Abstract
Background
Falls are a leading cause of preventable hospitalizations from long-term care facilities (LTCFs). Polypharmacy and falls-risk medications are potentially modifiable risk factors for falling.
Objective
This study investigated whether polypharmacy and falls-risk medications are associated with fall-related hospital admissions from LTCFs compared with hospital admissions for other causes.
Methods
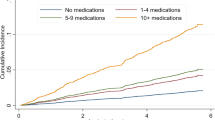
This was a hospital-based, case–control study of patients aged ≥65 years hospitalized from LTCFs. Cases were patients with falls and fall-related injuries, and controls were patients admitted for infections. Conditional logistic regression was used to calculate adjusted odds ratios (ORs) and 95% confidence intervals (CIs) for the associations between polypharmacy (defined as the use of nine or more regular pre-admission medications) and falls-risk medications (categorized as psychotropic medications and those that can cause orthostatic hypotension) with fall-related hospital admissions.
Results
There was no association between polypharmacy and fall-related hospital admissions (adjusted OR 0.97, 95% CI 0.63–1.48); however, the adjusted odds of fall-related hospital admissions increased by 16% (95% CI 3–30%) for each additional falls-risk medication. Medications that can cause orthostatic hypotension (adjusted OR 1.25, 95% CI 1.06–1.46), but not psychotropic falls-risk medications (adjusted OR 1.02, 95% CI 0.88–1.18) were associated with fall-related hospital admissions. The association between medications that can cause orthostatic hypotension and fall-related hospital admissions was strongest among residents with polypharmacy (adjusted OR 1.44, 95% CI 1.08–1.92).
Conclusion
Polypharmacy was not an independent risk factor for fall-related hospital admissions; however, medications that can cause orthostatic hypotension were associated with fall-related hospital admissions, particularly among residents with polypharmacy. Falls-risk should be considered when prescribing medications that can cause orthostatic hypotension.
Similar content being viewed by others
References
Kalisch LM, Caughey GE, Barratt JD, et al. Prevalence of preventable medication-related hospitalizations in Australia: an opportunity to reduce harm. Int J Qual Health Care. 2012;24(3):239–49.
Tovell A, Harrison JE, Pointer S. Hospitalised injury in older Australians, 2011–12. Injury research and statistics series no. 90. Cat. No. Injcat 166. Canberra: Australian Institute of Health and Welfare; 2014.
Baranzini F, Diurni M, Ceccon F, et al. Fall-related injuries in a nursing home setting: is polypharmacy a risk factor? BMC Health Serv Res. 2009;9:228.
Cherubini A, Corsonello A, Lattanzio F. Polypharmacy in nursing home residents: what is the way forward? J Am Med Dir Assoc. 2016;17(1):4–6.
Centers for Disease Control and Prevention. WISQARS. 2014. http://www.cdc.gov:8843/costT/. Accessed 24 April 2017.
Heinrich S, Rapp K, Rissmann U, et al. Cost of falls in old age: a systematic review. Osteoporos Int. 2010;21(6):891–902.
Bradley C. Trends in hospitalisations due to falls by older people, Australia 1999–00 to 2010–11. Injury research and statistics series 84. Canberra: Australian Institute of Health and Welfare; 2013.
Jokanovic N, Tan EC, Dooley MJ, et al. Prevalence and factors associated with polypharmacy in long-term care facilities: a systematic review. J Am Med Dir Assoc. 2015;16(6):535.e1–12.
Hilmer SN, Gnjidic D. The effects of polypharmacy in older adults. Clin Pharmacol Ther. 2009;85(1):86–8.
Jokanovic N, Tan EC, Dooley MJ, et al. Why is polypharmacy increasing in aged care facilities? The views of Australian health care professionals. J Eval Clin Pract. 2016;22(5):677–82.
Wastesson JW, Canudas-Romo V, Lindahl-Jacobsen R, et al. Remaining life expectancy with and without polypharmacy: a register-based study of Swedes aged 65 years and older. J Am Med Dir Assoc. 2016;17(1):31–5.
Woolcott JC, Richardson KJ, Wiens MO, et al. Meta-analysis of the impact of 9 medication classes on falls in elderly persons. Arch Intern Med. 2009;169(21):1952–60.
Runciman WB, Roughead EE, Semple SJ, et al. Adverse drug events and medication errors in Australia. Int J Qual Health Care. 2003;15(Suppl 1):i49–59.
Hartikainen S, Lonnroos E, Louhivuori K. Medication as a risk factor for falls: critical systematic review. J Gerontol A Biol Sci Med Sci. 2007;62(10):1172–81.
Olazarán J, Valle D, Serra JA, et al. Psychotropic medications and falls in nursing homes: a cross-sectional study. J Am Med Dir Assoc. 2013;14(3):213–7.
Ruxton K, Woodman RJ, Mangoni AA. Drugs with anticholinergic effects and cognitive impairment, falls and all-cause mortality in older adults: a systematic review and meta-analysis. Br J Clin Pharmacol. 2015;80(2):209–20.
Lipsitz LA, Jonsson PV, Kelley MM, et al. Causes and correlates of recurrent falls in ambulatory frail elderly. J Gerontol. 1991;46(4):M114–22.
Damián J, Pastor-Barriuso R, Valderrama-Gama E, et al. Factors associated with falls among older adults living in institutions. BMC Geriatr. 2013;13(1):1–9.
Park H, Satoh H, Miki A, et al. Medications associated with falls in older people: systematic review of publications from a recent 5-year period. Eur J Clin Pharmacol. 2015;71(12):1429–40.
Mann CJ. Observational research methods. Research design II: cohort, cross sectional, and case–control studies. Emerg Med J. 2003;20(1):54–60.
Australian Government. My aged care. 2015. http://www.myagedcare.gov.au/aged-care-homes. Accessed 24 April 2017.
Sluggett JK, Ilomaki J, Seaman KL, et al. Medication management policy, practice and research in Australian residential aged care: current and future directions. Pharmacol Res. 2017;116:20–8.
World Health Organization. International statistical classification of diseases and related health problems, 10th revision. 2004. http://apps.who.int/classifications/icd10/browse/2010/en. Accessed 24 April 2017.
Rothman KJ, Greenland S, Lash TL. Case–control studies. Encyclopedia of quantitative risk analysis and assessment. New Jersey: Wiley; 2008.
Bronskill SE, Gill SS, Paterson JM, et al. Exploring variation in rates of polypharmacy across long term care homes. J Am Med Dir Assoc. 2012;13(3):309.e15–21.
Australian Commission on Safety and Quality in Health Care. Medication reconciliation. 2017. https://www.safetyandquality.gov.au/our-work/medication-safety/medication-reconciliation. Accessed 24 April 2017.
WHO Collaborating Centre for Drug Statistics Methodology. ATC/DDD index 2016. 2015. http://www.whocc.no/atc/structure_and_principles/. Accessed 24 April 2017.
State Government of Victoria. Quality indicators in public sector residential aged care services: resource materials 2015. 2015. www.health.vic.gov.au/agedcare/publications/resourcemanual. Accessed 24 April 2017.
Milos V, Bondesson Å, Magnusson M, et al. Fall risk-increasing drugs and falls: a cross-sectional study among elderly patients in primary care. BMC Geriatr. 2014;14(1):1–7.
Groll DL, To T, Bombardier C, et al. The development of a comorbidity index with physical function as the outcome. J Clin Epidemiol. 2005;58(6):595–602.
Vu MQ, Weintraub N, Rubenstein LZ. Falls in the nursing home: are they preventable? J Am Med Dir Assoc. 2006;7(3 Suppl):S53–8.
Bavishi C, DuPont HL. Systematic review: the use of proton pump inhibitors and increased susceptibility to enteric infection. Aliment Pharmacol Ther. 2011;34(11–12):1269–81.
Eom CS, Jeon CY, Lim JW, et al. Use of acid-suppressive drugs and risk of pneumonia: a systematic review and meta-analysis. CMAJ. 2011;183(3):310–9.
Jansen S, Bhangu J, de Rooij S, et al. The association of cardiovascular disorders and falls: a systematic review. J Am Med Dir Assoc. 2016;17(3):193–9.
Benetos A, Labat C, Rossignol P, et al. Treatment with multiple blood pressure medications, achieved blood pressure, and mortality in older nursing home residents: the PARTAGE study. JAMA Intern Med. 2015;175(6):989–95.
O’Mahony D, O’Sullivan D, Byrne S, et al. STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing. 2015;44(2):213–8.
Goeres LM, Williams CD, Eckstrom E, et al. Pharmacotherapy for hypertension in older adults: a systematic review. Drugs Aging. 2014;31(12):897–910.
Pratt NL, Ramsay EN, Kalisch Ellett LM, et al. Association between use of multiple psychoactive medicines and hospitalization for falls: retrospective analysis of a large healthcare claim database. Drug Saf. 2014;37(7):529–35.
Sterke CS, van Beeck EF, van der Velde N, et al. New insights: dose–response relationship between psychotropic drugs and falls: a study in nursing home residents with dementia. J Clin Pharmacol. 2012;52(6):947–55.
Callisaya ML, Sharman JE, Close J, et al. Greater daily defined dose of antihypertensive medication increases the risk of falls in older people: a population-based study. J Am Geriatr Soc. 2014;62(8):1527–33.
Balancing benefits and harms of antipsychotic therapy. 2011. http://www.nps.org.au/publications/health-professional/nps-news/2011/balancing-benefits-harms-of-antipsychotic-therapy. Accessed 24 AprIL 2017.
Unit for Medication Outcomes Research and Education. RedUSe project. 2016. http://www.utas.edu.au/umore/assets/research/health-informatics/2008/reduse. Accessed 24 AprIL 2017.
Leung B, Jokanovic N, Tan EC, et al. Prescribed doses of opioids in long-term care facilities. J Am Med Dir Assoc. 2015;16(12):1100–2.
Australian Institute of Health and Welfare, Bradley C. Hospitalisations due to falls by older people, Australia 2009–2010. Canberra: Australian Institute of Health and Welfare; 2013.
Rubenstein LZ, Josephson KR. The epidemiology of falls and syncope. Clin Geriatr Med. 2002;18(2):141–58.
Ricci F, Manzoli L, Sutton R, et al. Hospital admissions for orthostatic hypotension and syncope in later life: insights from the Malmö preventive project. J Hypertens. 2017;35(4):776–83.
Sun BC, Emond JA, Camargo CA Jr. Direct medical costs of syncope-related hospitalizations in the United States. Am J Cardiol. 2005;95(5):668–71.
Cherubini A, Eusebi P, Dell’Aquila G, et al. Predictors of hospitalization in Italian nursing home residents: the U.L.I.S.S.E. project. J Am Med Dir Assoc. 2012;13(1):84.e5–10.
Lalic S, Sluggett JK, Ilomaki J, et al. Polypharmacy and medication regimen complexity as risk factors for hospitalization among residents of long-term care facilities: a prospective cohort study. J Am Med Dir Assoc. 2016;17(11):1067.e1–6.
Turner JP, Jamsen KM, Shakib S, et al. Polypharmacy cut-points in older people with cancer: How many medications are too many? Support Care Cancer. 2016;24(4):1831–40.
Wimmer BC, Bell JS, Fastbom J, et al. Medication regimen complexity and number of medications as factors associated with unplanned hospitalizations in older people: a population-based cohort study. J Gerontol A Biol Sci Med Sci. 2016;71(6):831–7.
Berry SD, Mittleman MA, Zhang Y, et al. New loop diuretic prescriptions may be an acute risk factor for falls in the nursing home. Pharmacoepidemiol Drug Saf. 2012;21(5):560–3.
Acknowledgements
The authors would like to thank Jessica Bailey and Grace Wan for their assistance with data management.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The authors gratefully acknowledge the Ageing and Aged Care Branch, Department of Health and Human Services, State Government of Victoria, for commissioning and funding this research. Jenni Ilomäki was supported by a National Health and Medical Council Early Career Fellowship.
Conflicts of interest
Taliesin Ryan-Atwood, Mieke Hutchinson-Kern, Jenni Ilomäki, Michael Dooley, Susan Poole, Carl Kirkpatrick, Elizabeth Manias, Biswadev Mitra and Simon Bell declare that they have no conflicts of interest relevant to the content of this study.
Rights and permissions
About this article
Cite this article
Ryan-Atwood, T.E., Hutchinson-Kern, M., Ilomäki, J. et al. Medication Use and Fall-Related Hospital Admissions from Long-Term Care Facilities: A Hospital-Based Case–Control Study. Drugs Aging 34, 625–633 (2017). https://doi.org/10.1007/s40266-017-0472-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40266-017-0472-8