Abstract
Background and objective
Optimisation of hydrocortisone replacement therapy in children is challenging as there is currently no licensed formulation and dose in Europe for children under 6 years of age. In addition, hydrocortisone has non-linear pharmacokinetics caused by saturable plasma protein binding. A paediatric hydrocortisone formulation, Infacort® oral hydrocortisone granules with taste masking, has therefore been developed. The objective of this study was to establish a population pharmacokinetic model based on studies in healthy adult volunteers to predict hydrocortisone exposure in paediatric patients with adrenal insufficiency.
Methods
Cortisol and binding protein concentrations were evaluated in the absence and presence of dexamethasone in healthy volunteers (n = 30). Dexamethasone was used to suppress endogenous cortisol concentrations prior to and after single doses of 0.5, 2, 5 and 10 mg of Infacort® or 20 mg of Infacort®/hydrocortisone tablet/hydrocortisone intravenously. A plasma protein binding model was established using unbound and total cortisol concentrations, and sequentially integrated into the pharmacokinetic model.
Results
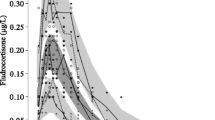
Both specific (non-linear) and non-specific (linear) protein binding were included in the cortisol binding model. A two-compartment disposition model with saturable absorption and constant endogenous cortisol baseline (Baseline cort,15.5 nmol/L) described the data accurately. The predicted cortisol exposure for a given dose varied considerably within a small body weight range in individuals weighing <20 kg.
Conclusions
Our semi-mechanistic population pharmacokinetic model for hydrocortisone captures the complex pharmacokinetics of hydrocortisone in a simplified but comprehensive framework. The predicted cortisol exposure indicated the importance of defining an accurate hydrocortisone dose to mimic physiological concentrations for neonates and infants weighing <20 kg.
EudraCT number: 2013-000260-28, 2013-000259-42.







Similar content being viewed by others
References
Bornstein SR, Allolio B, Arlt W, Barthel A, Don-Wauchope A, Hammer GD, et al. Diagnosis and treatment of primary adrenal insufficiency: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2016;101:364–89.
Porter J, Blair J, Ross RJ. Is physiological glucocorticoid replacement important in children? Arch Dis Child. 2017;102:199–205.
Toothaker RD, Sundaresan GM, Hunt JP, Goehl TJ, Rotenberg KS, Prasad VK, et al. Oral hydrocortisone pharmacokinetics: a comparison of fluorescence and ultraviolet high-pressure liquid. J Pharm Sci. 1982;71:573–6.
Derendorf H, Mollmann H, Barth J, Mollmann C, Tunn S, Krieg M. Pharmacokinetics and oral bioavailability of hydrocortisone. J Clin Pharm. 1991;31:473–6.
Speiser PW, Azziz R, Baskin LS, Ghizzoni L, Hensle TW, Merke DP, et al. Congenital adrenal hyperplasia due to steroid 21-hydroxylase deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2010;95:4133–60.
Whitaker MJ, Spielmann S, Digweed D, Huatan H, Eckland D, Johnson TN, et al. Development and testing in healthy adults of oral hydrocortisone granules with taste masking for the treatment of neonates and infants with adrenal insufficiency. J Clin Endocrinol Metab. 2015;100:1681–8.
Kauzor D, Spielmann S, Brosig H, Ross R, Blankenstein O, Kloft C. Medication safety study investigating hydrocortisone individually and extemporaneously compounded capsules for paediatric use in CAH [abstract no. P825]. 16th European Congress of Endocrinology, 2014. http://www.endocrine-abstracts.org/ea/0035/ea0035P825.htm. Accessed 25 Jun 2017.
Merke DP, Cho D, Calis KA, Keil MF, Chrousos GP. Hydrocortisone suspension and hydrocortisone tablets are not bioequivalent in the treatment of children with congenital adrenal hyperplasia. J Clin Endocrinol Metab. 2001;86:441–5.
Toothaker RD, Welling PG. Effect of dose size on the pharmacokinetics of intravenous hydrocortisone during endogenous hydrocortisone suppression. J Pharmacokinet Biopharm. 1982;10:147–56.
Lentjes EGWM. Romijn FHTPM. Temperature-dependent cortisol distribution among the blood compartments in man. J Clin Endocrinol Metab. 1999;84:682–7.
Toothaker RD, Craig WA, Welling PG. Effect of dose size on the pharmacokinetics of oral hydrocortisone suspension. J Pharm Sci. 1982;71:1182–5.
Mah PM, Jenkins RC, Rostami-Hodjegan A, Newell-Price J, Doane A, Ibbotson V, et al. Weight-related dosing, timing and monitoring hydrocortisone replacement therapy in patients with adrenal insufficiency. Clin Endocrinol. 2004;61:367–75.
Simon N, Castinetti F, Ouliac F, Lesavre N, Brue T, Oliver C. Pharmacokinetic evidence for suboptimal treatment of adrenal insufficiency with currently available hydrocortisone tablets. Clin Pharmacokinet. 2010;49:455–63.
Hoshiro M, Ohno Y, Masaki H, Iwase H, Aoki N. Comprehensive study of urinary cortisol metabolites in hyperthyroid and hypothyroid patients. Clin Endocrinol. 2006;64:37–45.
Debono M, Harrison RF, Whitaker MJ, Eckland D, Arlt W, Keevil BG, et al. Salivary cortisone reflects cortisol exposure under physiological conditions and after hydrocortisone. J Clin Endocrinol Metab. 2016;101:1469–77.
World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310:2191–4.
Association of the British Pharmaceutical Industry. Guidelines for phase 1 clinical trials (2012 edition). http://www.abpi.org.uk/our-work/library/guidelines/Pages/phase-1-trials-2012.aspx. Accessed 18 Nov 2016.
International Council for Harmonisation of Technical Requirements for Human Use. Guideline for good clinical practice E6(R1). http://www.ich.org/products/guidelines/efficacy/efficacy-single/article/good-clinical-practice.html. Accessed 18 Nov 2016.
Lewis JG, Lewis MG, Elder PA. An enzyme-linked immunosorbent assay for corticosteroid-binding globulin using monoclonal and polyclonal antibodies: decline in CBG following synthetic ACTH. Clin Chim Acta. 2003;328:121–8.
Beal S, Sheiner LB, Boeckmann A, Bauer RJ. NONMEM user’s guides (1989–2009). Ellicott City: Icon Development Solutions; 2009.
Lindbom L, Pihlgren P, Jonsson EN, Jonsson N. PsN-Toolkit–a collection of computer intensive statistical methods for non-linear mixed effect modeling using NONMEM. Comput Methods Programs Biomed. 2005;79:241–57.
Dansirikul C, Silber HE, Karlsson MO. Approaches to handling pharmacodynamic baseline responses. J Pharmacokinet Pharmacodyn. 2008;35:269–83.
Keizer R, Pastoor D, Savic R. New open source R libraries for simulation and visualization: “PKPDsim” and “vpc” 2015. http://www.page-meeting.eu/pdf_assets/1215-Page_Keizer_2015_pkpdsim_vpc.pdf. Accessed 5 Oct 2016.
R Development Core Team. R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2016. ISBN 3-900051-07-0. http://www.R-project.org. Accessed 15 June 2016.
Knutsson U, Dahlgren J, Marcus C, Rosberg S, Brönnegård M, Stierna P, et al. Circadian cortisol rhythms in healthy boys and girls: relationship with age, growth, body composition, and pubertal development. J Clin Endocrinol Metab. 1997;82:536–40.
Rohatgi A. WebPlotDigitizer. http://arohatgi.info/WebPlotDigitizer. Accessed 5 Oct 2016.
Wright DH, Stone JA, Crumley TM, Wenning L, Zheng W, Yan K, et al. Pharmacokinetic-pharmacodynamic studies of the 11β-hydroxysteroid dehydrogenase type 1 inhibitor MK-0916 in healthy subjects. Br J Clin Pharmacol. 2013;76:917–31.
Picard-Hagen N, Gayrard V, Alvinerie M, Smeyers H, Ricou R, Bousquet-Melou A, et al. A nonlabeled method to evaluate cortisol production rate by modeling plasma CBG-free cortisol disposition. Am J Physiol Endocrinol Metab. 2001;281:E946–56.
Charmandari E, Johnston A, Brook CG, Hindmarsh PC. Bioavailability of oral hydrocortisone in patients with congenital adrenal hyperplasia due to 21-hydroxylase deficiency. J Endocrinol. 2001;169:65–70.
Lennernäs H, Skrtic S, Johannsson G. Replacement therapy of oral hydrocortisone in adrenal insufficiency: the influence of gastrointestinal factors. Expert Opin Drug Metab Toxicol. 2008;4:749–58.
Westphal U. Steroid-protein interactions. In: Gross F, Labhart A, Mann T, Samuels L (eds.) 1st edn. New York: Springer; 1971.
Westphal U. Steroid-protein interactions XIII. Concentrations and binding affinities of corticosteroid-binding globulins in sera of man, monkey, rat, rabbit and guinea pig. Arch Biochem Biophys. 1967;118:556–67.
Coolens J-L, Baelen HVAN, Heyns W. Clinical use of unbound plasma cortisol as calculated from total cortisol and corticosteroid-binding globulin. J Steroid Biochem. 1987;26:197–202.
Lewis JG, Möpert B, Shand BI, Doogue MP, Soule SG, Frampton CM, et al. Plasma variation of corticosteroid-binding globulin and sex hormone-binding globulin. Horm Metab Res. 2006;38:241–5.
Chung TT, Gunganah K, Monson JP, Drake WM. Circadian variation in serum cortisol during hydrocortisone replacement is not attributable to changes in cortisol-binding globulin concentrations. Clin Endocrinol. 2016;84:496–500.
Benet LZ, Hoener B. Changes in plasma protein binding have little clinical relevance. Clin Pharmacol Ther. 2002;71:115–21.
Hadjian AJ, Chedin M, Cochet C, Chambaz EM. Cortisol binding to proteins in plasma in the human neonate and infant. Pediatr Res. 1975;9:40–5.
Rogers SL, Hughes BA, Jones CA, Freedman L, Smart K, Taylor N, et al. Diminished 11β-hydroxysteroid dehydrogenase type 2 activity is associated with decreased weight and weight gain across the first year of life. J Clin Endocrinol Metab. 2014;99:E821–31.
World Health Organisation. WHO child growth standards. 2006. http://www.who.int/childgrowth/standards/Technical_report.pdf. Accessed 19 Apr 2017.
Acknowledgements
The authors would like to thank the high-performance computing service of ZEDAT, Freie Universitaet Berlin, for computing time. In addition, the authors would like to thank Trevor Johnson and Dena Digweed for valuable support. Parts of the results were presented as a poster at the 2016 Population Approach Group Europe (PAGE) meeting.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The work was carried out under a Cooperation Agreement between Freie Universitaet and Diurnal funded by the European Commission FP7 Grant (No. 281654 TAIN).
Conflict of interest
Johanna Melin, Zinnia P. Parra Guillen and Niklas Hartung have no conflicts of interest. Richard Ross is a director of Diurnal Ltd and has stock options. Martin Whitaker is an employee and director of Diurnal Ltd and has stock options. Charlotte Kloft reports a research grant to Freie Universitaet Berlin from Diurnal funded by the European Commission FP7 Grant (No. 281654 TAIN) and grants from the Innovative Medicines Initiative-Joint Undertaking (‘DDMoRe’). Charlotte Kloft and Wilhelm Huisinga report grants from an industry consortium (AbbVie Deutschland GmbH & Co. KG, Boehringer Ingelheim Pharma GmbH & Co. KG, Grünenthal GmbH, F. Hoffmann-La Roche Ltd, Merck KGaA and SANOFI).
Ethical approval
Data from two studies (Registered EudraCT numbers: 2013-000260-28 and 2013-000259-42) were used for this analysis. Both studies were approved by the South East Wales Research Ethics committee and performed according to the 1964 Helsinki Declaration and International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use (ICH) guidelines.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Melin, J., Parra-Guillen, Z.P., Hartung, N. et al. Predicting Cortisol Exposure from Paediatric Hydrocortisone Formulation Using a Semi-Mechanistic Pharmacokinetic Model Established in Healthy Adults. Clin Pharmacokinet 57, 515–527 (2018). https://doi.org/10.1007/s40262-017-0575-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-017-0575-8