuwied, Germany) for use in acute or chronic wounds. It is part of a series of NICE Medical Technology Guidance summaries being published in Applied Health Economics and Health Policy [2, 3].
2 Background to the Condition and its Treatment
Skin wounds are a very common condition and can be acute or chronic. Acute wounds occur from cuts, burns, abrasions or pressure on the skin. Some acute wounds become chronic, particularly if there is underlying pathology, e.g. diabetes mellitus or poor venous drainage. Chronic wounds include pressure ulcers, diabetic foot ulcers, and venous and arterial leg ulcers.
In the UK in 2008, approximately 200,000 people had chronic wounds. These wounds include leg, pressure and foot ulcers [4]. Leg ulcers affect 1 in 500 people, although this rises sharply with an increase in age, to 1 in 50 in those over the age of 80 years [5]. In the UK, the annual incidence for foot ulcers among people with diabetes is 2–5 %, with the annual incidence of amputation being 0.25–1.8 % [6]. Approximately 10 % of all leg ulcers are caused by arterial ulcers.
Lymphoedema is a chronic condition that is characterised by oedema. Primary lymphoedema, an inherited condition, occurs in 1 in 10,000 people and mainly affects the legs, whereas secondary lymphoedema, caused by an injury to the lymph system, affects approximately 100,000 people in total in the UK [7] and can affect the legs and arms, depending on cause.
In any given year, just under half a million people in the UK will developing at least one pressure ulcer, usually people with an underlying health condition. Around 1 in 20 people who are admitted to hospital with an acute (sudden) illness will develop a pressure ulcer [8].
Debridement is the removal of devitalised, contaminated or foreign material from the surface of a wound with the intension to expose healthy tissue. The main methods of debridement are mechanical, sharp, larvae (loose or bagged), autolytic, enzymatic or surgical. These methods have different characteristics, speeds of conduct, advantages and disadvantages, and can be conducted by different groups of healthcare professionals (see Table 1). It is widely believed that wound healing is enhanced by the practice of debridement, but there is little conclusive proof. An early health technology assessment found no randomised controlled trials (RCTs) comparing debridement to no debridement in chronic wounds [9], but a more recent review on debridement methods has shown there may be some RCTs [10], although the descriptions of the primary study control groups in this review are unclear. A recent Cochrane review on debridement in diabetic foot ulcers has claimed that direct evidence on debridement versus no debridement is lacking [11]. There have been no large, good-quality RCTs of debridement versus no debridement in any acute or chronic wounds, so whether it is beneficial or not in acute or chronic wounds is unclear. RCTs found include one on surgical debridement in chronic venous ulcers which showed that 16 % of 28 ulcers had complete healing in the debridement group compared with 4.3 % of 27 ulcers in the control group [12]. Another on surgical debridement [13] found that 21 of 22 (95 %) ulcers treated with surgical debridement had completely healed within 6 months, compared with 19 of 24 (79 %) in the conservative care group. An early RCT on debridement versus no debridement in acute wounds (gunshot) found that slightly more patients in the debridement group (4 of 89) got wound infections than those in the control group (2 of 74) [14]. A recent US cohort study of a large number of patients with a variety of mainly chronic wounds found that those wounds receiving more frequent debridement had faster healing rates on average [15]. However, the results may be confounded by a variety of factors such as patient characteristics, nursing care experienced and debridement methods used. Nevertheless, it seems to be generally accepted by most wound care practitioners that debridement is mostly beneficial.
With regard to effectiveness of debridement, good comparative evidence does exist on the comparators, e.g. is a large cohort study was published recently of 312,744 wounds (154,664 patients, median age 69 years) looking at frequency of debridement and time to heal [15]. The debridement methods included autolytic, enzymatic, mechanical, surgical and biosurgical (larvae). The wound types were a wide variety of chronic wounds. The study found that more debridements per wound resulted in faster healing times. A Cochrane review of debridement of diabetic foot ulcers [11] included RCTs on larvae compared with hydrogel [16] and hydrogel compared with gauze/standard care [17–19]. A Cochrane review of debridement of surgical wounds [20] included RCTs of hydrogel compared with gauze [21, 22].
3 The Decision Problem
3.1 Population
The target population was adults or children requiring debridement of an acute or chronic wound in a community-based setting. The skin could be intact (closed wounds) or non-intact (open wounds). The sponsor evaluated adults with chronic wounds and did not investigate the subgroup of open and closed wounds. There was a considerable lack of clarity over normal debridement practice in a standard NHS community setting.
3.2 Intervention
The intervention was Debrisoft® monofilament debridement pad, which is a square pad measuring 10 × 10 cm that has monofilament polyester fibres projecting from the wound contact side, making it feel soft and fleecy. The pad is used when moistened with water and is gently rubbed over wound or skin surfaces, and is intended to facilitate the removal of dead or damaged tissue, etc. The claimed benefits of Debrisoft® include reduction in pain, improved acceptability, faster treatment and healing, reduced risks of trauma to healthy tissue, and of bleeding, reduced time and resources needed, lower costs and shorter waiting times, more effective debridement, improved patient concordance and avoidance of ongoing costs relating to specialist methods of debridement.
3.3 Comparators
The scope comparators were hydrogels or other autolytic dressings, or cleansing with gauze. The sponsor also evaluated the use of larvae. It was unclear whether the gauze use was wet to dry debridement or just wet cleansing.
3.4 Outcomes
Outcomes, including surrogate outcomes, listed in the scope included wound healing, quality of life, time to complete debridement, number of debridements required, number of dressings required, types of dressings required and the need to refer to a tissue viability nurse or hospital specialist clinic. Adverse effects included pain, wound infections, cellulitis and trauma to healthy tissue.
4 Review of the Clinical and Economic Evidence
The sponsor submitted clinical and economic evidence based on the scope issued by NICE. The economic evidence included a de novo economic model. The EAC critically appraised the submission and carried out additional analyses to evaluate the outcomes identified in the scope.
4.1 Clinical Effectiveness Evidence
4.1.1 Sponsor’s Review of Clinical Effectiveness Evidence
The sponsor submitted 51 studies in the qualitative synthesis. However, many of these were single case studies or testimonials, some within larger documents. They included eight journal articles, 28 conference posters and two advertising reports sponsored by the company that included multiple case studies. There were several multiple patient case series submitted. Bahr et al. [23] and Mustafi et al. [24] compared the overall mean time of each debridement session, using the Debrisoft® pad, with hydrogel, gauze and surgical debridement in 60 patients. Gray et al. [25] described a case series of 18 patients that evaluated which types of slough and necrotic tissue benefit most from debridement with the Debrisoft® pad. Haemmerle et al. [26] described a case series of 11 patients with chronic wounds from two hospitals. Johnson et al. [27] described a two-centre observational study that compared the effectiveness of the Debrisoft® pad with other non-specified debridement methods. Ten patients were recruited from each centre. Stephen-Haynes and Callaghan [28] evaluated the use of the Debrisoft® pad by 40 tissue viability nurses, over a 12-week period, on a wound or hyperkeratosis.
4.1.2 Critique of Clinical Effectiveness Evidence
As the claimed benefits for Debrisoft® were all comparative statements, only evidence with comparators was evaluated. These were journal articles by Bahr et al. [23] and Johnson et al. [27], and conference posters by Callaghan and Stephen-Haynes [29], Collarte [30], Mustafi et al. [24], Pietroletti et al. [31] and Wiser [32]. The characteristics of these studies are in Table 2.
An attempt was made to match the claimed benefits of Debrisoft® to the comparative evidence available. Table 3 shows all of the numerical comparative results found. Some of the included studies reported comparative results narratively. Wiser [32] reported reduction of pain, more effective debridement and improved acceptability with Debrisoft® compared with saline soaks. Collarte [30] reported a decreased time to treat with Debrisoft® compared with standard treatment (not otherwise specified) and that autolytic debridement took significantly longer. Collarte also reported that Debrisoft® removed more devitalised tissue and hyperkeratosis more quickly. Callaghan and Stephen-Haynes [29] reported a reduction in wound care visits for Debrisoft®, but it was not clear what the comparator was. They also reported that there were significant differences compared with gauze and sharp debridement. Pietroletti et al. [31] reported that Debrisoft® was not as expensive as current debridement methods (not otherwise specified).
The comparative evidence suggested that Debrisoft® was associated with less pain, improved acceptability by patients, decreased time to treat, reduction in wound care visits, more removal of devitalized tissue and more effective debridement than standard treatment, previous methods (not specified), gauze, autolytic, enzymatic or sharp/scalpel debridement. There was no comparative evidence on larvae found. It can be seen that there is no comparative information on most of the claimed benefits, particularly healing rates, compared with the comparators listed in the scope and to larvae (see Table 3). There was no useful evidence on the rate of wound healing or wound infections. There was no information on the mean number of applications required with Debrisoft® to achieve complete debridement.
No comparative results on adverse events were presented by the sponsor. It is currently unclear if use of Debrisoft® is associated with higher rates of wound infections than the comparators of gauze, hydrogel or larvae. It is also unclear if use of Debrisoft® is associated with higher or lower rates of pain in the patient than the comparators of gauze, hydrogel or larvae. The NICE expert advisers have not voiced a clear opinion about adverse events with the use of Debrisoft® compared with the comparators of gauze, hydrogel or larvae.
4.2 Economic Evidence
4.2.1 Sponsor’s Economic Submission
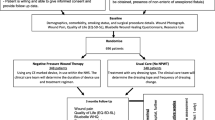
The sponsor conducted a systematic search of economic evidence from the literature but this did not identify any studies reporting data on the costs or cost effectiveness of Debrisoft®. In the absence of an appropriate published analysis, the sponsor submitted a de novo analysis using a simple cost model executed in Microsoft Excel®. The model estimated the cost and resource consequences of Debrisoft® used in a community setting compared with hydrogel, gauze and larvae. Separate analyses were conducted for applications in home and clinic settings. All analyses were based on an NHS perspective. No distinction was made between adults and children, or between chronic and acute wounds.
The stated time horizon of the analysis was to complete debridement. The clinical pathway reflected in the model included the following five stages: (1) an assessment of the skin and wound by a district nurse; (2) ordering the debridement agent if not available to the district nurse immediately; (3) application of the debridement agent by a district nurse; (4) re-assessment of the wound; and (5) further applications of the debridement agents until debridement is judged to be complete.
The effectiveness data used in the analysis came from three separate sources (see Table 4). Data on the mean number of applications to achieve wound healing from a published randomised trial were used to inform the effectiveness of larvae and hydrogel [33, 34]. The effectiveness of Debrisoft® was based on the percentage of wounds completely debrided after three applications as reported in the case series study by Bahr et al. [23]. This reported that 77 % of wounds were completely debrided with Debrisoft® after three applications. For gauze, the effectiveness data were based on clinical opinion of the number of applications required to achieve complete debridement. A summary of the effectiveness data used in the model is presented in Table 4. The model did not include adverse events associated with any of the technologies.
Given the differences in outcome measures used to inform clinical effectiveness in the model, particularly the lack of data on the mean number of applications for Debrisoft® to achieve debridement, the sponsor employed a ‘stopping rule’ for Debrisoft® in the analysis. This assumed that if the wound was not completely debrided after three applications of Debrisoft®, patients would switch to the use of hydrogel for complete debridement. No stopping rule was employed for the other debridement agents.
Resource use included the debridement agents (Debrisoft®, hydrogel, gauze and larvae), supplementary technologies (cover dressings: film and absorbent dressings; dressing packs) and district nurse visits (at home or clinic). The amount of debridement agents required was based on the amount needed to debride a wound of 10 × 10 cm. The cost of larvae was based on the costs of loose larvae and obtained directly from a supplier. The cost of hydrogel was based on the median cost of all formulations listed in the British National Formulary (BNF) [35]. Unit costs were obtained from published sources and were expressed in 2012–2013 Great Britain pounds sterling (reported in Table 5).
The number of visits by a district nurse required to apply the debridement agent varied according to setting (clinic or home) and comparator. The number and length of district nurse visits were based on expert opinion. Gauze (clinic and home settings) and hydrogel (clinic setting only) are assumed to be available to the nurse immediately and require a total of two visits for the first application (one to assess the wound and apply the debridement product; the second to reassess the wound and reapply the product if needed) plus one visit for each subsequent application. It was assumed that hydrogel would require ordering by the district nurse in the home setting following the initial assessment, similar to larvae in both the home and clinic settings. Therefore, additional visits are included for the first application of hydrogel in the home setting and for the first and all sequent applications of larvae in the home and clinic settings. All district nurse visits were assumed to last 15 min.
The sponsor conducted deterministic sensitivity analyses on the number of debridement applications, the number of district nurse visits and unit costs of debridement agents (all increased and decreased by an arbitrary 20 %). Probabilistic analyses were not presented.
The baseline results of the sponsor’s analysis are presented in Table 6. Debrisoft® was cost saving compared with all three comparators in both the home and clinic settings. Debrisoft® remained cost saving in all sensitivity analyses.
4.2.2 Critique of Economic Evidence
Overall, the pathway of care reflected in the sponsor’s economic model appeared to be appropriate. The time horizon of the analysis was until debridement rather than to wound healing, which may have been a more meaningful endpoint as it could reflect that some wounds will require multiple debridements. Time to wound healing has been used as the endpoint in previous clinical trials of debridement, including the main source of effectiveness used in the sponsor’s analysis for hydrogel and larvae [33].
The main drivers of the cost analysis were the number of applications required to debride the wound and number of visits required per application for each product. Although the stated time horizon was until complete debridement, the effectiveness data used for two of the comparators in the analysis (larvae and hydrogel) did not reflect this endpoint. The data on the number of applications for larvae and hydrogel came from a randomised clinical trial of the products with a primary endpoint of wound healing and an average follow-up of 1 year. The data from these studies used in the analysis reflected the average number of applications until wound healing rather than the number of applications to achieve complete debridement. The effectiveness data used for Debrisoft® were not comparable and based on the percentage of wounds successfully debrided after three applications at 12 days of follow-up from the case series study [23]. This study found that 77 % of wounds were completely debrided at 12 days; however, following clarification, the sponsor confirmed that this endpoint was not pre-specified in the analysis plan for the trial. This lack of information from a direct comparison or network meta-analysis for the main effectiveness data used in the economic analysis is likely to lead to bias in the comparison of the number of applications for each of the products; however, it is difficult to judge the likely impact of this on the results.
To compensate for the lack of comparability in the effectiveness outcomes used in the analysis, the sponsor employed a ‘stopping rule’ for Debrisoft®. The advice from a NICE clinical expert was that two to three applications of Debrisoft® would usually be required to debride a hard eschar, and one application for a sloughy wound. Based on this advice, the assumptions around the number of applications of Debrisoft® per debridement may be reasonable.
The time taken by the district nurse visit was based on advice from clinical experts and differs to estimates reported in a randomised trial of hydrogel and larvae in which the length of appointments was measured directly [36]. This trial reported the average duration of clinic visits to be 22 and 40 min for home visits.
The costs of larvae included in the analysis are based on the costs of loose larvae. Advice from a NICE clinical advisor was that bagged larvae would be used in UK clinical practice. This would have the effect of making larvae more expensive relative to Debrisoft®.
Further alternative feasible assumptions around the amount and costs of dressings could have been included in the sponsor’s analysis. Additional film and absorbent dressings would not be required prior to debridement, specifically at the first appointment if the debridement product has to be ordered by the district nurse. Also, the unit costs for these dressings, gauze and hydrogels were based on the median unit costs for each type of technology listed in the BNF. We considered that, given the assumption of equal efficacy in the model, it would be appropriate to use the lowest unit cost for each technology to reflect cost-effective practice.
4.2.3 Supplementary Economic Analyses Conducted by the External Assessment Centre
Upon review of the economic model, the EAC identified some errors in the sponsor’s analysis. These included the incorrect implementation of the stopping rule for Debrisoft® and a miscalculation in the unit costs of a district nurse visit at home. The estimates of the district nurse costs appear to have come from a misunderstanding regarding the apportionment of travel costs and the unit costs for nurses with qualifications in the original estimates. The results of the cost analysis after correcting these errors are presented in Table 6 (‘EAC corrected analysis’).
Further changes were made by the EAC to reflect alternative assumptions in the economic model. Firstly, the costs of larvae were amended to the bagged variety. Secondly, the costs of additional dressings when patients did not undergo debridement were removed. Thirdly, the time taken for each district nurse visit was amended to that reported in the published trial of hydrogel and larvae [36]. Finally, the unit costs of dressings, gauze and hydrogels were amended to the cheapest listed in the BNF. The impact of all of these changes on the results is shown in Table 6 (‘EAC amendments’). The use of the costs of bagged larvae led to a substantial increase in the costs of this comparator relative to Debrisoft®. The amendments to the nursing time also had an impact on the results, increasing the estimated cost savings for Debrisoft® relative to gauze and hydrogel, particularly in the home setting. The other amendments to the dressings had only a marginal impact.
The EAC also conducted further exploratory analyses. These included removing the stopping rule from the analysis and a threshold analysis to assess how many applications of Debrisoft® would be required for it to no longer be the cheapest option, keeping all other variables constant. The starting point for these analyses was the analysis after correcting for errors and employing alternative assumptions (‘EAC amendments’). We found that, without the stopping rule, Debrisoft® would no longer be the cheapest alternative if more than nine applications were required. With the stopping rule, this decreased to seven applications (Table 7).
Finally, the EAC requested sight of a further analysis to reflect some different assumptions, specifically: (1) an additional five nurse visits for each larvae application, each with an average duration of 15 min; (2) one home visit for the first application of Debrisoft® (to reflect the assumption that nurses have immediate access to Debrisoft® at their first home visit and there is no need to order it); and (3) only two home visits for the first application of hydrogel (to reflect the assumption that nurses have immediate access to hydrogel at their first home visit and there is no need to order it). The results are shown in Table 6 (‘Committee-requested analysis’). The results showed that Debrisoft® remained cost saving using these alternative assumptions.
In summary, the sponsor concluded that Debrisoft® is cost saving for use in the debridement of wounds compared with larvae, gauze and hydrogel. This result remained robust to most analyses conducted by the EAC. Cost savings ranged from £77 to £222 per patient compared to hydrogel, from £97 to £347 compared with saline and gauze, and from £180 to £484 compared with larvae depending on the assumptions included in the analysis and whether applied in a home or clinic setting (see Table 6). The results are driven largely by the requirement for fewer appointments with Debrisoft® than with hydrogel and gauze in the analysis, and from cheaper product costs for Debrisoft® relative to larvae. All analyses are severely limited by a lack of comparative data for Debrisoft® compared with hydrogel, larvae or gauze. The threshold analysis indicates that Debrisoft® is likely to be cost saving for most applications for an endpoint of debridement.
5 NICE Guidance
5.1 Preliminary Guidance
The evidence submitted by the sponsor and the EAC’s critique of this evidence was presented to the Medical Technologies Advisory Committee who provided draft recommendations relating to the Debrisoft® monofilament debridement pad following their meeting in December 2013. These were as follows [37]:
-
1.
“The case for adopting the Debrisoft® monofilament debridement pad as part of the management of acute or chronic wounds in the community is supported by the evidence. The available evidence is limited, but the likely benefits of using the Debrisoft pad on appropriate wounds are that they will be fully debrided more quickly, with fewer nurse visits needed, compared with other debridement methods. In addition, the Debrisoft pad is convenient and easy to use, and is well tolerated by patients. Debridement is an important component of standard woundcare management as described in Pressure ulcers (NICE clinical guideline 29) [now replaced by guideline 179] and Diabetic foot problems (NICE clinical guideline 119)” [38, 39].
-
2.
“The Debrisoft pad is indicated for adults and children with acute or chronic wounds. The available evidence is predominantly in adults with chronic wounds needing debridement in the community. The data indicate that the device is particularly effective for chronic sloughy and hyperkeratotic wounds.”
-
3.
“The Debrisoft pad is estimated to be cost saving for complete debridement when compared with other debridement methods. Cost savings per patient (per complete debridement) are estimated to be £99, £152 and £484 compared with hydrogel, gauze and bagged larvae respectively in a community clinic and £222, £347 and £469 respectively in the home.”
5.2 Consultation Response
During consultation, NICE received 26 consultation comments from six consultees. As a result of these comments, the technology description was improved and updated and the comparator types were clarified, but the recommendations did not change significantly. Section 4.5 was updated to state that nurses and other healthcare professionals should only use Debrisoft® after appropriate training in its indications and safe application.
6 Key Challenges and Learning Points
The Committee agreed with the EAC’s conclusions that there was a lack of good-quality comparative evidence. The EAC considered that there was insufficient robust evidence to demonstrate that Debrisoft® is clinically more effective than other methods for wound healing and wound infections. It would be better to measure outcomes to wound healing because this is a clinically much more important outcome and there does not appear to be a strong correlation between achieving complete debridement and subsequent wound healing. In the VenUS II trial [33, 40], a significant difference in debridement but no difference in time to healing was found. The sponsor agreed that there was a lack of evidence on wound healing:
“the complete healing outcome would bring in all sorts of confounding variables and the comparison of the benefits between debriding alternatives would be lost in the impact of the variables to complete wound healing, i.e. the physiology of the patient, background disease, effect of arterial status etc.”
[41]
Also, “The evidence base is not sufficient at this time to allow a meaningful analysis of costs or time to complete healing with debrisoft compared with other debridement methods in scope (hydrogel or other autolytic dressing, and cleansing with gauze)”.
The EAC noted that the available evidence is mainly in adults with chronic wounds and accepted that there is little evidence specific to children or the debridement of acute wounds. The EAC also noted, from the limited available evidence, that the Debrisoft® pad is particularly suited to the debridement of sloughy wounds with exudate and hyperkeratotic skin.
The EAC’s decision to recommend Debrisoft® was based on an evaluation of complete debridement which suggested that Debrisoft® may be cheaper overall than larvae, hydrogel and debridement with gauze (which is apparently not used in the UK, according to NICE clinical experts). The limited evidence available for Debrisoft® meant it was not possible to consider longer-term outcomes such as time to healing, adverse events, hospital visits, etc. There is no information on debridement methods currently being used by nurses or other health professionals in the community in the UK.
The EAC considered that an RCT of Debrisoft® compared with normal current practice in the community is needed. We suggest that follow-up should be to wound healing. Outcomes would also include wound infections, costs and quality of life. It would require that the number of applications of the debridement technique would need to reflect the number of applications required in clinical practice, rather than having the trial restricted to a fixed number. The RCT that is currently ongoing is not helpful in this respect because the protocol has no mention of time to healing as an outcome measure or of wound infection rates [42]. Also, an audit of current debridement practice in community health practice in the UK would be very helpful.
References
Campbell B, Campbell M. NICE Medical Technologies Guidance: a novel and rigorous methodology to address a new health technology assessment challenge. Appl Health Econ Health Policy. 2012;10(5):295–7.
White J, Carolan-Rees G. PleurX peritoneal catheter drainage system for vacuum-assisted drainage of treatment-resistant, recurrent malignant ascites. Appl Health Econ Health Policy. 2012;10(5):299–308.
Withers K, Carolan-Rees G, Dale M. Pipeline embolization device for the treatment of complex intracranial aneurysms: a NICE Medical Technology Guidance. Appl Health Econ Health Policy. 2013;11(1):5–13.
Posnett JFP. The burden of chronic wounds in the UK. Nurs Times. 2008;104(3):44–5.
Venous leg ulcer: NHS Choices; 2014. http://www.nhs.uk/conditions/Leg-ulcer-venous/Pages/Introduction.aspx. Accessed Jul 2014.
Hunt DL. Diabetes: foot ulcers and amputations. BMJ Clinical Evidence. 2011. http://clinicalevidence.bmj.com/x/systematic-review/0602/overview.html. Accessed Jul 2014.
Lymphoedema: NHS Choices; 2014. http://www.nhs.uk/conditions/Lymphoedema/Pages/Introduction.aspx. Accessed Jul 2014.
Pressure ulcers: NHS Choices; 2014. http://www.nhs.uk/conditions/Pressure-ulcers/Pages/Introduction.aspx. Accessed Jul 2014.
Bradley M, Cullum N, Sheldon T. The debridement of chronic wounds: a systematic review. Health Technol Assess. 1999;3(17 Pt 1):iii–iv.
Doerler M, Reich-Schupke S, Altmeyer P, Stucker M. Impact on wound healing and efficacy of various leg ulcer debridement techniques. J Deutsch Dermatol Ges. 2012;10(9):624–32.
Edwards J, Stapley S. Debridement of diabetic foot ulcers. Cochrane Database Syst Rev. 2010;1:CD003556.
Williams D, Enoch S, Miller D, Harris K, Price P, Harding KG. Effect of sharp debridement using curette on recalcitrant nonhealing venous leg ulcers: a concurrently controlled, prospective cohort study. Wound Repair Regen. 2005;13(2):131–7.
Piaggesi A, Schipani E, Campi F, Romanelli M, Baccetti F, Arvia C, et al. Conservative surgical approach versus non-surgical management for diabetic neuropathic foot ulcers: a randomized trial. Diabet Med. 1998;15(5):412–7.
Brunner RG, Fallon WF Jr. A prospective, randomized clinical trial of wound debridement versus conservative wound care in soft-tissue injury from civilian gunshot wounds. Am Surg. 1990;56(2):104–7.
Wilcox JR, Carter MJ, Covington S. Frequency of debridements and time to heal: a retrospective cohort study of 312744 wounds. JAMA Dermatol. 2013:E1-E9.
Markevich YO, McLeod-Roberts J, Mousley M, Melloy E. Maggot therapy for diabetic neuropathic foot wounds [abstract]. Diabetologia: Proceedings of the 36th annual meeting of the European Association for the Study of Diabetes. 2000;43(Suppl 1):A15.
Jensen JL, Seeley J, Gillin B. Diabetic foot ulcerations. A controlled, randomized comparison of two moist wound healing protocols: Carrasyn Hydrogel Wound dressing and wet-to-moist saline gauze. Adv Wound Care. 1998;11(7 Suppl):1–4.
D’Hemecourt PA, Smiell JM, Karim MR. Sodium carboxymethyl cellulose aqueous-based gel vs becaplermin gel in patients with nonhealing lower extremity diabetic ulcers. Wounds. 1998;10(3):69–75.
Vandeputte JAJ, Gryson LGM. Diabetic foot infection controlled by immuno-modulating hydrogel containing 65% glycerine. Presentation of a clinical trial [poster]. 6th European Conference on Advances in Wound Management; 1–4 Oct 1996, Amsterdam.
Smith F, Dryburgh N, Donaldson J, Mitchell M. Debridement for surgical wounds. Cochrane Database Syst Rev. 2013;9:CD006214.
Goode AW, Glazer G, Ellis BW. The cost effectiveness of dextranomer and eusol in the treatment of infected surgical wounds. Br J Clin Pract. 1979;33(11–12):325.
Michiels I, Christiaens MR. Dextranomer (Debrisan) paste in post-operative wounds. A controlled study. Clin Trials J. 1990;27(4):283–90.
Bahr S, Mustafi N, Hattig P, Piatkowski A, Mosti G, Reimann K, et al. Clinical efficacy of a new monofilament fibre-containing wound debridement product. J Wound Care. 2011;20(5):242–8.
Mustafi N, et al. Clinical efficacy of a monofilament fibre containing wound debridement product evaluated in multicentre real life study [poster]. EWMA Conference; 25–27 May 2011, Brussels.
Gray D, Cooper P, Russell F, Stringfellow S. Assessing the clinical performance of a new selective mechanical debridement product. Wounds UK. 2011;7(3):42–6.
Haemmerle G, Duelli H, Abel M, Strohal R. The wound debrider: a new monofilament fibre technology: results of a pilot study [poster]. EWMA Conference; 25–27 May 2011, Brussels.
Johnson S, Collarte A, Lara L, Alberto A. A multi-centre observational study examining the effects of a mechanical debridement system. J Community Nurs. 2012;26(6):43–7.
Stephen-Haynes J, Callaghan R. A new debridement technique tested on pressure ulcers. Wounds UK. 2012;8(3 suppl):S6–11.
Callaghan R, Stephen-Haynes J. Changing the face of debridement in pressure ulcers [poster]. Wounds UK Conference; Nov 2012, Harrogate.
Collarte A. Evaluation of a new debridement method for sloughy wounds and hyperkaratotic skin for a non-specialist setting [poster]. EWMA Conference; 25–27 May 2011, Brussels.
Pietroletti R, Capriotti I, Di Nardo R, Mascioli P, Gonzales M, Ermolli R. Economical comparison between three different types of debridement (autolytic and enzymatic vs mechanical debridement with polyester fibres) [poster]. Wounds UK Conference; Nov 2012, Harrogate.
Wiser M. A monofilament debridement product—is it a new support debridement? [poster]. EWMA Conference; May 2012, Vienna.
Dumville JC, Worthy G, Soares MO, Bland JM, Cullum N, Dowson C, et al. VenUS II: a randomised controlled trial of larval therapy in the management of leg ulcers. Health Technol Assess. 2009;13(55):1–182.
Raynor P, Dumville J, Cullum N. A new clinical trial of the effect of larval therapy. J Tissue Viability. 2004;14(3):104–5.
British National Formulary. London: BMA/Royal Pharmaceutical Society; 2012.
Soares MO, Iglesias CP, Bland JM, Cullum N, Dumville JC, Nelson EA, et al. Cost effectiveness analysis of larval therapy for leg ulcers. BMJ. 2009;338:b825.
NICE. The Debrisoft monofilament debridement pad for use in acute or chronic wounds: guidance consultation. https://www.nice.org.uk/guidance/mtg17/documents/the-debrisoft-monofilament-debridement-pad-for-use-in-acuteor-chronic-wounds-guidance-consultation2. Accessed 10 Aug 2015.
NICE. Pressure ulcers clinical guideline (CG179). London/Manchester: NICE; 2014.
NICE. Diabetic foot problems clinical guideline (CG119). London/Manchester: NICE; 2011.
Dumville JC, Worthy G, Bland JM, Cullum N, Dowson C, Iglesias C, et al. Larval therapy for leg ulcers (VenUS II): randomised controlled trial. BMJ. 2009;338:b773.
Meads C, Lovato E, Longworth L. External Assessment Centre report. Debrisoft monofilament debridement pad for the debridement of acute and chronic wounds. 2013. http://www.nice.org.uk/guidance/mtg17/documents/the-debrisoft-monofilament-debridement-pad-for-use-in-acute-or-chronicwounds-external-assessment-centre-assessment-report2. Accessed Sept 2013.
Clark M. Comparison of cleaning of leg ulcers using pads or wound dressings. ISRCTN Registry; 2015. http://www.isrctn.com/ISRCTN47349949. Accessed July 2015.
Strohal R, Apelqvist J, Dissemond J, O’Brien JJ, Piaggeri A, Rimdeika R, et al. EWMA document: debridement. J Wound Care. 2013;1:S1–52.
Callaghan R, Haynes SJ. Changing the face of debridement in pressure ulcers [poster]. EPUAP Conference; Sep 2012, Cardiff.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
The Birmingham and Brunel Consortium is funded by NICE to act as an External Assessment Centre for the Medical Technologies Evaluation Programme. This summary of the Medical Technology Guidance was produced following publication of the final guidance report. This summary has been reviewed by NICE, but has not been externally peer reviewed by Applied Health Economics and Health Policy. The authors have no conflicts of interest to report.
Author contributions
This manuscript was prepared by CM, with contributions from EL and LL. The EAC report was prepared by CM, EL and LL. CM and EL critically appraised the economic and clinical evidence submitted by the sponsor; and EL and LL critiqued the submitted cost model. CM is the guarantor for the overall content.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Meads, C., Lovato, E. & Longworth, L. The Debrisoft® Monofilament Debridement Pad for Use in Acute or Chronic Wounds: A NICE Medical Technology Guidance. Appl Health Econ Health Policy 13, 583–594 (2015). https://doi.org/10.1007/s40258-015-0195-0
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40258-015-0195-0