Abstract
Background and Objectives
Apixaban and enoxaparin are indicated for preventing venous thromboembolism (VTE). The aim of this study was to evaluate the cost effectiveness of apixaban versus enoxaparin for the prophylaxis of VTE and associated long-term complications in Chinese patients after total knee replacement (TKR).
Methods
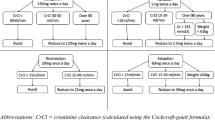
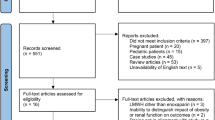
A decision model, which included both acute VTE (represented as a decision tree) and the long-term complications of VTE (represented as a Markov model), was developed to assess the economic outcomes of the two prophylactic strategies for Chinese patients after TKR. Transition probabilities, costs, and utilities were derived from published literature. One-way and probabilistic sensitivity analyses were performed to test the uncertainty concerning the model parameters. Quality-adjusted life-years (QALYs) and direct medical costs were reported over a 5-year horizon. Incremental cost-effectiveness ratios (ICERs) were also calculated.
Results
Thromboprophylaxis with apixaban was estimated to have a higher cost (US$68) and more health benefits (0.0006 QALYs) than thromboprophylaxis with enoxaparin over a 5.5-year time horizon, resulting in an ICER of US$108,497 per QALY gained. One-way sensitivity analyses found that the cost of apixaban and the probability of pulmonary embolism when taking either apixaban or enoxaparin had a considerable impact on the model outcomes.
Conclusions
Overall, the analysis found that the use of enoxaparin in Chinese patients after TKR was likely to be more cost effective than the use of apixaban.



Similar content being viewed by others
References
Turpie AGG, Bauer KA, Eriksson BI, Lassen MR, For the Steering Committess of the Pentasaccharide Orthopedic Prophylaxis Studies. Fondaparinux vs enoxaparin for the prevention of venous thromboembolism in major orthopedic surgery: a meta-analysis of 4 randomized double-blind studies. Arch Intern Med. 2002;162(16):1833–40.
Goldhaber SZ, Bounameaux H. Pulmonary embolism and deep vein thrombosis. Lancet. 2012;379(9828):1835–46.
Ruppert A, Steinle T, Lees M. Economic burden of venous thromboembolism: a systematic review. J Med Econ. 2011;14(1):65–74.
MacDougall DA, Feliu AL, Boccuzzi SJ, Lin J. Economic burden of deep-vein thrombosis, pulmonary embolism, and post-thrombotic syndrome. Am J Health Syst Pharm. 2006;63(20 Suppl 6):S5–15.
Geerts WH, Bergqvist D, Pineo GF, Heit JA, Samama CM, Lassen MR, et al. Prevention of venous thromboembolism. Chest. 2008;133(6):381S–453S.
Piovella F, Wang CJ, Lu H, Lee K, Lee LH, Lee WC, et al. Deep-vein thrombosis rates after major orthopedic surgery in Asia. An epidemiological study based on postoperative screening with centrally adjudicated bilateral venography. J Thromb Haemost. 2005;3(12):2664–70.
Chinese Orthopaedic Association. Guidelines for deep venous thrombosis prophylaxis during Orthopaedic surgery. Chin J Orthop. 2009;29(6):602–4.
Mandernach MW, Beyth RJ, Rajasekhar A. Apixaban for the prophylaxis and treatment of deep vein thrombosis and pulmonary embolism: an evidence-based review. Ther Clin Risk Manag. 2015;11:1273–82.
Lassen MR, Gallus A, Raskob GE, Pineo G, Chen D, Ramirez LM, et al. Apixaban versus enoxaparin for thromboprophylaxis after hip replacement. N Engl J Med. 2010;363(26):2487–98.
Sullivan SD, Kahn SR, Davidson BL, Borris L, Bossuyt P, Raskob G. Measuring the outcomes and pharmacoeconomic consequences of venous thromboembolism prophylaxis in major orthopaedic surgery. Pharmacoeconomics. 2003;21(7):477–96.
McCullagh L, Walsh C, Barry M. Value-of-information analysis to reduce decision uncertainty associated with the choice of thromboprophylaxis after total hip replacement in the Irish healthcare setting. Pharmacoeconomics. 2012;30(10):941–59.
Wolowacz SE, Roskell NS, Maciver F, Beard SM, Robinson PA, Plumb JM, et al. Economic evaluation of dabigatran etexilate for the prevention of venous thromboembolism after total knee and hip replacement surgery. Clin Ther. 2009;31(1):194–212.
Botteman MF, Caprini J, Stephens JM, Nadipelli V, Bell CF, Pashos CL, et al. Results of an economic model to assess the cost-effectiveness of enoxaparin, a low-molecular-weight heparin, versus warfarin for the prophylaxis of deep vein thrombosis and associated long-term complications in total hip replacement surgery in the United States. Clin Ther. 2002;24(11):1960–86 (discussion 38).
Gordois A, Posnett J, Borris L, Bossuyt P, Jonsson B, Levy E, et al. The cost-effectiveness of fondaparinux compared with enoxaparin as prophylaxis against thromboembolism following major orthopedic surgery. J Thromb Haemost. 2003;1(10):2167–74.
Lagerstedt CI, Olsson CG, Fagher BO, Oqvist BW, Albrechtsson U. Need for long-term anticoagulant treatment in symptomatic calf-vein thrombosis. Lancet. 1985;2(8454):515–8.
Moser KM, LeMoine JR. Is embolic risk conditioned by location of deep venous thrombosis? Ann Intern Med. 1981;94(4 pt 1):439–44.
Task Group of the Chinese Guidelines for Pharmacoeconomic Evaluations. China guidelines for pharmacoeconomic evaluations. China J Pharm Econ. 2011;3:7–48.
List of Chinese administrative divisions by GDP per capita. http://en.wikipedia.org/wiki/List_of_Chinese_administrative_divisions_by_GDP_per_capita. Accessed 28 Oct 2011.
Eichler HG, Kong SX, Gerth WC, Mavros P, Jonsson B. Use of cost-effectiveness analysis in health-care resource allocation decision-making: how are cost-effectiveness thresholds expected to emerge? Value Health. 2004;7(5):518–28.
Murray CJ, Evans DB, Acharya A, Baltussen RM. Development of WHO guidelines on generalized cost-effectiveness analysis. Health Econ. 2000;9(3):235–51.
Nakamura M, Miyata T, Ozeki Y, Takayama M, Komori K, Yamada N, et al. Current venous thromboembolism management and outcomes in Japan. Circ J. 2014;78(3):708–17.
Prandoni P, Villalta S, Bagatella P, Rossi L, Marchiori A, Piccioli A, et al. The clinical course of deep-vein thrombosis. Prospective long-term follow-up of 528 symptomatic patients. Haematologica. 1997;82(4):423–8.
Nakamura M, Yamada N, Ito M. Current management of venous thromboembolism in Japan: current epidemiology and advances in anticoagulant therapy. J Cardiol. 2015;66(6):451–9.
Pengo V, Lensing AW, Prins MH, Marchiori A, Davidson BL, Tiozzo F, et al. Incidence of chronic thromboembolic pulmonary hypertension after pulmonary embolism. N Engl J Med. 2004;350(22):2257–64.
Life tables for WHO member states. http://www.who.int/gho/mortality_burden_disease/life_tables/life_tables/en/. Accessed 26 July 2016.
Diamantopoulos A, Lees M, Wells PS, Forster F, Ananthapavan J, McDonald H. Cost-effectiveness of rivaroxaban versus enoxaparin for the prevention of postsurgical venous thromboembolism in Canada. Thromb Haemost. 2010;104(4):760–70.
Oster G, Tuden RL, Colditz GA. A cost-effectiveness analysis of prophylaxis against deep-vein thrombosis in major orthopedic surgery. JAMA. 1987;257(2):203–8.
Menzin J, Colditz GA, Regan MM, Richner RE, Oster G. Cost-effectiveness of enoxaparin vs low-dose warfarin in the prevention of deep-vein thrombosis after total hip replacement surgery. Arch Intern Med. 1995;155(7):757–64.
Nerurkar J, Wade WE, Martin BC. Cost/death averted with venous thromboembolism prophylaxis in patients undergoing total knee replacement or knee arthroplasty. Pharmacotherapy. 2002;22(8):990–1000.
Rubinstein I, Murray D, Hoffstein V. Fatal pulmonary emboli in hospitalized patients. An autopsy study. Arch Intern Med. 1988;148(6):1425–6.
Douketis JD, Kearon C, Bates S, Duku EK, Ginsberg JS. Risk of fatal pulmonary embolism in patients with treated venous thromboembolism. JAMA. 1998;279(6):458–62.
Stein PD, Henry JW. Prevalence of acute pulmonary embolism among patients in a general hospital and at autopsy. Chest. 1995;108(4):978–81.
Hansson PO, Sorbo J, Eriksson H. Recurrent venous thromboembolism after deep vein thrombosis: incidence and risk factors. Arch Intern Med. 2000;160(6):769–74.
Heit JA, Rooke TW, Silverstein MD, Mohr DN, Lohse CM, Petterson TM, et al. Trends in the incidence of venous stasis syndrome and venous ulcer: a 25-year population-based study. J Vasc Surg. 2001;33(5):1022–7.
Bao L, Xiaoping X, Yue G, Zhengang C. Cost-effectiveness of apixaban compared with enoxaparin for prevention of venous thromboembolism after major orthopedic surgery in China. Chin J Jt Surg (Electronic Version). 2014;8(5):677–81.
Xu H, Zhang Y, Liu L, Zou R. Warfarin dosing and pharmacoeconomic evaluation in patients after mechanical prosthesis aortic valve replacement. Acta Academiae Medicinae Jiangxi. 2009;49(12):102–5.
Zhou J, Li B. Cost-effectiveness analysis of endoscope and omprazole in the treatment of acute hemorrhage of upper digestive tract. Lingnan J Emerg Med. 2013;18(6):453–6.
Xingbao C, Eggington S, Caiyun W, Min ZHU. Cost-effectiveness study of rivaroxaban for the prevention of venous thromboembolism in patients under going total knee replacement. China Pharm. 2011;22(30):2787–90.
Hogg K, Kimpton M, Carrier M, Coyle D, Forgie M, Wells P. Estimating quality of life in acute venous thrombosis. JAMA Intern Med. 2013;173(12):1067–72.
Rasanen P, Paavolainen P, Sintonen H, Koivisto AM, Blom M, Ryynanen OP, et al. Effectiveness of hip or knee replacement surgery in terms of quality-adjusted life years and costs. Acta Orthop. 2007;78(1):108–15.
Garin MC, Clark L, Chumney EC, Simpson KN, Highland KB. Cost-utility of treatments for pulmonary arterial hypertension: a Markov state-transition decision analysis model. Clin Drug Investig. 2009;29(10):635–46.
Bo H, Fu AZ. Predicting utility for joint health states: a general framework and a new nonparametric estimator. Med Decis Mak. 2010;30(5):E29–39.
Wang Y, Zheng Y, Cai S, Fang L, Ni P. Efficacy and economics analysis of two anticoagulant schemes in the treatment of inpatients with pulmonary embolism. Chin J Drug Appl Monit. 2010;7(4):200–4.
Cao S. Pharmacoeconomic analysis of four strategies for treating deep vein thrombosis. J Huaihai Med. 2009;27(4):355–6.
Shen J, Sun Y, Liu H, Yao T, Bu J, Shen L, et al. Study on the cost-effect of combined therapy for patients with pulmonary arterial hypertension. J Intern Med Concepts Pract. 2008;3(6):416–9.
Craig BA, Black MA. Incremental cost-effectiveness ratio and incremental net-health benefit: two sides of the same coin. Expert Rev Pharmacoecon Outcomes Res. 2001;1(1):37–46.
Ryttberg L, Diamantopoulos A, Forster F, Lees M, Fraschke A, Bjorholt I. Cost-effectiveness of rivaroxaban versus heparins for prevention of venous thromboembolism after total hip or knee surgery in Sweden. Expert Rev Pharmacoecon Outcomes Res. 2011;11(5):601–15.
Gomez-Outes A, Avendano-Sola C, Terleira-Fernandez AI, Vargas-Castrillon E. Pharmacoeconomic evaluation of dabigatran, rivaroxaban and apixaban versus enoxaparin for the prevention of venous thromboembolism after total hip or knee replacement in Spain. Pharmacoeconomics. 2014;32(9):919–36.
Revankar N, Patterson J, Kadambi A, Raymond V, El-Hadi W. A Canadian study of the cost-effectiveness of apixaban compared with enoxaparin for post-surgical venous thromboembolism prevention. Postgrad Med. 2013;125(4):141–53.
Lewczuk J, Piszko P, Jagas J, Porada A, Wojciak S, Sobkowicz B, et al. Prognostic factors in medically treated patients with chronic pulmonary embolism. Chest. 2001;119(3):818–23.
Urushibara T, Tanabe N, Suda R, Kato F, Kasai H, Takeuchi T, et al. Effects of surgical and medical treatment on quality of life for patients with chronic thromboembolic pulmonary hypertension. Circ J. 2015;79(12):2696–702.
Schweikert B, Pittrow D, Vizza CD, Pepke-Zaba J, Hoeper MM, Gabriel A, et al. Demographics, clinical characteristics, health resource utilization and cost of chronic thromboembolic pulmonary hypertension patients: retrospective results from six European countries. BMC Health Serv Res. 2014;14:246.
Eriksson BI, Borris LC, Friedman RJ, Haas S, Huisman MV, Kakkar AK, et al. Rivaroxaban versus enoxaparin for thromboprophylaxis after hip arthroplasty. N Engl J Med. 2008;358(26):2765–75.
Duran A, Sengupta N, Diamantopoulos A, Forster F, Kwong L, Lees M. Cost effectiveness of rivaroxaban versus enoxaparin for prevention of post-surgical venous thromboembolism from a U.S. payer’s perspective. Pharmacoeconomics. 2012;30(2):87–101.
Acknowledgments
The authors would like to thank Seng Chuen and Xingzhi Wang from IMS Health Asia Pacific for reviewing and editing the manuscript. We would like to thank the two anonymous reviewers and the editor for their very useful comments and suggestions, which helped us improve the quality of our paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by Sanofi China. However, the study sponsor had no influence on the study design, data collection, or writing of the manuscript.
Conflict of interest statement
Dr. Wu has received a consulting fee from Sanofi China. None of the remaining authors has any personal or financial conflicts of interest.
Rights and permissions
About this article
Cite this article
Yan, X., Gu, X., Zhou, L. et al. Cost Effectiveness of Apixaban and Enoxaparin for the Prevention of Venous Thromboembolism After Total Knee Replacement in China. Clin Drug Investig 36, 1001–1010 (2016). https://doi.org/10.1007/s40261-016-0444-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-016-0444-5