Abstract
Purpose
Deferiprone (DFP), deferasirox (DFX) and deferoxamine (DFO) are used in thalassaemia major (TM) patients to treat chronic iron overload. We evaluated the cost-effectiveness of DFP, compared with DFX and DFO monotherapy, from an Italian healthcare system perspective.
Methods
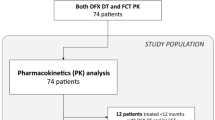
A Markov model was used over a time horizon of 5 years. Italian-specific cost data were combined with Italian efficacy data. Costs and quality-adjusted life years (QALYs) were calculated for each treatment, with cost-effectiveness expressed as cost per QALY.
Results
In all scenarios modelled, DFP was the dominant treatment strategy. Sensitivity analyses showed that DFP dominated the other treatments with a >99% likelihood of being cost-effective against DFX and DFO at a willingness to pay threshold of €20,000 per QALY.
Conclusions
DFP was the dominant and most cost-effective treatment for managing chronic iron overload in TM patients. Its use can result in substantial cost savings for the Italian healthcare system.




Similar content being viewed by others
References
Modell B, Darlison M. Global epidemiology of haemoglobin disorders and derived service indicators. Bull World Health Organ. 2008;86(6):480–7.
Galanello R, Origa R. Beta-thalassemia. Orphanet J Rare Dis. 2010;5:11.
Angelucci E, Barosi G, Camaschella C, Cappellini MD, Cazzola M, Galanello R, et al. Italian Society of Hematology practice guidelines for the management of iron overload in thalassemia major and related disorders. Haematologica. 2008;93(5):741–52.
Carbone S. Thalassemia in Messina: a sociological approach to chronic disease. Thalass Rep. 2014;4(1):2207.
Cao A, Galanello R. Beta-thalassemia. Genet Med. 2010;12(2):61–76.
Higgs DR, Engel JD, Stamatoyannopoulos G. Thalassaemia. Lancet. 2012;379(9813):373–83.
McLeod C, Fleeman N, Kirkham J, Bagust A, Boland A, Chu P, et al. Deferasirox for the treatment of iron overload associated with regular blood transfusions (transfusional haemosiderosis) in patients suffering with chronic anaemia: a systematic review and economic evaluation. Health Technol Assess. 2009;13(1):iii–iv, ix–xi, 1–121.
Borgna-Pignatti C, Rugolotto S, De Stefano P, Zhao H, Cappellini MD, Del Vecchio GC, et al. Survival and complications in patients with thalassemia major treated with transfusion and deferoxamine. Haematologica. 2004;89(10):1187–93.
Cunningham MJ, Macklin EA, Neufeld EJ, Cohen AR. Complications of beta-thalassemia major in North America. Blood. 2004;104(1):34–9.
Modell B, Khan M, Darlison M. Survival in beta-thalassaemia major in the UK: data from the UK Thalassaemia Register. Lancet. 2000;355(9220):2051–2.
Pepe A, Meloni A, Rossi G, Caruso V, Cuccia L, Spasiano A, et al. Cardiac complications and diabetes in thalassaemia major: a large historical multicentre study. Br J Haematol. 2013;163(4):520–7.
Zurlo MG, De Stefano P, Borgna-Pignatti C, Di Palma A, Piga A, Melevendi C, et al. Survival and causes of death in thalassaemia major. Lancet. 1989;2(8653):27–30.
Novartis Pharmaceuticals. Desferal SPC. http://www.medicines.org.uk/EMC/medicine/2666/SPC/Desferal+Vials%2c+500mg+or+2g/. Accessed 1 Oct 2015.
Abetz L, Baladi JF, Jones P, Rofail D. The impact of iron overload and its treatment on quality of life: results from a literature review. Health Qual Life Outcomes. 2006;4:73.
Delea TE, Edelsberg J, Sofrygin O, Thomas SK, Baladi JF, Phatak PD, et al. Consequences and costs of noncompliance with iron chelation therapy in patients with transfusion-dependent thalassemia: a literature review. Transfusion. 2007;47(10):1919–29.
Borgna-Pignatti C, Cappellini MD, De Stefano P, Del Vecchio GC, Forni GL, Gamberini MR, et al. Cardiac morbidity and mortality in deferoxamine- or deferiprone-treated patients with thalassemia major. Blood. 2006;107(9):3733–7.
Modell B, Khan M, Darlison M, Westwood MA, Ingram D, Pennell DJ. Improved survival of thalassaemia major in the UK and relation to T2* cardiovascular magnetic resonance. J Cardiovasc Magn Reson. 2008;10(1):42.
European Medicines Agency. Exjade: EPAR—product information. http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/medicines/000670/human_med_000780.jsp&mid=WC0b01ac058001d124. Accessed 1 Oct 2015.
Kirk P, Roughton M, Porter JB, Walker JM, Tanner MA, Patel J, et al. Cardiac T2* magnetic resonance for prediction of cardiac complications in thalassemia major. Circulation. 2009;120(20):1961–8.
Berdoukas V, Chouliaras G, Moraitis P, Zannikos K, Berdoussi E, Ladis V. The efficacy of iron chelator regimes in reducing cardiac and hepatic iron in patients with thalassaemia major: a clinical observational study. J Cardiovasc Magn Reson. 2009;11(1):20.
Maggio A, D’Amico G, Morabito A, Capra M, Ciaccio C, Cianciulli P, et al. Deferiprone versus deferoxamine in patients with thalassemia major: a randomized clinical trial. Blood Cells Mol Dis. 2002;28(2):196–208.
Pennell DJ, Berdoukas V, Karagiorga M, Ladis V, Piga A, Aessopos A, et al. Randomized controlled trial of deferiprone or deferoxamine in beta-thalassemia major patients with asymptomatic myocardial siderosis. Blood. 2006;107(9):3738–44.
Pepe A, Meloni A, Capra M, Cianciulli P, Prossomariti L, Malaventura C, et al. Deferasirox, deferiprone and desferrioxamine treatment in thalassemia major patients: cardiac iron and function comparison determined by quantitative magnetic resonance imaging. Haematologica. 2011;96(1):41–7.
Pennell DJ, Porter JB, Cappellini MD, El-Beshlawy A, Chan LL, Aydinok Y, et al. Efficacy of deferasirox in reducing and preventing cardiac iron overload in beta-thalassemia. Blood. 2010;115(12):2364–71.
Pepe A, Meloni A, Rossi G, Cuccia L, D’Ascola GD, Santodirocco M, et al. Cardiac and hepatic iron and ejection fraction in thalassemia major: multicentre prospective comparison of combined deferiprone and deferoxamine therapy against deferiprone or deferoxamine monotherapy. J Cardiovasc Magn Reson. 2013;15:1.
Pennell DJ, Carpenter JP, Roughton M, Cabantchik Z. On improvement in ejection fraction with iron chelation in thalassemia major and the risk of future heart failure. J Cardiovasc Magn Reson. 2011;13:45.
European Medicines Agency. Ferriprox: EPAR—product information. http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/medicines/000236/human_med_000789.jsp&mid=WC0b01ac058001d124. Accessed 1 Oct 2015.
Ceci A, Mangiarini L, Felisi M, Bartoloni F, Ciancio A, Capra M, et al. The management of iron chelation therapy: preliminary data from a national registry of thalassaemic patients. Anemia. 2011;2011:435683.
Karnon J, Tolley K, Oyee J, Jewitt K, Ossa D, Akehurst R. Cost-utility analysis of deferasirox compared to standard therapy with desferrioxamine for patients requiring iron chelation therapy in the United Kingdom. Curr Med Res Opin. 2008;24(6):1609–21.
Lai ME, Grady RW, Vacquer S, Pepe A, Carta MP, Bina P, et al. Increased survival and reversion of iron-induced cardiac disease in patients with thalassemia major receiving intensive combined chelation therapy as compared to desferoxamine alone. Blood Cells Mol Dis. 2010;45(2):136–9.
Luangasanatip N, Chaiyakunapruk N, Upakdee N, Wong P. Iron-chelating therapies in a transfusion-dependent thalassaemia population in Thailand: a cost-effectiveness study. Clin Drug Investig. 2011;31(7):493–505.
Bentley A, Gillard S, Spino M, Connelly J, Tricta F. Cost-utility analysis of deferiprone for the treatment of beta-thalassaemia patients with chronic iron overload: a UK perspective. Pharmacoeconomics. 2013;31(9):807–22.
Cataldo F. Immigration and changes in the epidemiology of hemoglobin disorders in Italy : an emerging public health burden. Italian J Pediatr. 2012;38(1):32. doi:10.1186/1824-7288-38-32.
Capri S, Ceci A, Terranova L, Merlo F, Mantovani L, TMotIG P. Guidelines for economic evaluations in Italy: recommendations from the Italian group of pharmacoeconomic studies. Drug Inform J. 2001;35:189–201.
Russo P. Pharmacoeconomic evaluations in the Italian regulatory context: a qualiquantitative analysis of pricing and reimbursement dossiers. Pharmacoecon Ital Res Artic. 2008;10:59–75.
Karnon J, Tolley K, Vieira J, Chandiwana D. Lifetime cost-utility analyses of deferasirox in beta-thalassaemia patients with chronic iron overload: a UK perspective. Clin Drug Investig. 2012;32(12):805–15.
Maggio A, Vitrano A, Capra M, Cuccia L, Gagliardotto F, Filosa A, et al. Improving survival with deferiprone treatment in patients with thalassemia major: a prospective multicenter randomised clinical trial under the auspices of the Italian society for thalassemia and hemoglobinopathies. Blood Cells Mol Dis. 2009;42(3):247–51.
Pepe A, Meloni A, Rossi G, Dell’Amico MC, Spasiano A, Capra M, et al. A T2* MRI prospective survey on heart iron in thalassemia major patients treated with deferasirox versus deferiprone and desferrioxamine in monotherapy. J Cardiovasc Magn Reson. 2011;13(1):1–2. doi:10.1186/1532-429x-13-s1-o21.
Cappellini MD, Cohen A, Piga A, Bejaoui M, Perrotta S, Agaoglu L, et al. A phase 3 study of deferasirox (ICL670), a once-daily oral iron chelator, in patients with beta-thalassemia. Blood. 2006;107(9):3455–62.
Piga A, Galanello R, Forni GL, Cappellini MD, Origa R, Zappu A, et al. Randomized phase II trial of deferasirox (Exjade, ICL670), a once-daily, orally-administered iron chelator, in comparison to deferoxamine in thalassemia patients with transfusional iron overload. Haematologica. 2006;91(7):873–80.
Tufts. Cost-effectiveness analysis registry. https://research.tufts-nemc.org/cear4/SearchingtheCEARegistry/SearchtheCEARegistry.aspx. Accessed 1 April 2015.
Pepe A, Meloni A, Rossi G, Carollo A, Santamaria V, Scaccetti A, et al. Direct cost analysis about the three chelators for the treatment of thalassemia patients with chronic iron overload: an Italian perspective from the MIOT network. Blood. 2013;122(21):5605.
Scalone L, Mantovani LG, Krol M, Rofail D, Ravera S, Bisconte MG, et al. Costs, quality of life, treatment satisfaction and compliance in patients with beta-thalassemia major undergoing iron chelation therapy: the ITHACA study. Curr Med Res Opin. 2008;24(7):1905–17.
Young KE, Urbinati D, Toumi M. HTA, approach in Italy. Structure, methods, and process of veneto region’s evaluation of pharmaceutical effectiveness unit (Unità Di Valutazione Dell’efficacia Del Farmaco, Uvef). Value Health. 2014;17(7):A442–3.
Briggs AH. Handling uncertainty in cost-effectiveness models. Pharmacoeconomics. 2000;17(5):479–500.
Briggs AH, Goeree R, Blackhouse G, O’Brien BJ. Probabilistic analysis of cost-effectiveness models: choosing between treatment strategies for gastroesophageal reflux disease. Med Decis Making. 2002;22(4):290–308.
Xia S, Zhang W, Huang L, Jiang H. Comparative efficacy and safety of deferoxamine, deferiprone and deferasirox on severe thalassemia: a meta-analysis of 16 randomized controlled trials. PLoS One. 2013;8(12):e82662.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This manuscript was partially supported by Apopharma Inc. who provided financial support to Decision Resources Group Abacus for economic analysis and writing assistance.
Conflict of interest
Alessia Pepe is the PI of the MIOT project, which received “no profit support” from Chiesi Farmaceutici S.p.A. and ApoPharma Inc. Anthony Bentley and Aishah Hanif were employed by a consultancy (Decision Resources Group) that was commissioned by Apopharma Inc. to prepare cost utility analysis and manuscript. All other authors have no conflicts of interest to declare.
Ethical statement
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Pepe, A., Rossi, G., Bentley, A. et al. Cost-Utility Analysis of Three Iron Chelators Used in Monotherapy for the Treatment of Chronic Iron Overload in β-Thalassaemia Major Patients: An Italian Perspective. Clin Drug Investig 37, 453–464 (2017). https://doi.org/10.1007/s40261-017-0496-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40261-017-0496-1