Abstract
Background
Certain broad medication classes have previously been associated with high rates of hospitalisation due to related adverse events in elderly Western Australians, based on clinical coding recorded on inpatient summaries. Similarly, some medications from the Beers Criteria, considered potentially inappropriate in older people, have been linked with an increased risk of unplanned hospitalisation in this population.
Objective
Our objective was to determine whether risk estimates of drug-related hospitalisations are altered in elderly patients taking ‘high-risk drugs’ (HRDs) when specific Beers potentially inappropriate medications (PIMS) are taken into consideration.
Methods
Using the pharmaceutical claims of 251,305 Western Australians aged ≥65 years (1993–2005) linked with other health data, we applied a case-time-control design to estimate odds ratios (ORs) for unplanned hospitalisations associated with anticoagulants, antirheumatics, opioids, corticosteroids and four major cardiovascular drug groups, from which attributable fractions (AFs), number and proportion of drug-related admissions were derived. The analysis was repeated, taking into account exposure to eight specific PIMs, and results were compared.
Results
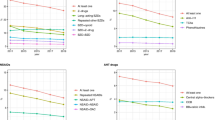
A total of 1,899,699 index hospitalisations were involved. Of index subjects, 12–57 % were exposed to each HRD at the time of admission, although the proportions taking both an HRD and one of the selected PIMs were much lower (generally ≤2 %, but as high as 8 % for combinations involving temazepam and for most PIMs combined with hypertension drugs). Included PIMs (indomethacin, naproxen, temazepam, oxazepam, diazepam, digoxin, amiodarone and ferrous sulphate) all tended to increase ORs, AFs and drug-related hospitalisation estimates in HRD combinations, although this was less evident for opioids and corticosteroids. Indomethacin had the greatest overall impact on HRD ORs/AFs. Indomethacin (OR 1.40; 95 % confidence interval [CI] 1.27–1.54) and naproxen (OR 1.22; 1.14–1.31) were associated with higher risks of unplanned hospitalisation than other antirheumatics (overall OR 1.09; 1.06–1.12). Similarly, among cardiac rhythm regulators, amiodarone (OR 1.22; 1.13–1.32) was riskier than digoxin (OR 1.08; 1.04–1.13). For comparisons of drug-related hospitalisation estimates, temazepam yielded the greatest absolute increases, especially with hypertension drugs.
Conclusions
Indomethacin and temazepam should be prescribed cautiously in elderly patients, especially in drug combinations. Furthermore, it appears other antirheumatics should be favoured over indomethacin/naproxen and, in situations where both drugs may be appropriate, digoxin over amiodarone. Our methodology may help assess the safety of new medications in drug combinations in preliminary pharmacovigilance investigations.




Similar content being viewed by others
References
Tangiisuran B, Gozzoli MP, Davies JG, Rajkumar C. Adverse drug reactions in older people. Rev Clin Gerontol. 2010;20(3):246–59.
Beijer HJM, De Blaey CJ. Hospitalisations caused by adverse drug reactions (ADR): a meta-analysis of observational studies. Pharm World Sci. 2002;24(2):46–54.
Boparai MK, Korc-Grodzicki B. Prescribing for older adults. Mt Sinai J Med. 2011;78(4):613–26. doi:10.1002/msj.20278.
Wynne HA, Blagburn J. Drug treatment in an ageing population: practical implications. Maturitas. 2010;66(3):246–50. doi:10.1016/j.maturitas.2010.03.004.
Shi S, Morike K, Klotz U. The clinical implications of ageing for rational drug therapy. Eur J Clin Pharmacol. 2008;64(2):183–99. doi:10.1007/s00228-007-0422-1.
Milton JC, Hill-Smith I, Jackson SHD. Prescribing for older people. Br Med J. 2008;336(7644):606–9. doi:10.1136/bmj.39503.424653.80.
Maio V. The quality of prescribing for the elderly: a forgotten issue? Am J Med Qual. 2005;20(4):177–8. doi:10.1177/1062860605276679.
Petrovic M, der Cammen Tv, Onder G. Adverse drug reactions in older people: detection and prevention. Drugs Aging. 2012;29(6):453–62.
Salvi F, Marchetti A, D’Angelo F, Boemi M, Lattanzio F, Cherubini A. Adverse drug events as a cause of hospitalization in older adults. Drug Saf. 2012;35(Suppl 1):29–45. doi:10.1007/BF03319101.
Budnitz DS, Lovegrove MC, Shehab N, Richards CL. Emergency hospitalizations for adverse drug events in older Americans. N Engl J Med. 2011;365(21):2002–12.
Runciman WB, Roughead EE, Semple SJ, Adams RJ. Adverse drug events and medication errors in Australia. Int J Qual Health Care. 2003;15(Supplement 1):i49–59.
Laroche ML, Charmes JP, Bouthier F, Merle L. Inappropriate medications in the elderly. Clin Pharmacol Ther. 2009;85(1):94–7. doi:10.1038/clpt.2008.214.
Levy HB, Marcus EL, Christen C. Beyond the Beers Criteria: a comparative overview of explicit criteria. Ann Pharmacother. 2010;44(12):1968–75. doi:10.1345/aph.1P426.
Chang CB, Chan DC. Comparison of published explicit criteria for potentially inappropriate medications in older adults. Drugs Aging. 2010;27(12):947–57.
Dimitrow MS, Airaksinen MSA, Kivela S-L, Lyles A, Leikola SNS. Comparison of prescribing criteria to evaluate the appropriateness of drug treatment in individuals aged 65 and older: a systematic review. J Am Geriatr Soc. 2011;59(8):1521–30. doi:10.1111/j.1532-5415.2011.03497.x.
Beers MH, Ouslander JG, Rollingher I, Reuben DB, Brooks J, Beck JC. Explicit criteria for determining inappropriate medication use in nursing-home residents. Arch Intern Med. 1991;151(9):1825–32.
Beers MH. Explicit criteria for determining potentially inappropriate medication use by the elderly—an update. Arch Intern Med. 1997;157(14):1531–6.
Fick DM, Cooper JW, Wade WE, Waller JL, Maclean JR, Beers MH. Updating the Beers Criteria for potentially inappropriate medication use in older adults—results of a US consensus panel of experts. Arch Intern Med. 2003;163(22):2716–24.
The American Geriatrics Society 2012 Beers Criteria Update Expert Panel. American Geriatrics Society updated Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2012;60(4):616–31. doi:10.1111/j.1532-5415.2012.03923.x.
Gallagher P, Barry P, O’Mahony D. Inappropriate prescribing in the elderly. J Clin Pharm Ther. 2007;32(2):113–21.
Wawruch M, Fialova D, Zikavska M, Wsolova L, Jezova D, Kuzelova M, et al. Factors influencing the use of potentially inappropriate medication in older patients in Slovakia. J Clin Pharm Ther. 2008;33(4):381–92.
Roughead EE, Gilbert AL, Primrose JG, Sansom LN. Coding drug-related admissions in medical records: is it adequate for monitoring the quality of medication use. Aust J Hosp Pharm. 1998;28(1):7–12.
Hodgkinson MR, Dirnbauer NJ, Larmour I. Identification of adverse drug reactions using the ICD-10 Australian Modification clinical coding surveillance. J Pharm Pract Res. 2009;39(1):19–23.
Dawes VP. Poisoning in Western Australia: overview, and investigation of therapeutic poisoning in the elderly [MPH Thesis]. Nedlands: The University of Western Australia; 1994.
Burgess CL, Holman CDJ, Satti AG. Adverse drug reactions in older Australians, 1981–2002. Med J Aust. 2005;182(6):267–70.
Zhang M, Holman CDJ, Preen DB, Brameld K. Repeat adverse drug reactions causing hospitalization in older Australians: a population-based longitudinal study 1980–2003. Br J Clin Pharmacol. 2007;63(2):163–70.
Price SD, Holman CDJ, Sanfilippo FM, Emery JD. Use of case-time-control design in pharmacovigilance applications: exploration with high-risk medications and unplanned hospital admissions in the Western Australian elderly. Pharmacoepidemiol Drug Saf. 2013;22(11):1159–70. doi:10.1002/pds.3469.
Price SD, Holman CD, Sanfilippo FM, Emery JD. Association between potentially inappropriate medications from the Beers Criteria and the risk of unplanned hospitalization in elderly patients. Ann Pharmacother. 2014;48(1):6–16. doi: 10.1177/1060028013504904.
Suissa S. The case-time-control design. Epidemiology. 1995;6(3):248–53.
Suissa S. The case-time-control design: further assumptions and conditions. Epidemiology. 1998;9(4):441–5.
Duckett SJ. Drug policy down under: Australia’s Pharmaceutical Benefits Scheme. Health Care Financ Rev. 2004;25(3):55–67.
Lopert R. Evidence-based decision-making within Australia’s Pharmaceutical Benefits Scheme. Issue Brief (Commonwealth Fund). 2009;60:1–13.
Harris MG, Harris RD. The Australian health system: continuity and change. J Health Hum Serv Adm. 1998;20(1):442–67.
Department of Health and Ageing. Medicare Benefits Schedule book. Canberra: Australian Government; 2008.
Australian Institute of Health and Welfare. Residential aged care in Australia 2007–08: a statistical overview. Aged care statistic series 28. Cat. no. AGE 58. Canberra: AIHW; 2009. p. 138–41.
Holman CDJ, Bass AJ, Rouse IL, Hobbs MS. Population-based linkage of health records in Western Australia: development of a health services research linked database. Aust N Z J Publ Health. 1999;23(5):453–9.
Holman CDJ, Bass AJ, Rosman DL, Smith MB, Semmens JB, Glasson EJ, et al. A decade of data linkage in Western Australia: strategic design, applications and benefits of the WA data linkage system. Aust Health Rev. 2008;32(4):766–77.
Australian Bureau of Statistics. Australian historical population statistics—population age-sex structure: population, age and sex, WA, 30 June, 1901 onwards. ABS cat. no. 4105.0.65.001. ABS, Canberra. 2008. http://www.abs.gov.au/AUSSTATS/abs@.nsf/DetailsPage/3105.0.65.0012008?OpenDocument. Accessed Jun 15 2012.
Department of Health and Ageing. Schedule of pharmaceutical benefits for approved pharmacists and medical practitioners. Canberra: Australian Government; 1991–2007.
WHO Collaborating Centre for Drug Statistics Methodology. Guidelines for ATC classification and DDD assignment 2007. Oslo, 2006.
WHO Collaborating Centre for Drug Statistics Methodology. ATC classification index with DDDs 2007. Oslo, 2006.
Britt H, Miller G, Charles J, Henderson J, Bayram C, Pan Y, et al. General practice activity in Australia 2009–10. General practice series no. 27. Cat. no. GEP 27. Canberra: Australian Institute of Health and Welfare; 2010.
Britt H, Miller G, Charles J, Henderson J, Bayram C, Valenti L, et al. General practice activity in Australia 2000-01 to 2009-10: 10 year data tables. General practice series no. 28. Cat. no. GEP 28. Canberra: Australian Institute of Health and Welfare; 2010.
Britt H, Miller G, Bayram C. The quality of data on general practice—a discussion of BEACH reliability and validity. Aust Fam Physician. 2007;36(1–2):36–40.
MIMS Australia. June 2000 MIMS annual. St Leonards: MIMS Australia; 2000.
MIMS Australia. June 2005 MIMS annual. St Leonards: MIMS Australia; 2005.
MIMS Australia. MIMS online. MIMS Australia: St Leonards; 2008. https://www.mimsonline.com.au/Search/Search.aspx. Accessed 2008.
WHO Collaborating Centre for Drug Statistics Methodology. Guidelines for ATC classification and DDD assignment 2008. Oslo, 2007.
WHO Collaborating Centre for Drug Statistics Methodology. ATC classification index with DDDs 2008. Oslo, 2007.
Greenblatt DJ. Elimination half-life of drugs: value and limitations. Annu Rev Med. 1985;36:421–7.
Birkett DJ. Pharmacokinetics made easy 3: half-life. Aust Prescriber. 1988;11(3):57–9.
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi J-C, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–9.
SAS Institute Inc. SAS 9.2 for Windows. Cary: SAS Institute Inc; 2002–2009.
Lin DY, Wei LJ. The robust inference for the Cox proportional hazards model. J Am Stat Assoc. 1989;84(408):1074–8.
Greenland S, Robins JM. Conceptual problems in the definition and interpretation of attributable fractions. Am J Epidemiol. 1988;128(6):1185–97.
Greenland S. Applications of stratified analysis methods. In: Rothman KJ, Greenland S, Lash TL, editors. Modern epidemiology. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2008. p. 283–302.
Greenland S, Rothman KJ, Lash TL. Measures of effect and measures of association. In: Rothman KJ, Greenland S, Lash TL, editors. Modern epidemiology. 3rd ed. Philadelphia: Lippincott Williams & Wilkins; 2008. p. 51–70.
English DR, Holman CDJ, Milne E, Winter MG, Hulse GK, Codde JP, et al. The quantification of drug caused morbidity and mortality in Australia 1995—part 1. Canberra: Commonwealth Department of Human Services and Health; 1995. p. 6–19.
Leone R, Magro L, Moretti U, Cutroneo P, Moschini M, Motola D, et al. Identifying adverse drug reactions associated with drug–drug interactions: data mining of a spontaneous reporting database in Italy. Drug Saf. 2010;33(8):667–75. doi:10.2165/11534400-000000000-00000.
Pasina L, Djade CD, Nobili A, Tettamanti M, Franchi C, Salerno F, et al. Drug-drug interactions in a cohort of hospitalized elderly patients. Pharmacoepidemiol Drug Saf. 2013;22(10):1054–60.
Moura CS, Prado NM, Belo NO, Acurcio FA. Evaluation of drug-drug interaction screening software combined with pharmacist intervention. Int J Clin Pharm. 2012;34(4):547–52.
Vitry AI. Comparative assessment of four drug interaction compendia. Br J Clin Pharmacol. 2007;63(6):709–14.
Malone DC, Hutchins DS, Haupert H, Hansten P, Duncan B, Van Bergen RC, et al. Assessment of potential drug-drug interactions with a prescription claims database. Am J Health Syst Pharm. 2005;62(19):1983–91.
Roughead EE, Kalisch LM, Barratt JD, Gilbert AL. Prevalence of potentially hazardous drug interactions amongst Australian veterans. Br J Clin Pharmacol. 2010;70(2):252–7. doi:10.1111/j.1365-2125.2010.03694.x.
Mahmood M, Malone DC, Skrepnek GH, Abarca J, Armstrong EP, Murphy JE, et al. Potential drug–drug interactions within Veterans Affairs medical centers. Am J Health Syst Pharm. 2007;64(14):1500–5.
Moura C, Prado N, Acurcio F. Potential drug–drug interactions associated with prolonged stays in the intensive care unit: a retrospective cohort study. Clin Drug Invest. 2011;31(5):309–16.
Johnell K, Klarin I. The relationship between number of drugs and potential drug–drug interactions in the elderly: a study of over 600 000 elderly patients from the Swedish prescribed drug register. Drug Saf. 2007;30(10):911–8.
Nobili AM, Pasina LPD, Tettamanti MM, Lucca UM, Riva EMDP, Marzona IPD, et al. Potentially severe drug interactions in elderly outpatients: results of an observational study of an administrative prescription database. J Clin Pharm Ther. 2009;34(4):377–86.
Secoli S-R, Figueras A, Lebrao ML, de Lima FD, Santos JLF. Risk of potential drug–drug interactions among Brazilian elderly: a population-based, cross-sectional study. Drugs Aging. 2010;27(9):759–70.
Obreli-Neto PR, Nobili A, de Oliveira Baldoni A, Guidoni CM, de Lyra Junior DP, Pilger D et al. Adverse drug reactions caused by drug-drug interactions in elderly outpatients: a prospective cohort study. Eur J Clin Pharmacol. 2012;68(12):1667–76. doi:10.1007/s00228-012-1309-3.
Fokter N, Mozina M, Brvar M. Potential drug-drug interactions and admissions due to drug–drug interactions in patients treated in medical departments. Wien Klin Wochenschr. 2010;122(3–4):81–8.
Bucsa C, Farcas A, Cazacu I, Leucuta D, Achimas-Cadariu A, Mogosan C, et al. How many potential drug-drug interactions cause adverse drug reactions in hospitalized patients? Eur J Intern Med. 2013;24(1):27–33.
Tulner LR, Frankfort SV, Gijsen GJPT, van Campen JPCM, Koks CHW, Beijnen JH. Drug–drug interactions in a geriatric outpatient cohort: prevalence and relevance. Drugs Aging. 2008;25(4):343–55.
Wright A, Feblowitz J, Phansalkar S, Liu J, Wilcox A, Keohane CA, et al. Preventability of adverse drug events involving multiple drugs using publicly available clinical decision support tools. Am J Health Syst Pharm. 2012;69(3):221–7.
Schafer AI. Effects of nonsteroidal antiinflammatory drugs on platelet function and systemic hemostasis. J Clin Pharmacol. 1995;35(3):209–19. doi:10.1002/j.1552-4604.1995.tb04050.x.
Hines LEP, Murphy JEP. Potentially harmful drug–drug interactions in the elderly: a review. Am J Geriatr Pharmacother. 2011;9(6):364–77.
Park KE, Qin Y, Bavry AA. Nonsteroidal anti-inflammatory drugs and their effects in the elderly. Aging Health. 2012;8(2):167–77.
Biederman RE. Pharmacology in rehabilitation: nonsteroidal anti-inflammatory agents. J Orthop Sports Phys Ther. 2005;35(6):356–67.
Arnstein P. Balancing analgesic efficacy with safety concerns in the older patient. Pain Manag Nurs. 2010;11(2) Sup(1):S11–22.
Cooney D, Pascuzzi K. Polypharmacy in the elderly: focus on drug interactions and adherence in hypertension. Clin Geriatr Med. 2009;25(2):221–33. doi:10.1016/j.cger.2009.01.005.
Bauman JL, DiDomenico RJ, Galanter WL. Mechanisms, manifestations, and management of digoxin toxicity in the modern era. Am J Cardiovasc Drugs. 2006;6(2):77–86.
Jelinek HF, Warner P. Digoxin therapy in the elderly: pharmacokinetic considerations in nursing. Geriatr Nurs. 2011;32(4):269.
Feely J, Barry M. Adverse drug interactions. Clin Med. 2005;5(1):19–22.
Zetin M. Psychopharmacohazardology: major hazards of the new generation of psychotherapeutic drugs. Int J Clin Pract. 2004;58(1):58–68.
Wang PS, Bohn RL, Glynn RJ, Mogun H, Avorn J. Hazardous benzodiazepine regimens in the elderly: effects of half-life, dosage, and duration on risk of hip fracture. Am J Psychiatry. 2001;158(6):892–8.
Pariente A, Dartigues J-F, Benichou J, Letenneur L, Moore N, Fourrier-Reglat A. Benzodiazepines and injurious falls in community dwelling elders. Drugs Aging. 2008;25(1):61–70.
French DD, Chirikos TN, Spehar A, Campbell R, Means H, Bulat T. Effect of concomitant use of benzodiazepines and other drugs on the risk of injury in a veterans population. Drug Saf. 2005;28(12):1141–50.
Delgado-Rodriguez M, Llorca J. Bias. J Epidemiol Community Health. 2004;58:635–41.
Department of Health and Ageing. Australian statistics on medicines 2004–05. Canberra: Australian Government; 2007.
Greenland S. Confounding and exposure trends in case crossover and case time-control designs. Epidemiology. 1996;7(3):231–9.
Department of Health and Ageing. Schedule of pharmaceutical benefits (effective 1 August 2012–31 August 2012). Canberra: Australian Government; 2012.
Marcum ZA, Hanlon JT. Commentary on the new American Geriatric Society Beers Criteria for potentially inappropriate medication use in older adults. Am J Geriatr Pharmacother. 2012;10(2):151–9. doi:10.1016/j.amjopharm.2012.03.002.
Acknowledgments
This study was funded by an Australian National Health and Medical Research Council (NHMRC) project grant. The funding body was not involved in any aspect of the study other than assessment of the project proposal for funding purposes via an independent peer review process.
We are grateful to the Department of Health of Western Australia (DoHWA) and the Australian Department of Health and Ageing for supplying the project data. We particularly thank the Data Linkage Branch (DoHWA) for undertaking the record linkage.
The authors have no conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Price, S.D., Holman, C.D.J., Sanfilippo, F.M. et al. Impact of Specific Beers Criteria Medications on Associations between Drug Exposure and Unplanned Hospitalisation in Elderly Patients Taking High-Risk Drugs: A Case-Time-Control Study in Western Australia. Drugs Aging 31, 311–325 (2014). https://doi.org/10.1007/s40266-014-0164-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-014-0164-6