Abstract
Introduction
Data are still lacking about the use of terlipressin or vasopressin in the treatment of pediatric patients who are in a state of therapy-refractory shock.
Objective
The aim of this study was to evaluate the effect of terlipressin on hemodynamics in children with distributive shock and to describe any severe side effects.
Methods
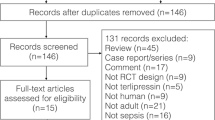
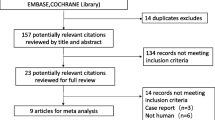
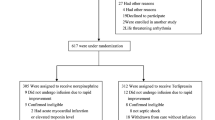
Consecutive patients (n = 20) with catecholamine-resistant distributive shock who were treated with terlipressin were retrospectively enrolled in this study. We analyzed response in terms of mean arterial blood pressure, heart rate, vasoactive inotropic score (VIS), urinary output, and serum lactate.
Results
The hemodynamics of 12 children significantly improved within 6 h of commencing terlipressin (mean blood pressure increase of ≥20 % without VIS increase, or mean blood pressure increase of ≥10 % with VIS decrease of ≥10 %). The hemodynamics of eight patients did not improve, regardless of treatment dosage or duration. More children died in the responders group (n = 7 [58.3 %]) than in the non-responders group (n = 2 [25.0 %]), but this was not statistically significant. Two patients (one in each group) who received high dosages of terlipressin developed rhabdomyolysis. One case of Takotsubo cardiomyopathy was observed, which could be related to terlipressin.
Conclusions
Although treatment with terlipressin resulted in rapid positive hemodynamic responses in some children, it did not seem to have a positive effect in other pediatric patients. Therefore, the possible benefits of terlipressin should be always weighed against potential severe adverse effects.

Similar content being viewed by others
References
Matok I, Leibovitch L, Vardi A, et al. Terlipressin as rescue therapy for intractable hypotension during neonatal septic shock. Pediatr Crit Care Med. 2004;5(2):116–8.
Rodriguez-Nunez A, Fernandez-Sanmartin M, Martinon-Torres F, et al. Terlipressin for catecholamine-resistant septic shock in children. Intensive Care Med. 2004;30(3):477–80. doi:10.1007/s00134-003-2114-3.
Zeballos G, Lopez-Herce J, Fernandez C, et al. Rescue therapy with terlipressin by continuous infusion in a child with catecholamine-resistant septic shock. Resuscitation. 2006;68(1):151–3. doi:10.1016/j.resuscitation.2005.06.016.
Filippi L, Gozzini E, Daniotti M, et al. Rescue treatment with terlipressin in different scenarios of refractory hypotension in newborns and infants. Pediatr Crit Care Med. 2011;12(6):e237–41. doi:10.1097/PCC.0b013e3181fe304c.
Jerath N, Frndova H, McCrindle BW, et al. Clinical impact of vasopressin infusion on hemodynamics, liver and renal function in pediatric patients. Intensive Care Med. 2008;34(7):1274–80. doi:10.1007/s00134-008-1055-2.
Masutani S, Senzaki H, Ishido H, et al. Vasopressin in the treatment of vasodilatory shock in children. Pediatr Int. 2005;47(2):132–6. doi:10.1111/j.1442-200x.2005.02043.x.
Matok I, Vard A, Efrati O, et al. Terlipressin as rescue therapy for intractable hypotension due to septic shock in children. Shock. 2005;23(4):305–10.
Rodriguez-Nunez A, Oulego-Erroz I, Gil-Anton J, et al. Continuous terlipressin infusion as rescue treatment in a case series of children with refractory septic shock. Ann Pharmacother. 2010;44(10):1545–53. doi:10.1345/aph.1P254.
Agrawal A, Singh VK, Varma A, et al. Intravenous arginine vasopressin infusion in refractory vasodilatory shock: a clinical study. Indian J Pediatr. 2012;79(4):488–93. doi:10.1007/s12098-011-0557-z.
Albanese J, Leone M, Delmas A, et al. Terlipressin or norepinephrine in hyperdynamic septic shock: a prospective, randomized study. Crit Care Med. 2005;33(9):1897–902.
Rodriguez-Nunez A, Lopez-Herce J, Gil-Anton J, et al. Rescue treatment with terlipressin in children with refractory septic shock: a clinical study. Crit Care. 2006;10(1):R20. doi:10.1186/cc3984.
Yildizdas D, Yapicioglu H, Celik U, et al. Terlipressin as a rescue therapy for catecholamine-resistant septic shock in children. Intensive Care Med. 2008;34(3):511–7. doi:10.1007/s00134-007-0971-x.
Choong K, Bohn D, Fraser DD, et al. Vasopressin in pediatric vasodilatory shock: a multicenter randomized controlled trial. Am J Respir Crit Care Med. 2009;180(7):632–9. doi:10.1164/rccm.200902-0221OC.
Leone M, Albanese J, Delmas A, et al. Terlipressin in catecholamine-resistant septic shock patients. Shock. 2004;22(4):314–9.
Morelli A, Rocco M, Conti G, et al. Effects of terlipressin on systemic and regional haemodynamics in catecholamine-treated hyperkinetic septic shock. Intensive Care Med. 2004;30(4):597–604. doi:10.1007/s00134-003-2094-3.
O’Brien A, Clapp L, Singer M. Terlipressin for norepinephrine-resistant septic shock. Lancet. 2002;359(9313):1209–10. doi:10.1016/S0140-6736(02)08225-9.
Westphal M, Stubbe H, Sielenkamper AW, et al. Terlipressin dose response in healthy and endotoxemic sheep: impact on cardiopulmonary performance and global oxygen transport. Intensive Care Med. 2003;29(2):301–8. doi:10.1007/s00134-002-1546-5.
Agrawal A, Singh VK, Varma A, et al. Therapeutic applications of vasopressin in pediatric patients. Indian Pediatr. 2012;49(4):297–305.
Delmas A, Leone M, Rousseau S, et al. Clinical review: vasopressin and terlipressin in septic shock patients. Crit Care. 2005;9(2):212–22. doi:10.1186/cc2945.
Leone M, Martin C. Rescue therapy in septic shock—is terlipressin the last frontier? Crit Care. 2006;10(2):131. doi:10.1186/cc4863.
Leone M, Martin C. Role of terlipressin in the treatment of infants and neonates with catecholamine-resistant septic shock. Best Pract Res Clin Anaesthesiol. 2008;22(2):323–33.
Meyer S, McGuire W, Gottschling S, et al. The role of vasopressin and terlipressin in catecholamine-resistant shock and cardio-circulatory arrest in children: review of the literature. Wien Med Wochenschr. 2011;161(7–8):192–203. doi:10.1007/s10354-010-0853-7.
Polito A, Parisini E, Ricci Z, et al. Vasopressin for treatment of vasodilatory shock: an ESICM systematic review and meta-analysis. Intensive Care Med. 2012;38(1):9–19. doi:10.1007/s00134-011-2407-x.
Shivanna B, Rios D, Rossano J, et al. Vasopressin and its analogues for the treatment of refractory hypotension in neonates. Cochrane Database Syst Rev. 2013;3:CD009171. doi:10.1002/14651858.CD009171.pub2.
Neunhoeffer F, Renk H, Hofbeck M, et al. Safety, efficacy and response to a hydrocortisone rescue therapy protocol in children with refractory hypotension after cardiopulmonal bypass. Pediatr Cardiol. 2015;36(3):640–5. doi:10.1007/s00246-014-1059-3.
Graciano AL, Balko JA, Rahn DS, et al. The Pediatric Multiple Organ Dysfunction Score (P-MODS): development and validation of an objective scale to measure the severity of multiple organ dysfunction in critically ill children. Crit Care Med. 2005;33(7):1484–91.
Akcan-Arikan A, Zappitelli M, Loftis LL, et al. Modified RIFLE criteria in critically ill children with acute kidney injury. Kidney Int. 2007;71(10):1028–35. doi:10.1038/sj.ki.5002231.
Pierce ST, Nickl N. Rhabdomyolysis associated with the use of intravenous vasopressin. Am J Gastroenterol. 1993;88(3):424–7.
Rolla D, Cannella G, Ravetti JL. Toxic rhabdomyolysis induced by terlipressin infusion in a uraemic patient suffering from AA-type amyloidosis. Nephron. 1999;83(2):167–8. doi:10.1159/000045496.
Zimmer V, Lammert F. Terlipressin-induced skin necrosis and rhabdomyolysis. Am J Med Sci. 2010;340(6):506. doi:10.1097/MAJ.0b013e3181ee9873.
Hernandez LE. Takotsubo cardiomyopathy: how much do we know of this syndrome in children and young adults? Cardiol Young. 2014;24(4):580–92. doi:10.1017/S1047951114000080.
Di Micoli A, Buccione D, Degli Esposti D, et al. Terlipressin infusion induces Tako-Tsubo syndrome in a cirrhotic man with hepato-renal syndrome. Intern Emerg Med. 2011;6(5):437–40. doi:10.1007/s11739-011-0534-6.
Lu YY, Wei KC, Wu CS. Terlipressin-induced extensive skin necrosis: a case report and published work review. J Dermatol. 2012;39(10):866–8. doi:10.1111/j.1346-8138.2012.01595.x.
Ozel Coskun BD, Karaman A, Gorkem H, et al. Terlipressin-induced ischemic skin necrosis: a rare association. Am J Case Rep. 2014;15:476–9. doi:10.12659/AJCR.891084.
Sundriyal D, Kumar N, Patnaik I, et al. Terlipressin induced ischaemia of skin. BMJ Case Rep. 2013. doi:10.1136/bcr-2013-010050.
Donnellan F, Cullen G, Hegarty JE, et al. Ischaemic complications of Glypressin in liver disease: a case series. Br J Clin Pharmacol. 2007;64(4):550–2. doi:10.1111/j.1365-2125.2007.02921.x.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Approval
The study protocol was approved by the Ethics Committee of Tuebingen University Hospital, Germany (189/2013R).
Funding
No funding was received for the conduct of this study.
Conflict of interest
Jörg Michel, Michael Hofbeck, Gina Spiller, Hanna Renk, Matthias Kumpf, and Felix Neunhoeffer have no conflicts of interest that might be relevant to the contents of this manuscript.
Rights and permissions
About this article
Cite this article
Michel, J., Hofbeck, M., Spiller, G. et al. Safety and Efficacy of Terlipressin in Pediatric Distributive Shock: A Retrospective Analysis in 20 Children. Pediatr Drugs 19, 35–41 (2017). https://doi.org/10.1007/s40272-016-0199-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40272-016-0199-8